Documenting the Hypopharyngeal Environment of Patients Undergoing General Endotracheal Tube Anesthesia: A First Look at Intraoperative pH Characteristics
Received: 04-Jul-2015 / Accepted Date: 25-Jul-2015 / Published Date: 31-Jul-2015 DOI: 10.4172/2161-119X.1000202
Abstract
Objectives: While laryngeal injuries are important and not infrequent following both short and extended endotracheal tube exposure, little detailed information is available regarding the hypopharyngeal environment during intubation. The objective of this pilot study was to explore a simple method of accurately documenting hypopharyngeal pH values in surgical patients undergoing endotracheal tube anesthesia and to report the findings.
Methods: Twenty volunteers were continuously monitored intra-operatively using a commercially available hypopharyngeal pH monitoring system. Demographics, pre- and postoperative voice and reflux self reported survey data were also collected.
Results: No complications associated with the pH monitoring system occurred. Median pH was 6.5 (range 6.0-7.0); median recorded time in minutes was 183.9 (range 130.7 – 323.5). 13/20 patients had pH>5.0 ≤ 5.5 events, for up to 113 minutes of monitored time; 2/20 patients had pH>4.0 ≤ 5.0 events, for up to 8 minutes of monitored time; 2/20 patients had pH ≤ 4.0 events, for up to 61 minutes of monitored time.
Conclusions: The hypopharyngeal pH test was used successfully to intra-operatively record hypopharyngeal pH variations. Extended pharyngeal exposures to low pH environments were commonly documented. No associations were found with patient survey scores. Future research appears warranted to expand this study, identify “at-risk” populations and to rigorously evaluate an expanded set of voice-related and lower airway clinical outcomes measures.
Keywords: Anesthesia; Laryngopharyngeal reflux; Laryngeal diseases; Hoarseness; Voice disorders; Esophageal pH monitoring
Introduction
Common laryngopharyngeal complaints following general endotracheal tube anesthesia include hoarseness and sore throat. Postextubation hoarseness has been reported in 12–25 % of patients, while post-extubation sore throat has been described in 6–90% [1]. A recent systematic review of the literature which looked at the occurrence and type of vocal cord injuries after short-term general anesthesia using an endotracheal tube (ET) or laryngeal mask in adults found hoarseness and vocal cord injuries to be common in most studies with several investigations reporting persistent hoarseness and injury for up to 6 months [2].
Several risk factors leading to ET-related laryngeal injury have been described. These include ET size, cuff design, cuff pressure, type of ET, use of an introducer, use of a gastric tube, use of a paralytic agent, use of Propofol, duration of the operation, intubation conditions, and movement of the ET. The pressure exerted on the adjacent laryngeal tissue can reach more than 200 mmHg and lead to ischemic necrosis of the posterolateral laryngeal mucosa since its capillary perfusion pressure is far below that [1]. Additional factors such as sex, weight, history of smoking, the type of operation and gastroesophageal reflux have also been cited [3].
Most studies that have focused on pH monitoring during surgical procedures have done so to answer questions related to aspiration risk. While the majority of such studies report the average pH as well as reflux episodes during surgery none have provided a more detailed evaluation of the exposure time at varied hypopharyngeal pH that might occur during the procedures and how this might relate to laryngeal morbidity.
Given the “gap” in knowledge as to the ET-related procedurespecific factors and patient-specific risk characteristics that may predispose to enhanced risk for laryngeal injury, our pilot study sought to describe the variations in hypopharyngeal pH observed intra-operatively during an ET surgical procedure. The possibility of a relationship between intraoperative prolonged pH environmental exposure with changes (from baseline to post-hospital discharge) of patient voice and reflux self-reported survey outcomes will also be reported. As a descriptive, exploratory pilot study, we sought to gather preliminary data regarding intraoperative pH measures that may be useful to guide future research to advance this important field forward.
Methods
Design, participants, and setting
As an observational cross-sectional study, twenty volunteers were recruited as a convenience sample between June and September 2013 from two surgical services, the Division of Otolaryngology Head and Neck Surgery and the Division of Gynecologic Surgery. Following study start-up, patients were recruited for the study based on the operating room schedule prepared by each service. All patients underwent surgery with general endotracheal (ET) anesthesia, at Stony Brook University Hospital, a tertiary care academic medical center located on Long Island, New York. Patients were excluded from study consideration if they were: < 18 years of age; considered unsafe to maintain the device trans-nasally (e.g. facial surgery); had a history of a deviated septum, frequent epistaxis, nasal polyps, fractured nose, or frequent hoarseness; received anesthesia for a head or neck procedure that might complicate the surgical process (bleeding into the pharynx); were pregnant; or were unwilling to provide informed consent.
