Fatal Massive Pulmonary Hemorrhage in Dengue Infection
Received: 16-May-2016 / Accepted Date: 15-Jun-2016 / Published Date: 22-Jun-2016 DOI: 10.4172/2161-1165.1000251
Abstract
Background
Pulmonary hemorrhage is a very rare complication of dengue infection. This condition presenting with hemoptysis has been reported in 1.4% of dengue infections. However, major hemorrhage is unusual except when associated with profound or prolonged shock. In contrast although this case showed no features of plasma leakage, it resulted in massive pulmonary hemorrhage leading to death.
Case Presentation
A 17 year old previously healthy Sri Lankan, Sinhalese male presented with a 5 day history of fever. On admission he was ill looking and the hematocrit was 44.8%. He was treated in the High Dependency Unit with close monitoring and was started on normal saline 100 ml per hour and showed improved blood pressure and hematocrit value of 41.5% with the initial chest X-ray and ultrasound on abdomen showing no fluid leakage. But within a few hours he developed sudden onset of hemoptysis and respiratory distress, and an urgent chest X-ray taken showed a patchy right sided middle lobe opacity with no pleural effusion. Death occurred following failed resuscitation and the post mortem revealed massive pulmonary hemorrhage.
Conclusion
Pulmonary hemorrhage in dengue infection has rapid progression associated with high mortality. Thus, a high index of suspicion is needed for diagnosis.
Keywords: Dengue virus; Arthropod borne diseases; Dengue fever; Severe dengue infection; Dengue hemorrhagic fever; Pulmonary hemorrhage; Sri Lanka
Abbreviations
DF: Dengue Fever; DHF: Dengue Hemorrhagic Fever; SDI: Severe Dengue Infection; BP: Blood Pressure; Bpm: Beats per minute; WBC: White Blood cell count; HCT: Haematocrit; PLT: Platelet count; Hb: Haemaoglobin concentration; ICU :Intensive care unit; ALT: Alanine transaminase; AST: Aspartate transaminase; DIC: Disseminated Intravascular Coagulation; WHO: World Health Organization
Background
Dengue fever (DF) is a major health hazard in tropical countries including Sri Lanka. This is the commonest arthropod- borne viral infection caused by flavivirus. The dengue virus currently has 4 different antigenic varieties (DEN-1, DEN-2, DEN-3 and DEN-4); which are all transmitted during diurnal biting of Aedes aegypti , and Aedes albopictus mosquitos. This infection is responsible for an estimated 100 million cases of dengue fever, 500,000 cases of dengue hemorrhagic fever (DHF), and 25,000 deaths annually [1]. According to the 2009 World Health Organization (WHO) classification [2], severe dengue infection (SDI) can present with severe plasma leakage, severe bleeding, or severe organ dysfunction. According to the previous WHO classification of Dengue infection [3], DHF was described as the presence of widespread plasma leakage with or without hemorrhagic manifestations such as bleeding from sites of trauma, gastrointestinal bleeding, and hematuria. SDI if left untreated, it is likely to progress to dengue shock syndrome and circulatory failure after which death is inevitable.
Although SDI presents with multisystem hemorrhagic manifestations, dengue infection with pulmonary hemorrhage is rarer or under reported [4,5]. For the best of our knowledge this is the first reported case of SDI with fatal pulmonary hemorrhage in Sri Lanka.
Case Presentation
A 17 year old previously healthy Sri Lankan, Sinhalese male presented to a Base Hospital with a 5 days history of fever with chills, associated with arthralgia, myalgia, sore throat, frontal headache and retro-orbital pain. He has had dry cough 3 days ago. He had no right hypochondrial pain, and no bleeding manifestations like haemoptysis, or malaena. He maintained a normal urine output at that time, and had no postural dizziness. On examination he was febrile, tachypnoeic, had a blood pressure (BP) of 98/60 mmHg with no postural drop, pulse rate of 110 beats per minute (bpm) with normal capillary refilling. His initial blood counts showed low White cell count (WBC) of 3.4 × 103/ μl, haematocrit (HCT) of 44.8%, and platelet count (PLT) of 48 × 103/ μl, with a hemoglobin (Hb) of 14 g/dl. Dengue infection was confirmed by a positive dengue IgM serology result. DHF of the critical phase with impending shock was suspected, and he was immediately transferred to the Intensive Care Unit (ICU) at a tertiary care hospital for further management.
