Benefit of Active Approach to Surveillance of Hospital-Acquired Infections
Received: 17-Mar-2016 / Accepted Date: 14-Apr-2016 / Published Date: 21-Apr-2016 DOI: 10.4172/2161-1165.1000239
Abstract
Background: In Slovakia the most usual approach to the prevention and control of hospital-acquired infections is passive surveillance, which typically leads to of under-reporting. The resulting lack of information means there is insufficient support for effective measures to tackle preventable hospital-acquired infections. Uncontrolled incidence has a negative impact on health care outcomes as well as being a burden for the management of institutional health care. The aim of this study was to demonstrate the benefits of active approach to surveillance for more efficient identification of hospital-acquired infections and, in respect of multidrug-resistant organisms, to determine the relation to the average treatment time and to clarify the impact on hospital budgets of treating patients for such infections.
Methods: Monitoring was carried out in the form of surveillance. Diagnostic criteria for detecting infection were prepared in accordance with available protocols, and were incorporated into hospital procedures for the diagnosis of hospital-acquired infections. Information was drawn from the database of the laboratory information system FONSOpenlims and patients’ medical records. Data was collected by the hospital epidemiologist and subsequently hospital-acquired infections were diagnosed by the treating physician. The incidence of infections was reported to the Regional Public Health Authority.
Results: Monitoring identified 65 hospital-acquired infections, representing an incidence of 1.57%. Hospitalacquired infections prolonged hospitalisation time by an average of 9.6 days according to the monitoring of the relation of infections to the average time of treatment. It was shown that the cost of treating hospital-acquired infections exceeds payments from the health insurers.
Conclusion: The study provided an overview of the incidence of infections caused by multidrug-resistant organisms in hospitals and led to a series of measures in the implementation and monitoring of best practices for sanitary epidemiological regime. The costs for the diagnosis and treatment of infections promoted the merits of prospective active approach to surveillance of hospital-acquired infections.
Keywords: Financial costs; Hospital-acquired infections; Multidrugresistant organisms; Protocols; Surveillance
Introduction
Hospital infections are one of the most frequent complications of hospitalisation. They increase morbidity and mortality in patients. They also prolong patients’ hospitalisation and require extensive diagnosis and treatment, which significantly increases costs [1]. They are significant adverse events in healthcare provision [2]. Effective hospital programs for infection control are based on surveillance to identify trends in the incidence of hospital-acquired infections (HAIs), environmental factors as well as practical risks affecting their incidence [3].
Surveillance is defined as “the ongoing, systematic collection, analysis and interpretation of health data essential to the planning, implementation, and evaluation of public health practice, closely integrated with the timely dissemination of these data to those who need to know” [3,4]. Active surveillance has been used successfully to control infections in hospitals. Passive surveillance involving the reporting of infections by physicians is considered to be complementary [5,6].
Clinical staff primarily focuses their skills and knowledge on immediate treatment needs, whereas the control and prevention of HAIs requires the development of specific knowledge and skills by a dedicated team of specialists. It is not surprising that passive surveillance leads to the erroneous classification or the inadequate and delayed or negative reporting of HAIs.
The Law of Slovak Republic, Act No 355/2007 on the Protection, Support and Development of Public Health and amending certain acts, as amended, lays down obligations for healthcare providers and clinical staff in relation to the prevention and control of HAIs [7].
The management of a health care institution is responsible for the control and prevention of HAIs, including the funding of this activity. Costs for the control and prevention of HAIs are not taken into account in payments from insurance companies. A consequence of this is that the predominant form of monitoring for HAIs in Slovak healthcare facilities is passive surveillance, which detects HAI incidence in the range 0.5-1.0% [8].
Hospitals have the opportunity to participate voluntarily in projects on HAIs organized by the national contact person for the European Centre for Disease Prevention and Control (ECDC).
However, such projects allow only retrospective monitoring of the incidence of HAIs. The hospital receives information on the incidence of individual types of infections but usually when it is too late to take measures to control the situation.
Materials and Methods
Before the study, protocols were prepared, verified and put into practice which established working definitions of HAIs, reporting procedures, responsible persons and the method of checking reports. The protocols were incorporated into the Quality Management System (QMS) documentation for the hospital.