Intervention
To obtain our intraoperative pH measures, the Restech® Dx-pH test (Respiratory Technology Corp., San Diego, CA, USA) was selected for this purpose as it was developed to measure reflux in patients suspected of having extraesophageal symptoms presumably related to GERD [4,5]. While traditional hypopharyngeal pH catheters are prone to drying-out effects, which may cause misleading results due to pseudoreflux, the Restech probe reportedly resists drying, and does not require contact with fluid or tissue for electrical continuity. This sensor detects aerosolized or liquid acid, records pH values twice every second (2 Hz) while other pH devices may detect pH values once every 4–6 seconds. The device utilizes a 1.5 mm diameter catheter that incorporates a flashing LED light at its tip to facilitate placement [6,7]. Data is sent from the probe to a wireless recording device and saved to an SD card for latter download and analysis.
Prior to the patient entering the operating room the pH probe was calibrated with the test kit’s pH 7.0 and pH 4.0 calibration solutions. Just after intubation, an attending Otolaryngologist or Anesthesiologist performed trans-nasal placement of the calibrated pH probe. Probe placement was limited to two attempts to reduce potential trauma or irritation to the nose and/or throat. None of the patients were dropped from the study due to this. An intubating laryngoscope was used for direct visualization to confirm the position of the blinking LED probe tip at the level of the epiglottis. The probe was removed and recording terminated after extubation and prior to the patient leaving the operating room. The raw data was converted to pH values and analyzed as described below using Microsoft Excel.
Main outcomes and measures
The baseline pH for each patient was the initial value measured. The measured pH values at or below a defined threshold were recorded as a pH hypopharyngeal event; for example, pH ≤ 6.0 events are measured pH values that were recorded as initiating at a pH of ≤ 6.0 as a threshold value. To explore a wide diversity of pH environments (i.e., pH ≤ 5.5, pH ≤ 5.0, pH ≤ 4.5, and pH ≤ 4.0) we counted the number of events occurring as well as the duration of each event for this set of threshold values. We also attempted to divide the group at a 50th percentile, the pH value at which half the group had exposure and half did not.
All study participants were requested to complete two validated questionnaires, the Reflux Symptom Index (RSI) and a Voice Handicap Index-10 (VHI-10) questionnaires, preoperatively and two to four weeks postoperatively [8-10]. Additional data collected on other covariates included age, height, weight, sex, tobacco use, alcohol use, proton pump inhibitor (PPI) use, a patient given history of gastroesophageal reflux disease (GERD), type of surgical procedure, duration of surgery and any complications that may have been related to the pH monitoring device during surgery and in the immediate postoperative period.
An official GERD diagnosis based on the “gold standard” assessment using esophageal pH monitoring was not required for purposes of this pilot study. Each patient’s past medical history of gastroesophageal reflux disease (GERD) was gathered as part of the pre-surgery assessment, as self-reported by study patients. With symptom relief described, moreover, the patient’s use of refluxrelated medications (PPI or H2 blockers) within the past month prior to their date of surgery was deemed to be an adequate verification of the presence of GERD. The use of antacids (or other over the counter medications) with symptom relief was not deemed sufficient, in and of itself, to document GERD history.
Statistical analysis
Due to our small, pilot studies sample size (n = 20), all comparisons for non-normally distributed variables were performed using nonparametric statistical tests. Comparisons of categorical data elements were made using a Fisher’s exact test; comparisons of continuous variables were made using either a t-test or a Wilcoxon-Mann-Whitney test. Data analysis was done with Microsoft Excel 2010 (Redmond, WA, USA) and STATA 11.0 (College Station, Texas, USA). A p-value ≤ 0.05 was considered statistically significant. Due to the large number of statistical tests performed, some or all of the significant correlations may be false positives (type I errors). No multivariable adjustments were made due to small sample size. Moreover, no Bonferroni corrections were made due the exploratory nature of this pilot study.