On admission to the ICU, which was 2 hours after the initial presentation, he had a BP of 125/80 mmHg with no postural drop, increased pulse rate of 126 bpm, and respiratory rate of 46 per minute with an oxygen saturation of 92%. He was managed with critical monitoring of fluid balance and maintenance of urine output. Repeat blood investigations showed a reduction of HCT to 41.5%, WBC to 3.1 × 103/μl, and PLT to 39 × 103/μl, with Hb remaining at 15 g/dl. There was mild elevation of liver enzymes and renal function tests, with an alanine aminotransferase (ALT) of 128.6 U/l, aspartate aminotransferase (AST) of 151.6 U/l, and serum creatinine of 83 Umol/l with normal serum electrolytes. The initial chest X-ray and ultrasound scan of the chest and abdomen were normal with no evidence of fluid leakage.
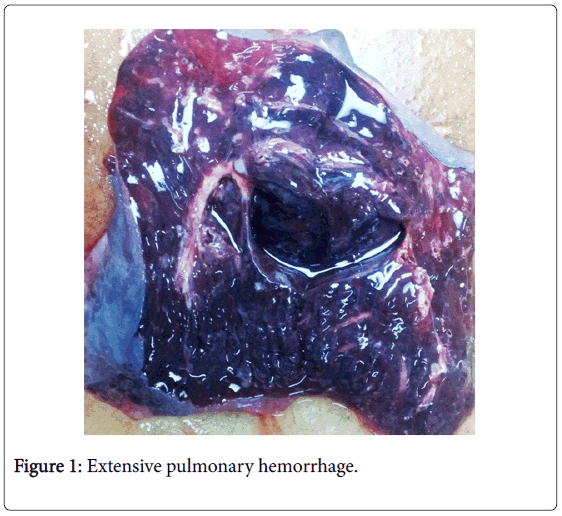
About 5-6 hours later, he developed sudden onset of significant haemoptysis and pinkish froth with dyspnea, and the oxygen saturation dropped to 80% while on oxygen. He was immediately intubated and ventilated, and saturation could be barely maintained with high concentration of oxygen. His BP was un-recordable due to cold clammy peripheries, and urgently taken blood investigations revealed a significant reduction of HCT to 36.3%, and Hb of 10 g/dl indicating significant hemorrhage. An urgent ultrasound scan of the abdomen showed no free fluid, and chest X-ray showed a patchy opacity in the right sided middle lobe with no pleural effusion. He developed sudden cardiac arrest, and death occurred followed with failure in subsequent cardio-pulmonary resuscitation. The post mortem revealed extensive pulmonary hemorrhage, (Figure 1) with no evidence of pleural effusion or ascites.
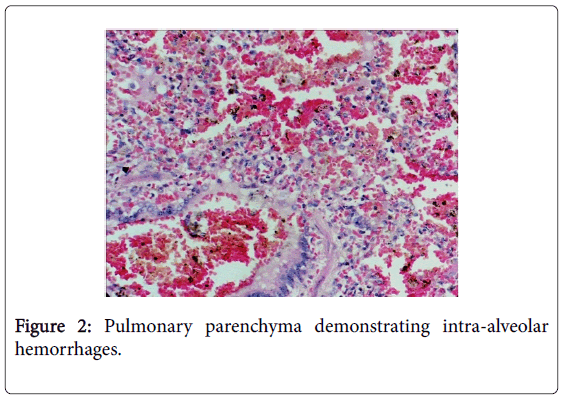
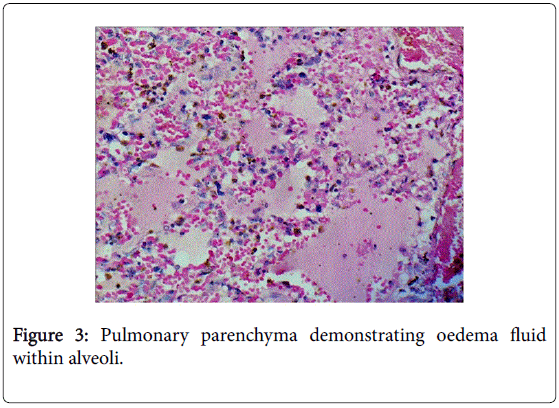
Histopathology revealed pulmonary parenchyma demonstrating intra-alveolar hemorrhages (Figure 2) and oedema fluid within alveoli (Figure 3).