The results of the microbiological examination of biological material of patients admitted to the hospital provided baseline information for surveillance of HAIs. The bacterial agents with clinically and epidemiologically important mechanisms of resistance to antibiotics were monitored.
Multidrug-resistant organisms (MDROs) included carbapenemaseproducing bacteria, extended-spectrum β-lactamases (ESBLs), AmpCtype β-lactamases in plasma, carbapenem-resistant enterobacteriaceae, methicillin-resistant Staphylococcus aureus (MRSA) and vancomycinresistant enterococci (VRE) [9].
Information about MDROs was drawn from the database of laboratory information system FONSOpenlims (Openlims). Clinical information on the course of infection with MDROs aetiology was obtained from patients’ medical records. The monitoring was performed in Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia in the period of 6 months (from 1st January 2012 to 30th June 2012). In the monitored period, Faculty Hospital with Polyclinic Skalica, joint stock company had 314 of beds.
The healthcare provision was carried out at the following Departments (Dept.): Dept. of Internal Medicine including Cardiology Intensive Care Unit, Dept. of Neurology, Dept. of Surgery, Dept. of Urology, Dept. of Orthopedics, Dept. of Otorhinolaryngology, Dept. of Pediatrics, Dept. of Neonatology, Dept. of Obstetrics and Gynecology and Dept. of Anesthesiology and Intensive Care Medicine (AIC). Monitoring was carried out only in those departments where the incidence of MDROs was recorded. MDROs in colonized patients were excluded from monitoring.
A working diagnosis of an HAI was made based on the criteria laid down in the protocol for the diagnosis of HAI. A potential identification of an HAI in a patient was submitted to their treating physician for assessment. Diagnosed HAIs were included in monitoring and subsequently reported to Regional Public Health Authority.
The calculation of the costs associated with prolonged hospitalization due to HAI was based on the actual average costs per day of treatment in the relevant department and compared with the average payment (all health insurance companies) for a hospital discharge. The average real costs were based on total costs i.e., fixed costs and treatment costs.
Limitations of monitoring were that surveillance of HAIs was carried out only on patients with findings of MDROs and there were also some deficiencies in the management of medical records. The data obtained through surveillance was analysed in Excel and XLSTAT.
Results
In the monitored period, 4 247.5 patients were hospitalized and their hospitalisation required 23 828 treatment days. A total of 10 115 samples of clinical material taken from 4 248 patients underwent microbiological examination. Out of the total number of samples, indications of MDROs were found in 456 isolates, which represented a share of 4.5%.
The calculation of the number of hospitalizations was based on the requirements of National Health Information Center (NHIC) which counts the number of hospitalized patients as follows: for the hospital (admitted patients + discharged patients + dead patients): 2 [10].
Detected HAIs
In total, the study found and confirmed 65 HAIs, representing an incidence rate of 1.57% of hospitalized patients. The density of incidence was 1.93/1 000 treatment days. The highest incidences, 3.82% and 2.73% of hospitalized patients, were reported in the Department of Internal Medicine and in the Department of Anaesthesiology and Intensive Care Medicine (Table 1).
| Departments | Hospital-acquired infections | Incidence (%) | Density of incidence / 1000 treatment days | Patients Resistant strains | Resistant strains | Resistant strains % | Number of samplings | Number of hospitalized patients | Treatment days |
|---|---|---|---|---|---|---|---|---|---|
| Internal Medicine | 41 | 3.82 | 4.8 | 80 | 292 | 7.6 | 3839 | 1074.5 | 8600 |
| Surgery | 12 | 1.37 | 2.87 | 40 | 43 | 4.5 | 950 | 878.5 | 4533 |
| Urology | 3 | 0.47 | 0.81 | 18 | 43 | 3.5 | 1213 | 632 | 3691 |
| Orthopaedics | 1 | 0.25 | 0.52 | 2 | 4 | 2.4 | 166 | 390.5 | 1918 |
| AIC | 4 | 2.73 | 9.09 | 23 | 65 | 5.6 | 1157 | 146.5 | 440 |
| Paediatrics | 1 | 0.13 | 0.35 | 6 | 8 | 0.3 | 2468 | 759 | 2845 |
| Neonatology | 3 | 0.82 | 2.77 | 1 | 1 | 0.3 | 322 | 366.5 | 1801 |
| Total | 65 | 1.57 | 2.81 | 169 | 456 | 4.5 | 10115 | 4 247.5* | 23828 |
Table 1: Overview of the hospital-acquired infections detected by surveillance over the period of 6 months (Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia; 1st January 2012 - 30th June 2012). AIC-Anaesthesiology and Intensive Care Medicine. *Calculated according to National Health Information Center [10].