Institutional review board approval
This pilot research project was approved by our Institutional Review Board (Committee on Research in Human Subjects [CORIHS]) at Stony Brook University (CORIHS # 2012-1914-R1).
Results
Twenty patients were voluntarily enrolled in this pilot study, as a convenience sample. Operative procedures performed included: microsuspension direct laryngoscopy (n = 1); thyroidectomies (n = 3); gynecologic oncology procedures (n = 16). The pH probe was successfully placed and tolerated throughout surgery without reported complication, including the immediate postoperative period. Six of the 20 study patients enrolled were lost to follow-up, and therefore did not complete the postoperative surveys.
Our enrolled patient characteristics are described in Table 1. In general, our study volunteers were 54.3 (mean age) years old, with only one male patient enrolled. Body mass index (BMI) classification was based upon WHO and NIH guidelines [11, 12]. The majority of patients (80%) were either overweight or obese. Of the study patients, 45% had a history of GERD, 25% had PPI use, and 30% were prior or current smokers. Median values for monitored time and baseline pH are also given.
| All Patients | |
|---|---|
| Variable | (n=20) |
| Age, mean (SD) | 54.3 (14.1) |
| Height, mean (SD), cm | 162.8 (8.9) |
| Weight, mean (SD), kg | 85.2 (23.5) |
| BMI, mean (SD) | 32.3 (9.5) |
| Monitored time, median (IQR), minutes | 183.9 (126.7 - 324.5) |
| Median pH (IQR) | 6.5 (6.0 - 7.0) |