Discussion
Dengue predominantly affects children and young adults. According to the 2009 WHO classification [2], presentation of symptomatic dengue infection can range from undifferentiated fever, dengue fever with or without warning signs, and SDI presenting as severe plasma leakage, severe bleeding, or severe organ dysfunction. DF is characterized by biphasic fever, skin rash, headache, retro-orbital pain, photophobia, cough, vomiting, myalgia, arthralgia, leucopenia and thrombocytopenia; most which were seen in this case as well. DHF is usually associated with secondary dengue infection but can rarely appear during a primary infection [6]. A second attack of DHF is very rare and occurs in about 0.5% of cases according a study [7].
According to the previous WHO criteria, DHF is defined by the presence of fever lasting 2-7 days, hemorrhagic tendencies, thrombocytopenia <100,000 cells/mm3, and evidence of plasma leakage [3]. However, this case showed no evidence of plasma leakage, and is thus classified under SDI with severe bleeding, according to the current 2009 Dengue Guidelines [2], and the diagnosis was confirmed serologically by a positive IgM result.
The pathophysiology of leaking in dengue infection is explained by the enhancement of the immune activation, particularly during a secondary infection, leading to exaggerated cytokine response resulting in increased vascular permeability, which is also helped by viral products such as NS1 antigen which may play a role in compliment activation [8]. TNF-α has been implicated in severe manifestations like hemorrhage in some animal models [9]. Higher levels of viral load and NS1 antigen have been detected in DHF compared to DF, suggesting that the viral burden may be a key determinant of disease severity such as the amount of pleural effusion [10]. The hallmark of DHF; plasma leakage begins around the transition from febrile to afebrile phase and lasts 24-48 hours, and is usually minimal, that it may not be clinically detected, even in cases of shock prior to fluid therapy. A rise in HCT 20% above the baseline level may be the earliest evidence of fluid leakage, which was not detected in this case. If timely and adequate fluid replacement is not done during the critical phase of the leakage, death may follow by shock within 12-24 hours, or may give rise to other complications like metabolic acidosis, electrolyte imbalance, multi organ failure, severe hemorrhage from organs and encephalopathy which have a poor prognosis. However, major hemorrhage is unusual except when associated with profound or prolonged shock [11]. In contrast, this case showed no plasma leakage, but resulted in massive pulmonary hemorrhage leading to death.
Although the pathogenesis of severe bleeding in SDI is not yet well described, it could be similar to bleeding in DHF, which is thought to be a multifactorial process including abnormalities in coagulation cascade, thrombocytopenia, platelet dysfunction, disseminated intravascular coagulation (DIC), and vascular defects. In DHF it is likely that coagulation proteins also leak out of the vascular compartment due to increased vascular permeability, and levels are further reduced due to the dilutional effect following fluid replacement. In severe and prolonged shock, in combination with severe thrombocytopenia, secondary effects of hypoxia and acidosis may result in true DIC and major hemorrhage [12]. Studies have shown abnormal prothrombin time, or a combination of biphasic fever pattern, haemo concerntration, PLT<50,000/mm3, and elevated ALT as predictors of spontaneous bleeding in dengue [13]. Studies have shown gastrointestinal tract hemorrhage to be the commonest site of hemorrhage (46.9%), followed by petichae (31.6%), gum bleeding (19.4%) and epistaxis (10.2%) [14]. Pulmonary hemorrhage is a rare complication of Dengue infection, presenting with hemoptysis that has been reported in 1.4% of dengue infections [4,5].
Other pulmonary manifestations of SDI, though rare, are pleural effusion, and pneumonitis resulting in respiratory distress syndrome. Pulmonary hemorrhage is an even rarer manifestation. Histopathological studies of lung tissue in DHF with lung involvement have revealed interstitial pneumonia associated with focal or diffused zones of alveolar congestion and hemorrhage, increased number of alveolar macrophages, recruiting of platelets, mononuclear and polymorphonuclear cells [15].
There is no specific treatment for dengue infection apart from the critical monitoring of fluid balance and fluid therapy as supportive treatment. Studies have shown that prophylactic transfusion of platelets or fresh frozen plasma did not reduce bleeding or expedite platelet recovery and instead caused fluid overload. The improvement of platelet count by transfusion was transient, lasting <5 hours [16]. Mortality may be reduced to <1% with appropriate supportive therapy [17].
Conclusion
Severe dengue infection with bleeding, though rarely, can present with massive fatal pulmonary hemorrhage, even in the absence of any features of plasma leakage. Pulmonary hemorrhage in dengue infection has rapid progression with high mortality, and thus needs a high index of suspicion for diagnosis.