Incidence of resistant strains
Of the total of 10115 samples taken from 4248 patients, 456 samples of MDROs were isolated and MRDOs developed in 169 patients. The clinical manifestation was reflected in 38.5% of infected patients. Of the total number of examined samples, the largest proportion of MDRO strains, 7.6%, was recorded in the Department of Internal Medicine. MDROs strains were present in 80 of 1075 hospitalized patients and an HAI manifested in every second colonized patient. In the Department of AIC, an average 8 samples of biological material were taken per patient and MDROs were detected in 5.6% of samples. Out of a total of 147 hospitalized patients, 23 patients (15.6%) were colonized with MDROs and 4 patients fell ill, representing the incidence of 2.73% and a density of incidence of 9.09/1000 treatment days.
Clinical manifestation
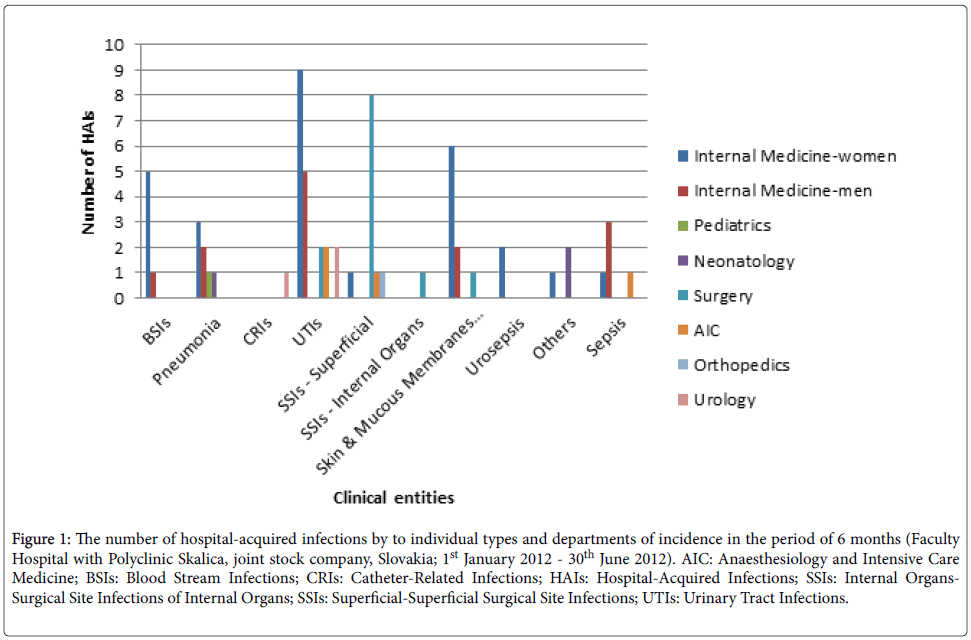
Infection caused by MDROs was most likely to affect the urinary tract (30.8% of cases; 33.9% including urosepsis). Surgical site infections (SSIs) were affected in 18.5% of cases. The surface of the skin and mucous membranes were attacked by 13.8% of infections, mainly in the form of infected pressure ulcers. Pneumonia was diagnosed in 10.8% of the total number of HAIs. Bloodstream infections (BSIs) including sepsis represented 16.9% of cases. Sepsis accounted for 7.7% of incidence. Catheter-related infections (CRIs) occurred in 1.5%. Other infections included conjunctivitis and sinusitis (4.6%)
The number of hospital-acquired infections by to individual types and departments of incidence represents Figure 1.