| Baseline pH, median (IQR) | 6.7 (6.2 - 7.2) |
| Female (yes) | 19 |
| Preop RSI > 10 | 8 |
| Tobacco Use (n) | 6 |
| Alcohol Use (n) | 5 |
| PPI Use (n) | 5 |
| History of GERD (n) | 9 |
| BMI: Underweight (n) | 2 |
| BMI: Normal (n) | 2 |
| BMI: Overweight (n) | 4 |
| BMI: Class I obesity (n) | 5 |
| BMI: Class II obesity (n) | 2 |
| BMI: Class III obesity (n) | 5 |
Table 1: Patient demographics.
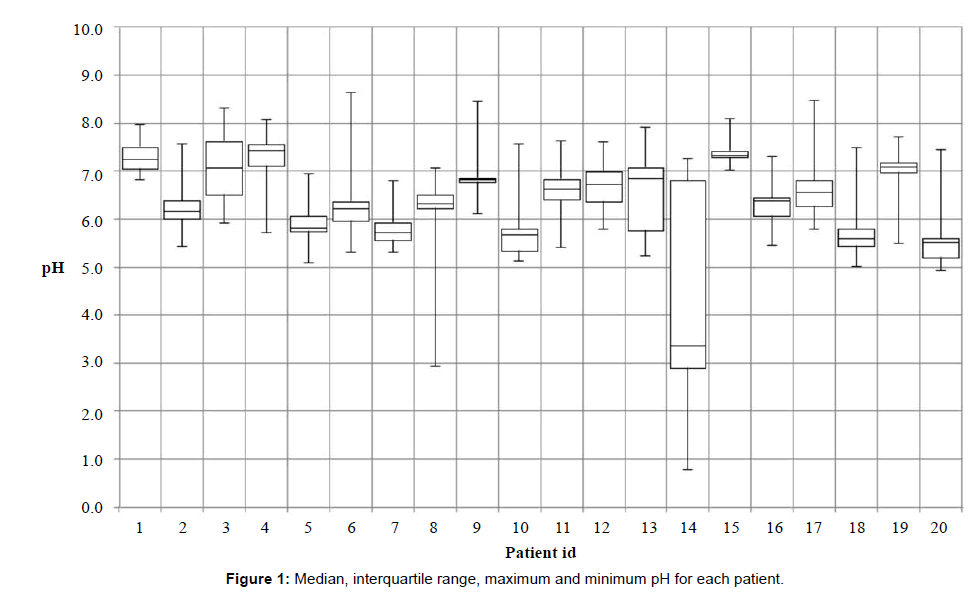
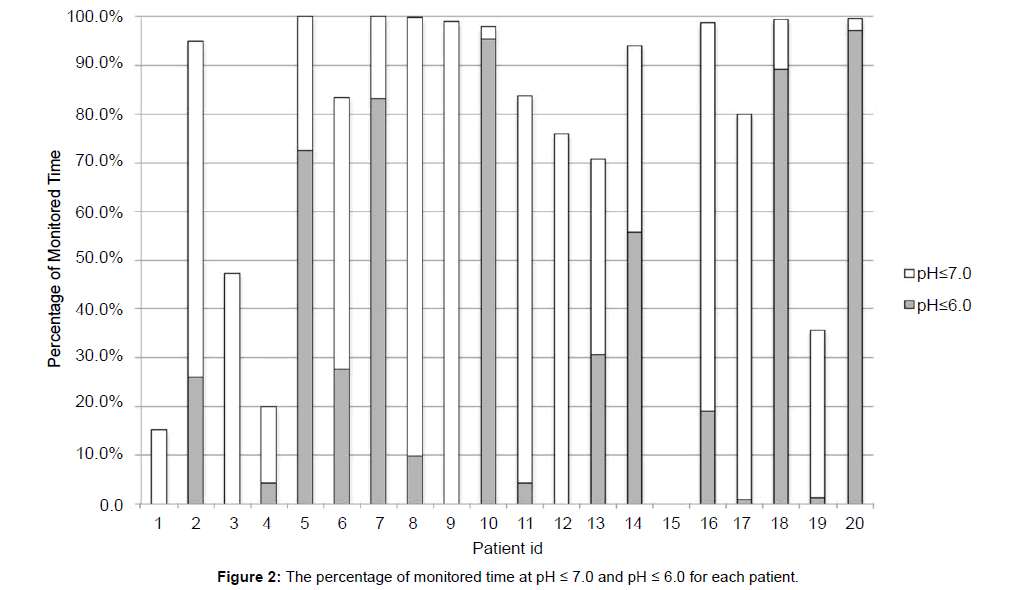
Individual patient pH median values are shown in Figure 1. The median pH for five patients was > 7.0; nine patients were pH ≤ 7.0 > 6.0; six patients were pH ≤ 6.0. The percentage of recorded time at pH ≤ 7.0 and pH ≤ 6.0 is shown if Figure 2. The median percentage time at pH ≤ 6.0 was 14.4% (0.6 – 60.0).
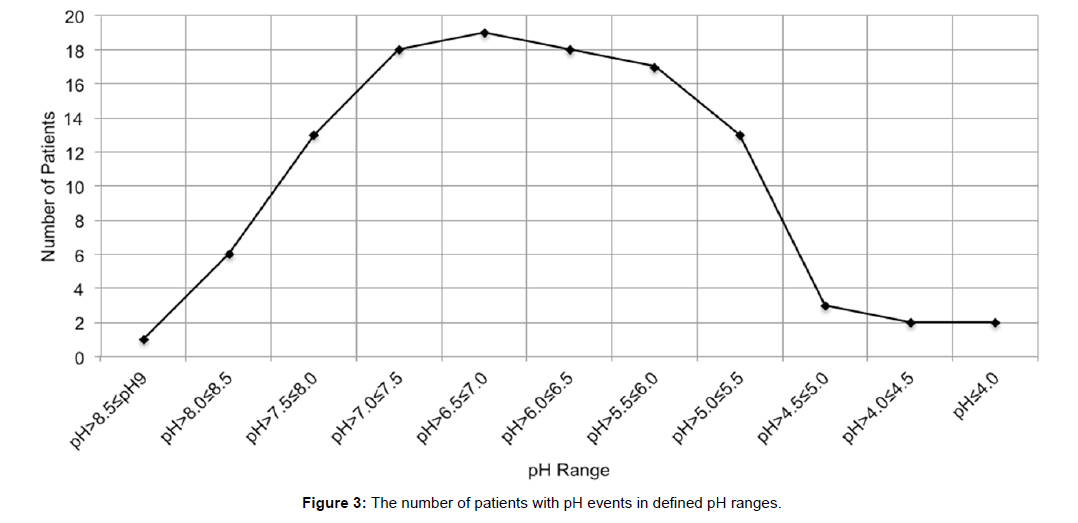
The number of patients with recorded pH values within various pH ranges is shown in Figure 3. Looking at the range of pH < 7.0, 13/20 patients had pH>5.0 ≤ 5.5 events, for up to 113 minutes of monitored time; 2/20 patients had pH>4.0 ≤ 5.0 events, for up to 8 minutes of monitored time; 2/20 patients had pH ≤ 4.0 events, for up to 61 minutes of monitored time. Of the thirteen with pH ≤ 5.5 events, three patients events were of only 0.5 seconds each. It was therefore felt to be reasonable to place these three in the “without pH ≤ 5.5 events” group in order to create a better approximation of a 50th percentile of pH events for group analysis.
