PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
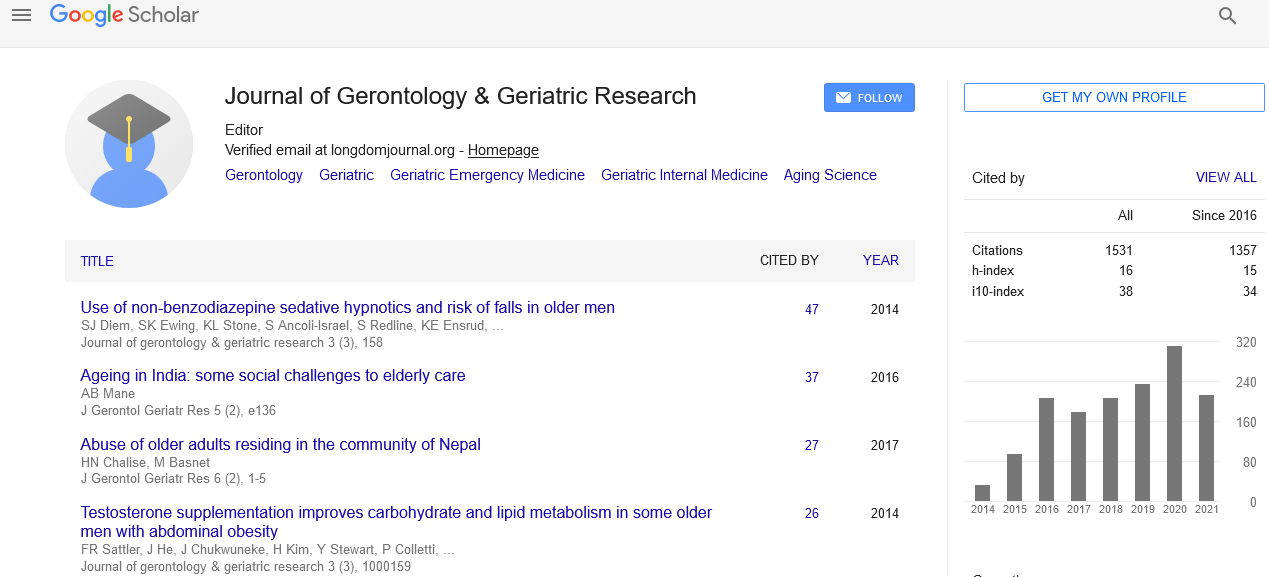
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Depression and dementia in the context of chronic pain
International Conference on Geriatrics & Gerontology
July 08-10, 2014 DoubleTree by Hilton Hotel Chicago-North Shore Conference Center, USA
Adina Carmen Rusu Klappheck
Scientific Tracks Abstracts: J Gerontol Geriat Res
Abstract:
Typically, pain hurts. It feels bad. And in a certain sense, it is bad, sometimes producing profound suffering. But pain is also critically useful, motivating us to avoid and limit bodily damage. So, while pain sometimes ruins lives, it also frequently saves them. In short, pain is important. During recent decades, the empirical sciences have made remarkable progress in getting to grips with pain, for example by detailing the peripheral neural mechanisms and the brain activation patterns (the socalled pain matrix) associated with it and nociception. Yet these advances have cast little light on a key question: How do people in pain understand and communicate their pain and suffering, and how do they relate pain to their bodies and to themselves? The question of how we understand and communicate pain is crucially important. Introspective reports remain the principal basis on which physicians?aiming to relieve pain and suffering?attempt to determine how subjects feel. Yet progress in explaining how subjects articulate, communicate, and understand their pain has been limited. What is responsible for the limited progress, we suggest, are three false assumptions of the traditional view of pain: (i) that pain is independent of the subject?s linguistic capacities and pain concepts; (ii) conversely, that subjects? understanding and processing of pain language is independent of pain processing in their brains; and (iii) that, being subjective and ?private? states, we cannot improve on our understanding of one another?s expressions of pain and suffering. Thanks to recent advances in the philosophy, psychology and neuroscience of pain, we think that the time is ripe to tackle these problems in order to develop a new theoretical framework that will allow us to better understand how subjects articulate, communicate, and understand their pain, and also to generate significant hypotheses to be empirically tested during the course of this project.
Biography :
Adina Rusu-Klappheck is assistant professor at the Department of Medical Psychology University of Bochum, Germany and associate fellow at the Department of Psychology, Royal Holloway, and University of London, U.K. She is a clinical psychologist, trained in cognitive-behavioural psychotherapy. In 2009 she obtained her PhD degree in Psychology at the University of London (Thesis: ?Cognitive biases and future thinking in chronic pain?). She is a Psychology graduate of the University of Bochum, Germany. Afterwards she earned a postgraduate degree in Cognitive-Behavioural Psychotherapy and gained experience as a clinical psychologist in a pain management unit and psychiatric hospitals. She has worked as a psychotherapist with elderly people, children and adolescents in different settings. As an assistant professor, she has been involved in teaching health psychology, clinical psychology and stress management.