Figure 1: The number of hospital-acquired infections by to individual types and departments of incidence in the period of 6 months (Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia; 1st January 2012 - 30th June 2012). AIC: Anaesthesiology and Intensive Care Medicine; BSIs: Blood Stream Infections; CRIs: Catheter-Related Infections; HAIs: Hospital-Acquired Infections; SSIs: Internal Organs-Surgical Site Infections of Internal Organs; SSIs: Superficial-Superficial Surgical Site Infections; UTIs: Urinary Tract Infections.
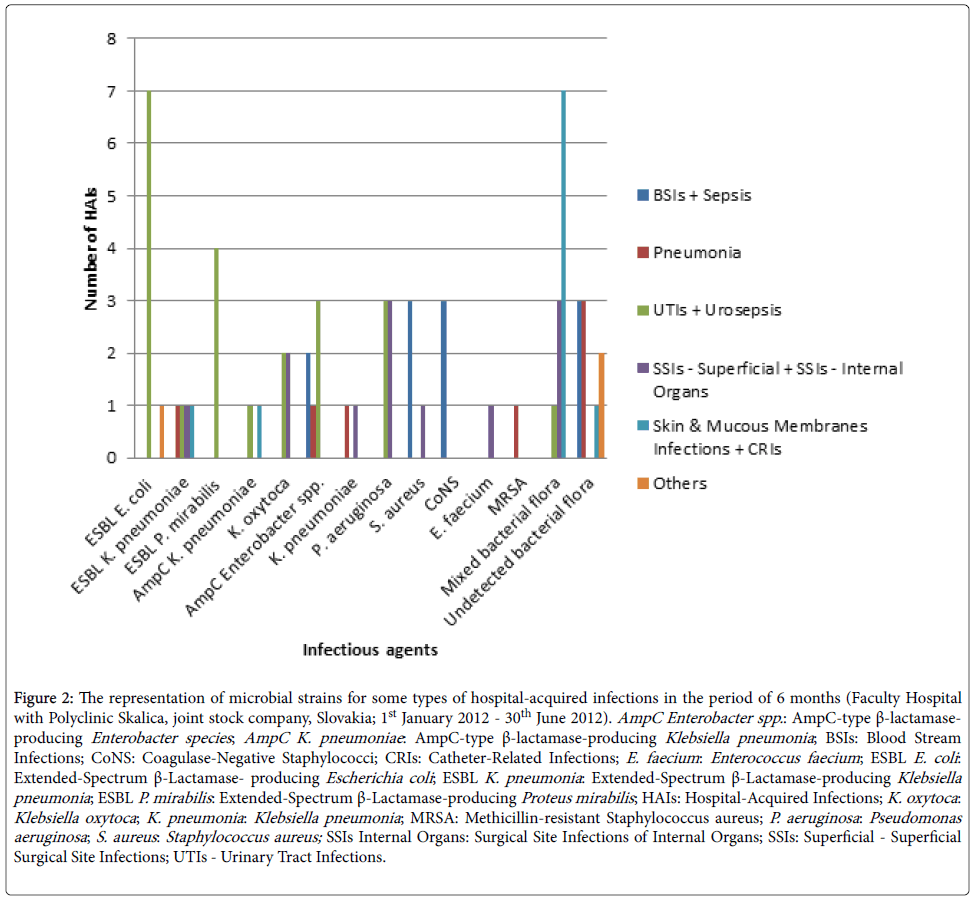
Infectious agents
The main infectious agents of the urinary tract were extendedspectrum β-lactamase- producing Escherichia coli (ESBL E. coli ), extended-spectrum β-lactamase-producing Proteus mirabilis (ESBL P. mirabilis ), AmpC-type β-lactamase-producing Enterobacter species (AmpC Enterobacter spp. ) and Pseudomonas aeruginosa (P. aeruginosa ).