There was no difference in the incidence of pH ≤ 5.5 hypopharyngeal events and baseline patient characteristics, Table 2, with the exception that patients with pH ≤ 5.5 events had significantly lower mean weight and BMI. Comparisons of subgroups of patients with and without pH ≤ 5.5 events are summarized in Table 3. There were no significant differences between these sub-groups with regard to the incidence of pH ≤ 5.5 hypopharyngeal events with the exception of baseline pH that was significantly lower in those with pH ≤ 5.5 events.
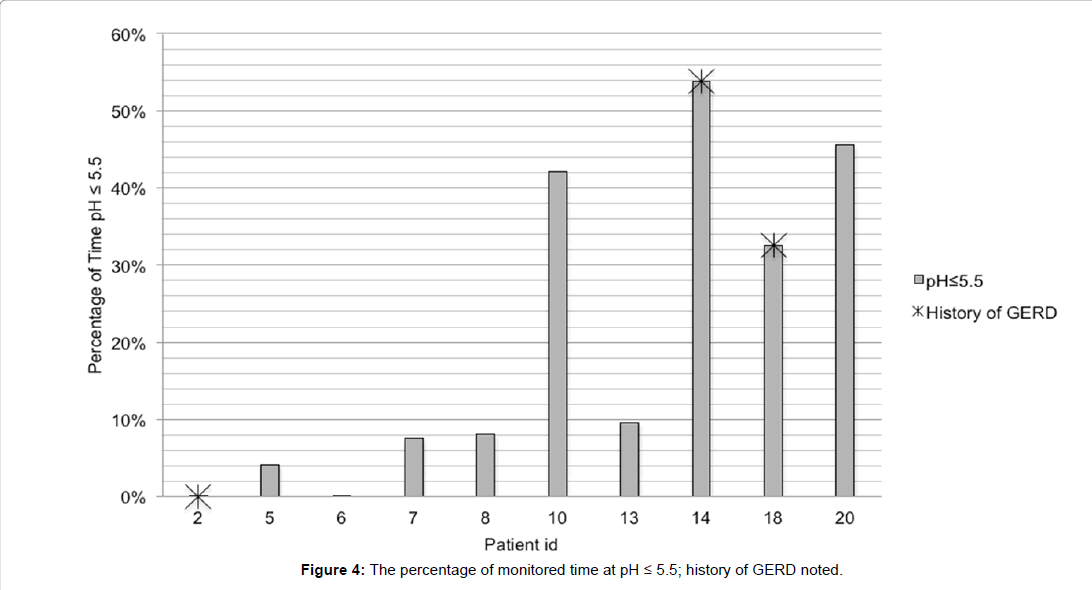
The percentage of total monitored time at measured pH ≤ 5.5 for each of the ten patients is documented in Figure 4. Only two of the nine patients with a history of GERD had pH ≤ 5.5 events was higher in the sub-group without a history of gastroesophageal reflux disease. Two (2,18) of the five patients reporting PPI use had pH ≤ 5.5 events, one of which represented a third of the monitored time.
Patient self-reported survey findings are shown in Table 3. The average pre- and post-operative RSI values were 7.8 (6.6) and 4 (5.3) respectively; pre- and post-operative VHI-10 values were 1.5 (4.0) and 1.6 (3.6) respectively. Baseline and follow-up RSI and VHI-10 scores were not significantly different between patient sub-groups. The analysis of VHI-10 scores may have been affected by the consistently low scores reported pre- and postoperatively for both groups.
The number of pH ≤ 5.5 events categorized by duration of events is summarized in Table 4. The percentage of monitored time for the total number of events for each duration per patient is also shown. 81% of pH ≤ 5.5 events were less than one minute; 13% were 1-10 minute duration; 4% were 10 – 60 minute duration; 3% were over one hour duration.