Consent
Written informed consent was obtained from the patient’s mother for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
Authors’ Contributions
Analysis and interpretation of patient data and literature review were done by DMPUKR, KPJ EMME and TJ. DMPUKR and TJ guided the other authors in reporting this case and corrected the final manuscript. DH helped in collecting patient information. All authors were involved in the management of the patient and read and approved the final manuscript.
Acknowledgement
We all express our gratitude to the patient’s mother who kindly gave consent for this case to be presented in this paper. The authors thank Mahes Salgado, the Head, English Language Teaching Unit of the University of Peradeniya for editorial help.
References
- Gubler DJ (1998) Dengue and dengue hemorrhagic fever.ClinMicrobiol Rev 11: 480-496.
- World Health Organization (2009) Dengue Guidelines for diagnosis, treatment, prevention and control, Geneva.
- World Health Organization (1997) Dengue haemorrhagic fever: diagnosis, treatment, prevention control, Geneva.
- Setlik RF, Ouellette D, Morgan J, McAllister CK, Dorsey D, et al. (2004) Pulmonary hemorrhage syndrome associated with an autochthonous case of dengue hemorrhagic fever.South Med J 97: 688-691.
- Liam CK, Yap BH, Lam SK (1993) Dengue fever complicated by pulmonary haemorrhage manifesting as haemoptysis.J Trop Med Hyg 96: 197-200.
- Chye JK, Lim CT, Ng KB, Lim JM, George R, et al. (1997) Vertical transmission of dengue.Clin Infect Dis 25: 1374-1377.
- Nimmannitya S, Kalaayanarooj S, Nisalak A(1990) Second attack of Dengue Hemorrhagic fever. Proceedings of the International Symposium on Dengue and Dengue Hemorrhagic Fever, Bangkok.
- Avirutnan P, Punyadee N, Noisakran S, Komoltri C, Thiemmeca S, et al. (2006) Vascular leakage in severe dengue virus infections: a potential role for the nonstructural viral protein NS1 and complement.J Infect Dis 193: 1078-1088.
- Yen YT, Chen HC, Lin YD, Shieh CC, Wu-Hsieh BA (2008) Enhancement by tumor necrosis factor alpha of dengue virus-induced endothelial cell production of reactive nitrogen and oxygen species is key to hemorrhage development.J Virol 82: 12312-12324.
- Vaughn DW, Green S, Kalayanarooj S, Innis BL, Nimmannitya S, et al. (2000) Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity.J Infect Dis 181: 2-9.
- Tagore S, Yim CF, Kwek K (2007) Dengue haemorrhagic fever complicated by eclampsia in pregnancy.Singapore Med J 48: e281-e283.
- Wills BA, Oragui EE, Stephens AC, Daramola OA, Dung NM, et al. (2002) Coagulation abnormalities in dengue hemorrhagic Fever: serial investigations in 167 Vietnamese children with Dengue shock syndrome.Clin Infect Dis 35: 277-285.
- Shivbalan S, Anandnathan K, Balasubramanian S, Datta M, Amalraj E (2004) Predictors of spontaneous bleeding in Dengue.Indian J Pediatr 71: 33-36.
- Chhina DK, Goyal O, Goyal P, Kumar R, Puri S, et al. (2009) Haemorrhagic manifestations of dengue fever and their management in a tertiary care hospital in north India.Indian J Med Res 129: 718-720.
- Basílio-de-Oliveira CA, Aguiar GR, Baldanza MS, Barth OM, Eyer-Silva WA, et al. (2005) Pathologic study of a fatal case of dengue-3 virus infection in Rio de Janeiro, Brazil.Braz J Infect Dis 9: 341-347.
- Lum LC, Abdel-Latif Mel-A, Goh AY, Chan PW, Lam SK (2003) Preventive transfusion in Dengue shock syndrome-is it necessary?J Pediatr 143: 682-684.
- Chaturvedi UC (2006) The curse of dengue.Indian J Med Res 124: 467-470.
Citation: Ralapanawa DMPUK, Jayawickreme KP, Ekanayake EMM, Jayalath T, Herath D (2016) Fatal Massive Pulmonary Hemorrhage in Dengue Infection. Epidemiology (Sunnyvale) 6:251. Doi: 10.4172/2161-1165.1000251
Copyright: © 2016 Ralapanawa DMPUK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 15199
- [From(publication date): 6-2016 - Apr 25, 2024]
- Breakdown by view type
- HTML page views: 14380
- PDF downloads: 819