Klebsiella pneumoniae (K. pneumoniae ), Klebsiella oxytoca (K. oxytoca ), extended-spectrum β-lactamase-producing Klebsiella pneumoniae (ESBL K. pneumoniae ), P. aeruginosa , Staphylococcus aureus (S. aureus ), Enterococcus faecium and mixed flora, including Gram negative and Gram positive bacteria were the causes of SSIs. ESBL K. pneumoniae , AmpC-type β-lactamase-producing Klebsiella pneumoniae (AmpC K. pneumoniae ) and a mixed flora including Gram positive and Gram negative bacteria, participated in the infections of the skin and mucous membranes. The infectious agents in BSIs including sepsis were coagulasenegative staphylococci (CoNS), S. aureus and AmpC Enterobacter spp. Diagnostics of clinical ongoing pneumonia was established on microbiological examination of sputum with findings of ESBL K. pneumoniae , K. pneumoniae and AmpC Enterobacter spp. (Figure 2).
Figure 2: The representation of microbial strains for some types of hospital-acquired infections in the period of 6 months (Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia; 1st January 2012 - 30th June 2012). AmpC Enterobacter spp.: AmpC-type β-lactamaseproducing Enterobacter species; AmpC K. pneumoniae : AmpC-type β-lactamase-producing Klebsiella pneumonia ; BSIs: Blood Stream Infections; CoNS: Coagulase-Negative Staphylococci; CRIs: Catheter-Related Infections; E. faecium : Enterococcus faecium ; ESBL E. coli : Extended-Spectrum β-Lactamase- producing Escherichia coli ; ESBL K. pneumonia : Extended-Spectrum β-Lactamase-producing Klebsiella pneumonia ; ESBL P. mirabilis : Extended-Spectrum β-Lactamase-producing Proteus mirabilis ; HAIs: Hospital-Acquired Infections; K. oxytoca : Klebsiella oxytoca ; K. pneumonia : Klebsiella pneumonia ; MRSA: Methicillin-resistant Staphylococcus aureus; P. aeruginosa : Pseudomonas aeruginosa ; S. aureus : Staphylococcus aureus; SSIs Internal Organs: Surgical Site Infections of Internal Organs; SSIs: Superficial - Superficial Surgical Site Infections; UTIs - Urinary Tract Infections.
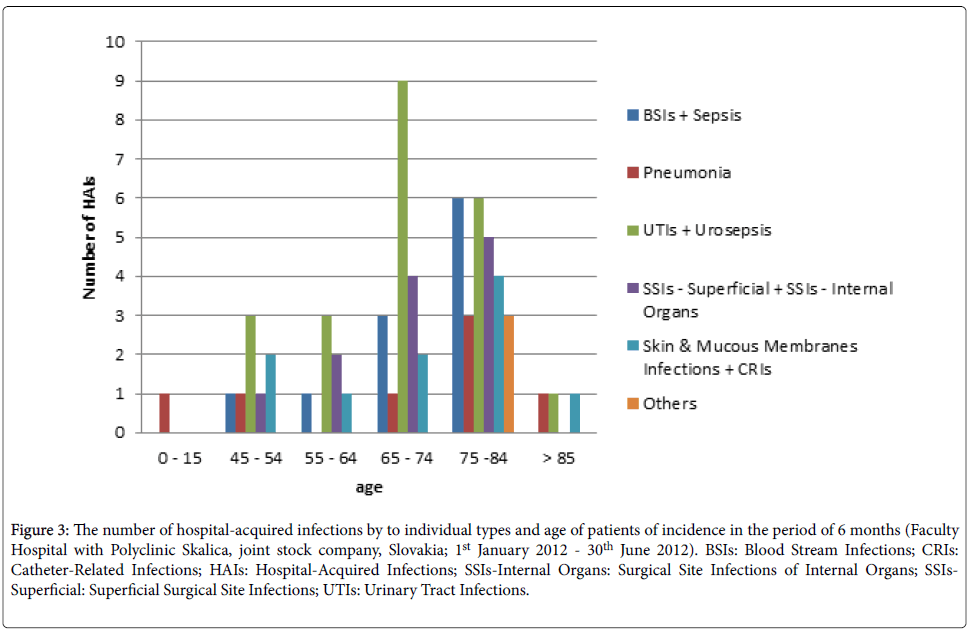
Age of patients
In the study, the highest number of hospital-acquired infections was in the patients of ages from 65 to 84 years. In the age groups from 65 to 74 years were the most represented urinary tract infections (UTIs) including urosepsis and from 75 to 84 years UTIs including urosepsis as well as BSIs including sepsis (Figure 3).