Discussion
The risk of injury to the larynx and trachea from endotracheal tube anesthesia has been well known for many years. According to anesthesia-related claims in a closed claims database, 7% of all claims are related to airway injury [13]. The most frequent site of injury is the larynx. In addition to arytenoid subluxation and vocal fold paralysis, associated lesions have included inflammation, edema, hematoma, scarring and granuloma formation [14]. Regarding prolonged intubation, numerous studies have found various degrees of similar laryngeal injuries in nearly all patients intubated for more than 48 hours [15]. These injuries may result in severe, prolonged laryngeal dysfunction and the majority has been associated with extraesophageal reflux [8]. Damage may occur due to a drop in pH and also due to exposure to noxious elements in the refluxate, including pepsin, bile salts and pancreatic enzymes [16].
| without pH≤5.5 events | with pH≤5.5 events | P Value | |
|---|---|---|---|
| n | 10 | 10 | |
| Age, mean (SD) | 56 (14.5) | 53.6 (14.1) | 0.7a |
| Height, mean (SD), cm | 163.4 (11.5) | 162.3 (5.9) | 0.8a |
| Weight, mean (SD), kg | 96.8 (19.0) | 73.7 (22.6) | 0.02a |
| BMI, mean (SD) | 36.6 (8.4) | 28.2 (9.1) | 0.04a |
| Preop RSI > 10 (n) | 4 | 4 | 1b |
| Tobacco Use (n) | 2 | 4 | 0.6b |
| Alcohol Use (n) | 1 | 4 | 0.3b |
| PPI Use (n) | 3 | 2 | 1b |
| History of GERD (n) | 6 | 3 | 0.4b |
| aindependent samples t-test assuming equal variance; bFisher’s exact test | |||
Table 2: pH events.
| without pH≤5.5 events | with pH≤5.5 events | PValuea | |
|---|---|---|---|
| n | 10 | 10 | |
| Monitored time, median (IQR), min | 316.2 (136.5 - 365.5) | 168.2 (122.8 - 205.2) | 0.3 |
| Baseline pH, median (IQR) | 7.2 (6.8 - 7.2) | 6.3 (5.9 - 6.5) | 0.001 |
| Baseline RSI, median (IQR) | 6.5 (4.3 - 15.3) | 3 (0.5 - 11.5) | 0.2 |
| Baseline VHI-10, median (IQR) | 1.5 (0 - 2) | 0 (0 - 0) | 0.06 |
| Follow-up RSI, median (IQR) | 3 (1 - 9) | 0 (0 - 3) | 0.3 |
| Follow-up VHI-10, median (IQR) | 0 (0 - 3) | 0 (0 - 0) | 0.4 |
| a Wilcoxon (Mann-Whitney) | |||
Table 3: pH events.
Most studies that have included hypopharyngeal pH measures have done so in terms of understanding aspiration risk with various anesthesia devices. Turndorf et al and Blitt et al utilized dye instillation into the stomach to look for extraesophageal regurgitation in patients undergoing general anesthesia [17,18]. They found a regurgitation rate of 14.5% and 7.8% respectively. Carlsson and Islander used pH test paper at the end of surgery to assess hypopharyngeal pH, which was found to average pH 5.6 (1.0) [19]. Kofke et al. reported on hypopharyngeal pH during mask anesthesia. Patients were grouped by inhalation anesthetic [20]. They used a monocrystalline antimony electrode connected to a pH meter (Biosearch Medical Products, Somerville, NJ), recording readings at approximately five-minute intervals over one hour. The range of hypopharyngeal pH was between 5.0 and 7.7. Joshi et al reported continuous hypopharyngeal monitoring comparing laryngeal mask to tracheal intubation [21]. A monocrystalline antimony electrode was used and measures stored in a portable pH data logger system (Reflux Monitoring System I; Sandhill, Littleton, CO). Four patients were eliminated from the study due to difficulty in retrieving pH data from the data logger. There were no episodes of hypopharyngeal regurgitation (pH < 4) detected during the course of measurement. At no time did the hypopharyngeal pH value decrease below 5.5.The hypopharyngeal pH values in both groups were similar, ranging between 5.5 and 7.5, with median values of 5.7 and 6.2. The pH in any given patient did not vary more than 1.0 unit from the initial value after placement of the airway device throughout the study period. Comparing six airway devices Khazin, et al focused on “regurgitation” episodes (pH<4), but reported minimal pH values ranging from approximately pH 1 – pH 8; twenty of 180 patients had episodes pH<4.0 [22]. They used nondisposable antimony catheters with an external reference electrode (Medtronic Functional Diagnostics,Inc, c/o Medtronic, Inc, Minneapolis, MN), measuring pH eight times per minute.
