Indexed In
- Open J Gate
- JournalTOCs
- The Global Impact Factor (GIF)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
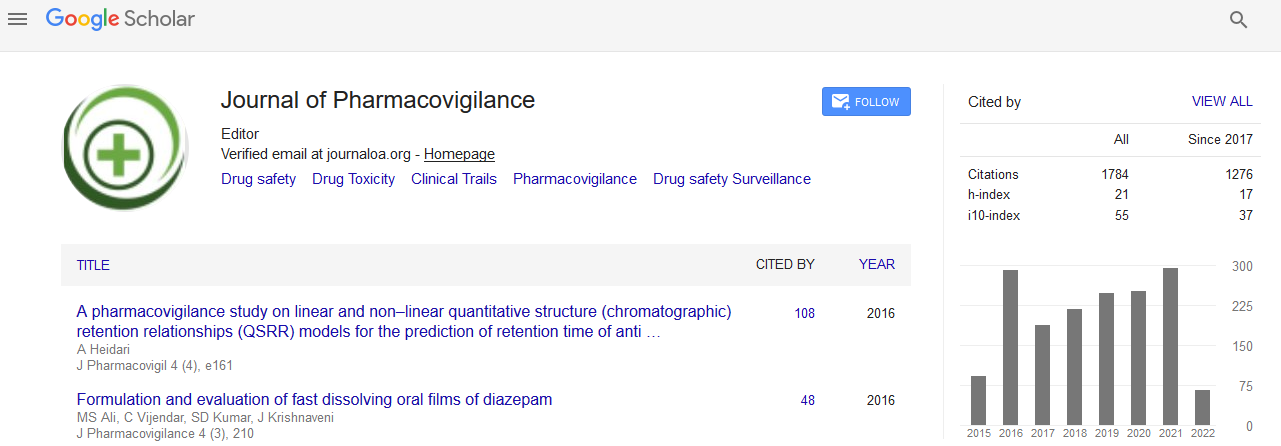
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
The influence of co-prescribed GABA-ergic drugs on anti-depressant compliance in patients with depression: A prospective study in a South African private healthcare cohort
4th International Conference and Exhibition on Pharmacovigilance & Clinical Trials
August 10-12, 2015 London, UK
Martie S Lubbe, Francois N Slabbert, Brian H Harvey and Christiaan B Brink
Posters-Accepted Abstracts: J Pharmacovigilance
Abstract:
Background: Despite the progress made in recent years regarding our understanding of the neurobiology of major depressive disorder (MDD), approximately one third of patients remain unresponsive to treatment. Co-prescribing of GABA-ergic drugs (GDs), such as sedative hypnotics, with antidepressants (ADs) is not uncommon, although how they benefit the outcome, if at all, remains controversial. Adequate compliance is central to a positive outcome, although its impact with respect to drug usage patterns has not been considered. The aim of the current study is to establish how the co-prescribing of GDs is associated with altered antidepressant compliance and which antidepressants (ADs) are associated with the worst compliance in combination with GDs. Methods: A prospective, cohort study design was used to analyse nationally representative medicine claims data submitted to a privately-owned South African Pharmaceutical Benefit Management (PBM) company. Three groups were distinguished over a six-year study period, namely patients treated only with ADs, those treated only with GDs and those treated with both ADs and GDs. The study population was determined by means of the following inclusion criteria: AD and/or GDs prescribed, patients older than 18 years, and MDD diagnosed by a psychiatrist supported by an appropriate ICD-10 code. The medicine possession ratio (MPR) was used as proxy to determine patient compliance for both AD and GD medication. Results: The overall AD compliance of patients taking both ADs and GDs (35.19% acceptable compliance; n=42869) was weak, and no statistically significant difference (p=0.657) was observed compared to patients taking only ADs (35.44% acceptable compliance; n=8247). The lowest percentage of patients taking amitriptyline (29.57%), mirtazapine (31.36%) and fluoxetine (32.29%) in addition with GDs were associated with compliance, with a higher percentage of duloxetine (40.67%), venlafaxine (38.62%), and citalopram (38.50%) that were compliant. ADs with the highest non-compliance were associated with a significant increase in GDs prescribing. Conclusion: The addition of GDs does not increase AD compliance. The class of AD is not always a risk factor for noncompliance. Different ADs show differences with respect to GD co-prescribing, which may be related to side effect burden and patient acceptability. Non-compliance and associated use of GD may correlate with ADS.
Biography :
Martie S Lubbe is currently the leader of the research niche area, Medicine Usage in South Africa (MUSA) at the North-West University (NWU), Potchefstroom campus in South Africa. She obtained her Bachelor?s, MPharm and PhD degrees in Pharmacy Practice at the Potchefstroom University for CHE. She has devoted 25 years of her career to pharmacy education and practice-related research and contributed significantly towards the development of Pharmacy practice. From 2004 to 2009 she acted as Subject Head of Pharmacy Practice at the NWU.