Figure 3: The number of hospital-acquired infections by to individual types and age of patients of incidence in the period of 6 months (Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia; 1st January 2012 - 30th June 2012). BSIs: Blood Stream Infections; CRIs: Catheter-Related Infections; HAIs: Hospital-Acquired Infections; SSIs-Internal Organs: Surgical Site Infections of Internal Organs; SSIs-Superficial: Superficial Surgical Site Infections; UTIs: Urinary Tract Infections.
Length of hospitalization
During the six months of the study in the hospital, the average length of treatment for patients with HAIs was 20.4 days; the median length of treatment was 17 days (CI 95% 17.2, 23.6).
The length of hospitalization of a patient with an infection was prolonged by an average of 9.6 days (CI 95%7.5, 11.8), with the median being 7 days and the average length of treatment being 5.57 days (CI 95% 5.4, 5.74).
Costs
The overall average daily cost of treatment was €227.85. When a patient’s hospital stay was prolonged due to an HAI for on average 9.6 days, the additional costs would be €2187.40.
For one complete hospitalization, the hospital received an average of €818.30 from health insurance companies.
The total financial resources spent on treatment of HAIs detected by surveillance amounted to €142 184.00 over the half year (Table 2), which is 17.5% of the total costs incurred for providing healthcare in the monitored departments.
| Departments | Detected hospital- acquired infections | Expected hospital- acquired infections | Detected vs. expected hospital-acquired infections % | Costs per 1 day of treatment € / 2012 | Costs of 1 hospital- acquired infection € / 2012 | Total cost of hospital-acquired infections € / 2012 | Total cost of hospital-acquired infections € / 2012 |
|---|---|---|---|---|---|---|---|
| Internal Medicine | 41 | 43 | 95.3 | 60.88 | 642.05 | 26323.97 | 490 |
| Surgery | 12 | 35 | 34.3 | 98.14 | 942.15 | 11305.73 | 587 |
| Urology | 3 | 25 | 12 | 74.65 | 716.64 | 2149.92 | 545 |
| Orthopaedics | 1 | 16 | 6.2 | 252.89 | 2 427.74 | 2427.74 | 767 |
| AIC | 4 | 6 | 66.6 | 983.2 | 9 436.80 | 37747.20 | 2541.00 |
| Paediatrics | 1 | 30 | 3.3 | 72.62 | 697.15 | 697.15 | 458 |
| Neonatology | 2 | 15 | 13.3 | 52.59 | 504.86 | 1009.72 | 340 |
| Total | 65 | 170 | 38.2 | 227.85 | 2 187.40 | 142184.00 | 818.3 |
Table 2: The costs of treatment of hospital-acquired infections over a period of 6 months (Faculty Hospital with Polyclinic Skalica, joint stock company, Slovakia; 1st January 2012 - 30th June 2012). AIC - Anaesthesiology and Intensive Care Medicine.
Discussion
In our surveillance study, we have found that HAIs caused by MDROs had an incidence 1.57%. Because we had no information on the incidence of HAIs in the previous period, we used for comparison the available information on the prevalence of HAIs from the Point Prevalence Study (PPS) performed in Slovakia in the year 2012. In the hospital the prevalence within the PPS was 4% (CI 95% 1.5, 8.6) [11].
If we assume that in the hospital in the first half of 2012 4% of patients acquired an infection, it represents an incidence of 170 HAIs of hospitalized patients. The HAIs detected by surveillance (65 HAIs) accounted for 38.2% of the number of expected infections.
The potential for comparing the results of our monitoring with the data from international studies is limited by the study size and the restricted focus on HAIs caused by MDROs. Nevertheless, it is noteworthy that the most common infections in terms of their localisation were UTIs and SSIs.
Compared with the results of PPS, in our monitoring infections of the skin and mucous membranes with the prevalence of infected pressure ulcers (90%) were found more often (13.8%) in the Department of Internal Medicine.
Urinary tract infections
Of the total number of infections detected by surveillance, UTIs made up 30.8%. The National surveillance system in Hungary, which focuses on epidemiologically serious MDROs, reports a 9.6% share for UTIs. This result is affected by the structure of hospitals involved in the reporting, where surgical departments oriented on monitoring for SSIs are predominant [12]. UTIs of all pathogen types make up 19% of HAIs for European hospitals [13] and 26% in Slovak Republic [11].