| number of events (% monitored time) | ||||
|---|---|---|---|---|
| patient id | <1minute | 1-10minute | 10-60minute | >1hour |
| 2 | 2 (<1%) | 0 | 0 | 0 |
| 5 | 7 (<1%) | 2 (3.3%) | 0 | 0 |
| 6 | 3 (<1%) | 0 | 0 | 0 |
| 7 | 13 (3.8%) | 1 (3.7%) | 0 | 0 |
| 8 | 4 (<1%) | 0 | 1 (8%) | 0 |
| 10 | 10 (<1%) | 1 (<1%) | 0 | 1 (40.8%) |
| 13 | 5 (<1%) | 1 (<1%) | 1 (8.6%) | 0 |
| 14 | 3 (1.2%) | 1 (1.1%) | 0 | 1 (51.6%) |
| 18 | 23 (5.8%) | 5 (4.9%) | 0 | 1 (21.8%) |
| 20 | 20 (4.5%) | 3 (6.7%) | 2 (34.5%) | 0 |
Table 4: Duration of pH ≤ 5.5 events.
To our knowledge, this study is the first to report a more detailed analysis of intraoperative hypopharyngeal pH values from monitoring during surgery performed under general endotracheal tube anesthesia. The Restech® Dx-pH wireless system proved to be easy to setup, position and reliable in terms of data capture. No device-related complications were encountered.
While the results of our pilot study should not be generalized broadly, they are intriguing. Over 50% of monitored time for six patients studied had events of pH ≤ 6.0 and four of these were over 80% of monitored time. Looking in detail at pH ≤5.5 events, the majority of these events were of trivial duration of less than one minute; seven patients recorded short duration events of one to ten minutes; three patients experienced moderately long events of ten to sixty minutes and three experienced long events of over one hour. The long duration pH ≤ 5.5 events represented approximately 22% - 52% of the monitored time.
As a limitation of our current pilot study, we used a convenience sample of study volunteers, resulting in almost all female patients being recruited. Future studies should be designed to recruit both a larger and more diverse population, as well as to identify patient subpopulations (e.g., patients with a GERD history) that may be “at risk” for extended exposure to various pH hypopharyngeal environments. Our study was underpowered to detect a statistical difference across patient sub-groups.
The range of pH values recorded throughout the study was surprisingly broad. The stomach secretes acid at a pH of 1.5 to 2.0 and exhaled breath condensate has been found to have a pH range of 4-6 depending on disease state [23,24]. Correlative data utilizing multichannel intraluminal pH monitoring, impedance and other technologies will need to be performed to better understand the etiology of the pH fluctuations. Future studies will also need to include preand post-procedural laryngeal evaluations such as laryngoscopy, more extensive patient-reported outcome measures and objective measure of voice such acoustic analysis. Extending observations to intensive care settings, the role that various hypo pharyngeal pH environments may play in prolonged intubation (and re-intubation) clinical outcomes and resource utilization should also be explored.
Conclusion
Our pilot study documented a surprisingly wide range and dynamic pH environment during general endotracheal tube anesthesia. The Restech pH-Dx test appears to be a safe, simple to use tool that can be considered to support future investigations. The reasons for the unanticipated variability in the frequency and duration of low pH exposure during ET-related surgical procedures need to be elucidated. It is unclear what role various pH environments may play in the pathogenesis of laryngotracheal morbidity or voice-related performance challenges arising post-ET surgery. As this study has raised important questions regarding potential for laryngeal damage during routine surgical procedures, further research appears warranted to better understand the clinical significance of these preliminary findings.
References
- Bottcher A, Mencke T, Zitzmann A, Knecht R, Jowett N, et al. (2014) Laryngeal injuries following endotracheal intubation in ENT surgery: predictive value of anatomical scores. Eur Arch Otorhinolaryngol 271: 345-352.
- Mendels EJ, Brunings JW, Hamaekers AE, Stokroos RJ, Kremer B, et al. (2012) Adverse laryngeal effects following short-term general anesthesia: a systematic review. Arch Otolaryngol Head Neck Surg 138: 257-264.