A comparison with data from the Department of Health and Human Services USA is impossible, since only UTIs associated with the introduction of urinary catheter are reported in this system [14,15].
In our group of UTIs Gram negative bacteria were most commonly isolated, with prevalence of the bacterial strain culture (80%). ESBL E. coli (30%) and ESBL P. mirabilis (20%) were the most common. As the etiological agents, AmpC Enterobacter spp. and carbapenem-resistant Pseudomonas aeruginosa each accounted for 15%. A similar spectrum of urinary infection agents was recorded in Hungary between 2005 and 2010 [12].
In our study, the UTIs caused by Gram negative bacteria reached the highest incidence of the monitored HAIs. The best practices were incorporated into standard procedures for the introduction and care of urinary catheters [16]. Other measures promoted compliance with the disinfection programme and staff training on disinfection, including hand hygiene.
Surgical site infections
SSIs were the second most common HAI with an incidence 18.5%. Superficial SSIs had an incidence of 16.9% and SSIs of internal organs 1.5% of all infections. The German surveillance system, Krankenhaus- Infektion-Surveillance-system (KISS), which focuses on selected MDROs (MRSA and Clostridium difficile ), recorded a 15.8% share for SSIs [1].
Pathogens of internal organs related to surgical intervention included Gram negative bacteria with prevalence of carbapenemresistant P. aeruginosa (25%). Microbiological examination of superficial surgical wounds confirmed the presence of mixed flora, including Gram negative and Gram positive bacteria. Monitoring of SSIs depends on the type of operation and this limits the conclusions and comparisons that can be based on the data [17].
Despite the fact that the number of detected SSIs is consistent with the findings of the European and American studies, there is no room for complacency and these infections demand a response. It is particularly noteworthy that two thirds of the 12 infections identified by surveillance in the Department of Surgery were SSIs. In the future it will be necessary to carry out monitoring of SSIs in relation to the type of surgical intervention. Because Gram negative bacteria were the predominant pathogens in the monitored group, attention will focus mainly on operations of the digestive tract. Preventative measures will include preoperative monitoring, prophylactic administration of antibiotics and patient care in the postoperative period.
Infections of the skin and mucous membranes
Infections of the skin and mucous membranes made up 13.8% of cases, almost 90% of which were infections of pressure ulcers in the Department of Internal Medicine. PPS recorded a 20.2% share of pressure ulcers in the total number of skin and mucous membranes infections. ESBL K. pneumoniae , AmpC K. pneumoniae and a mixed flora including Gram positive and Gram negative bacteria participated in these infections.
The incidence of infections of pressure ulcers was the subject of an epidemiological investigation which showed weaknesses especially in nursing care and barrier regimen in the treatment of patients diagnosed with multidrug-resistant strains.
Blood stream infections
In European hospitals, BSIs make up 10.6% of HAIs [13]. In the Hungarian study of multi-resistant strains, BSIs occurred in 9.7% of cases [12]. In the USA, BSIs accounted for 14% of all types of HAIs [14]. In our monitoring, 16.9% of infections in the Department of Internal Medicine were BSIs, including sepsis. Incorrect management of central and peripheral venous catheters during their introduction was one of the causes of these infections.
To address the incidence of BSIs best practices were incorporated into standard procedures for the introduction of medical devices into the bloodstream and for care in the management of exchange [16].
Pneumonia
Pneumonia made up 10.8% of the total number of HAI diagnoses. In European hospitals the share of pneumonia was 19.4% [13] and in the USA 13% of the total number of infections [14]. The diagnosis of pneumonia was based only on microbiological examination of sputum; therefore, comparison with the data in the literature was not possible.
Monitoring of costs
HAIs prolonged hospitalisation time of about 9.6 days. Of one complete hospitalization, the hospital received €818.30 from health insurance companies on average. Overall average daily treatment costs were €227.85. In the monitored period, payments received from health insurance companies reflected the average costs for a patient hospitalisation lasting 3.5 days.