- Mencke T, Echternach M, Plinkert PK, Johann U, Afan N, et al. (2006) Does the timing of tracheal intubation based on neuromuscular monitoring decrease laryngeal injury? A randomized, prospective, controlled trial. AnesthAnalg 102: 306-312.
- Wiener GJ, Tsukashima R, Kelly C, Wolf E, Schmeltzer M, et al. (2009) Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice 23: 498-504.
- Sun G, Muddana S, Slaughter JC, Casey S, Hill E, et al. (2009) A new pH catheter for laryngopharyngeal reflux: Normal values. Laryngoscope 119: 1639-1643.
- Savarino E, Zentilin P, Savarino V, Tenca A, Penagini R, et al. (2013) Functional testing: pharyngeal pH monitoring and high-resolution manometry. Ann N Y AcadSci 1300: 226-235.
- Ayazi S, Lipham JC, Hagen JA, Tang AL, Zehetner J, et al. (2009) A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J GastrointestSurg 13: 1422-1429.
- Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16: 274-277.
- Arffa RE, Krishna P, Gartner-Schmidt J, Rosen CA (2012) Normative values for the Voice Handicap Index-10. J Voice 26: 462-465.
- Rosen CA, Lee AS, Osborne J, Zullo T, Murry T (2004) Development and validation of the voice handicap index-10. Laryngoscope 114: 1549-1556.
- http://www.nhlbi.nih.gov/health/ public/heart/obesity/lose_wt/bmi_dis.htm
- Metzner J, Posner KL, Lam MS, Domino KB (2011) Closed claims' analysis. Best Pract Res ClinAnaesthesiol 25: 263-276.
- Domino KB, Posner KL, Caplan RA, Cheney FW (1999) Airway injury during anesthesia: a closed claims analysis. Anesthesiology 91: 1703-1711.
- Colton House J, Noordzij JP, Murgia B, Langmore S (2011) Laryngeal injury from prolonged intubation: a prospective analysis of contributing factors. Laryngoscope 121: 596-600.
- Ylitalo R, Baugh A, Li W, Thibeault S (2004) Effect of acid and pepsin on gene expression in laryngeal fibroblasts. Ann OtolRhinolLaryngol 113: 866-871.
- Turndorf H, Rodis ID, Clark TS (1974) "Silent" regurgitation during general anesthesia. AnesthAnalg 53: 700-703.
- Blitt CD, Gutman HL, Cohen DD, Weisman H, Dillon JB (1970) "Silent" regurgitation and aspiration during general anesthesia. AnesthAnalg 49: 707-713.
- Carlsson C, Islander G (1981) Silent gastropharyngeal regurgitation during anesthesia. AnesthAnalg 60: 655-657.
- Kofke WA, Fasano M, Keamy MF 3rd, Derr JA (1987) Continuous hypopharyngeal pH during anesthesia via mask. Anesthesiology 67: 434-436.
- Joshi GP, Morrison SG, Okonkwo NA White PF (1996) Continuous hypopharyngeal pH measurements in spontaneously breathing anesthetized outpatients: laryngeal mask airway versus tracheal intubation. AnesthAnalg 82: 254-257.
- Khazin V, Ezri T, Yishai R, Sessler DI, Serour F, et al. (2008) Gastroesophageal regurgitation during anesthesia and controlled ventilation with six airway devices. J ClinAnesth 20: 508-513.
- Wood JM, Hussey DJ, Woods CM, Watson DI, Carney AS (2011) Biomarkers and laryngopharyngeal reflux. J LaryngolOtol 125: 1218-1224.
- Paget-Brown AO, Ngamtrakulpanit L, Smith A, Bunyan D, Hom S, et al. (2006) Normative data for pH of exhaled breath condensate. Chest 129: 426-430.
Citation: Regenbogen E, Oleszak SP, Corrado T, Shroyer ALW, Vanner E, et al. (2015) Documenting the Hypopharyngeal Environment of Patients Undergoing General Endotracheal Tube Anesthesia: A First Look at Intraoperative pH Characteristics. Otolaryngology 5: 202. Doi: 10.4172/2161-119X.1000202
Copyright: © 2015 Regenbogen E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 14377
- [From(publication date): 7-2015 - Apr 26, 2024]
- Breakdown by view type
- HTML page views: 10012
- PDF downloads: 4365