Extra costs spent on treatment of HAIs amounted to €142 184.00, representing 17.5% of the total costs for inpatients. The costs of 1 hospital-acquired infection were €2 187.40 which represented the benefit, how much money the active approach to surveillance could save, in the case of our study.
The calculations were made of the actual prices for the hospital discharge in 2012.
Conclusion
The study provided an overview of the incidence of infections caused by MDROs in hospital conditions. The results led to the introduction of a uniform disinfection program, protocols on the implementation of the central and peripheral venous catheters and protocols for the diagnosis of HAIs.
A form for reporting HAIs was added to the National Information System (NIS) to improve the flow of information between treating physicians and hospital epidemiologist.
The calculation of costs incurred for diagnosis and treatment in hospital and their share of the total costs supported the rationale for active approach to surveillance as well as prevention measures, including additional best practices incorporated into standard procedures in trained staff, in Nurse, in Physician educational curriculum and in sanitary epidemiological practice.
References
- GeffersCh, Gastmeier P (2011) Nosocomial Infections and Multidrug-resistant Organisms epidemiological data from KISS. DtschArztebl Int. 108: 87-93.
- (2009) Report to the Council on the basis of Member States relating to the implementation of the Council Recommendation on patient safety, including the prevention and control of healthcare associated infections.
- Allen-Bridson K, Morrell GC, Horan TC (2012) Surveillance of healthcare-associated infections: Hospital epidemiology and infection control (4th edn.) Philadelphia, Wolters Kluwer.
- Klement C, Mezencev RFN (2016) Slovak-English terminology glossary, A - Z.: Slovak-English terminology of public health I (1st edn.) BanskáBystrica, joint stock company, Slovakia.
- Nettleman MD, Roach RL, Wenzel RP (2011) Principles of healthcare epidemiology: Hospital epidemiology and infection control (4th edn.)Lippincott William & Wilkins, Wolters Kluwer, Philadelphia.
- Beneden CV, Olsen SJ, Skoff T, Lynfield R (2007) Population-based, active surveillance for emerging infectious diseases: Infectious Disease Surveillance, United Kingdom, Blackwell Publishing.
- (2007) Support and Development of Public Health and on the Amendment and Supplement to Selected Laws as amended by later regulations.
- (2012) Analysis of epidemiological situation and No. activity epidemiology department In Slovak republic.
- The Ministry of Health of the Slovak Republic (2014) Professional guideline for the diagnosis and anti-epidemic measures in the incidence of bacterial infectious agents with clinically and epidemiologically important mechanisms of resistance. Ministry of Health of the Slovak Republic pp: 161-165.
- Štefkovicová M, Litvová S (2013) Nosocomial infections in Slovak hospitals: The prevalence of surveillance of nosocomial infections and antibiotic use. Žilina, Slovakia, Zdravéstránky, joint stock company
- Caini S, Hajdu A, Kurcz A, Böröcz K (2013) Hospital-acquired infection due to multidrug-resistant organisms in Hungary, 2005 - 2010. Eurosurveillance 18: 13-21.
- ECDC (2013) Point prevalence survey of health-care associated infection and antimicrobial use in European acute care hospitals 2011-2012.
- (2009) CDC’s National Healthcare Safety Network (NHSN). First state-specific healthcare-associated infections summary data report.
- (2009) United States Department of Health and Human Services. Action Plan to prevent healthcare-associated infections.
- Sydnor ERM, Perl TM (2011) Hospital epidemiology and infection control in acute-care settings. Clinical microbiology reviews 24: 141-173.
- Siebert T, Jurkovic R, Statelová D, Strecha J (2015) Immediate implant placement in and a patient with osteoporosis undergoing patient using bisphosphonate therapy: 1-year preliminary prospective study. J Oral Implantol 44: 360-365.
Citation: Katarína N, Viera R, Martin N, Vladimíra S, Tatiana C, et al. (2016) Benefit of Active Approach to Surveillance of Hospital-acquired Infections. Epidemiology (Sunnyvale) 6:239. Doi: 10.4172/2161-1165.1000239
Copyright: © 2016 Katarína N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 12589
- [From(publication date): 4-2016 - Apr 23, 2024]
- Breakdown by view type
- HTML page views: 11871
- PDF downloads: 718