Analysis of Clinical Features, Biochemical and Inflammatory Indexes in Patients with Acute Pancreatitis
Received: 04-May-2024 / Manuscript No. DPO-24-134009 / Editor assigned: 07-May-2024 / PreQC No. DPO-24-134009 (PQ) / Reviewed: 23-May-2024 / QC No. DPO-24-134009 / Revised: 03-Jul-2025 / Manuscript No. DPO-24-134009 (R) / Published Date: 10-Jul-2025
Abstract
Background: Acute Pancreatitis (AP) is an inflammatory process unpredictability occurring in the pancreas, imposing a substantial burden on healthcare systems. Herein, exploring the clinical characteristics of patients with acute pancreatitis, biochemical tests and the role of inflammatory indexes in the disease, to predict the prognosis of acute pancreatitis.
Methods: We retrospectively analyzed the clinical data, biochemical and inflammatory indexes of 116 patients with acute pancreatitis diagnosed in Puren Hospital affiliated to Wuhan University of Science and Technology. They were divided into non-severe group and severe group. Counting data were expressed as rate (%), X2 test was used and measurement data were expressed as mean ± standard deviation. Comparison between the two groups was performed by t-test and comparison between the mean of more than two samples was performed by a one-way Analysis of Variance (ANOVA). P<0.05 was considered to be statistically significant. Receiver Operating Characteristic Curve (ROC) analysis was performed according to the inflammatory indexes of the two groups and the Area Under the Curve (AUC) and the Cut-Off value (CUT-OFF) are calculated respectively.
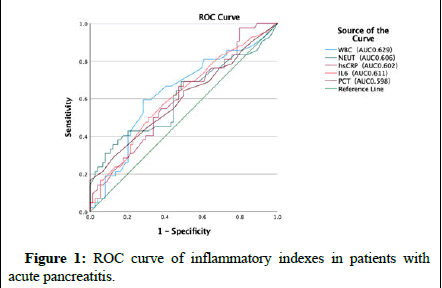
Results: The mean age of patients in the severe group was older and the proportion of underlying diseases was higher. The biochemical and inflammatory indexes in the severe group were higher than those in the non-severe group (P<0.05). The Area Under the Curve (AUC) and CUT-OFF value (cut-off) were obtained by ROC curve analysis of the inflammatory indexes of White Blood Cell count (WBC), Neutrophil Count (NEUT), hypersensitive CReactive Protein (hs-CRP), Procalcitonin (PCT) and Interleukin-6 (IL-6).
Conclusion: Elderly patients with acute pancreatitis accompanied by underlying diseases are more likely to develop into severe disease. In severe patients, biochemical tests are obviously abnormal and inflammatory indexes are increased or even excessive, which is helpful to judge the condition and prognosis of patients with acute pancreatitis.
Keywords: Acute pancreatitis; Inflammatory indexes; ROC curve; Area under the curve
Abbreviations
AP: Acute Pancreatitis; MAP: Mild Acute Pancreatitis; MSAP: Moderately Severe Acute Pancreatitis; SAP: Severe Acute Pancreatitis; RAP: Recurrent Acute Pancreatitis; CP: Chronic Pancreatitis; AMY: Amylase; FBG: Fasting Blood Glucose; FDP: Fibrin Degradation Products; ESR: Erythrocyte Sedimentation Rate; LDH: Lactate Dehydrogenase; ALT: Alanine Aminotransferase; CK-MB: Creatine Kinase Isoenzyme; HS-CRP: Hypersensitive C-reactive Protein; WBC: White Blood Cell Count; PCT: Procalcitonin; IL-6: Interleukin-6; ROC: Curve Receiver Operating Characteristic Curve; AUC: Area Under the Curve
Introduction
Pancreatitis is a complex, progressive and destructive inflammatory disease of the pancreas with a high risk of morbidity and mortality. Acute Pancreatitis (AP) has an estimated global incidence of 33.74 cases and 1.16 deaths per 100,000 person-years and ranks among the most common gastrointestinal cause of hospital admissions. Approximately 20% of patients with a first episode of AP develop Recurrent Acute Pancreatitis (RAP) and 3%-35% of patients will progress to Chronic Pancreatitis (CP) over 3-8 years. Globally, AP affects millions of individuals, with particularly severe cases causing major clinical and economic burdens in the United States. Despite considerable attempts, the pathogenesis of AP remains poorly understood.
Pancreatitis is a condition characterized by the inflammation of the pancreas due to the self‐digesting effect of digestive enzymes produced by the pancreas. Pancreatic damages occur including edema, congestion, bleeding and necrosis, leading to the symptoms of abdominal pain, bloating, nausea, vomiting, fever and other symptoms in the patients. The prognosis depends mainly on the development of organ failure and secondary infection with pancreatic or peripancreatic necrosis. Gallstones and alcohol abuse are the two most common causes of AP. With the significant increase in obesity in recent years, hypertriglyceridemia has become the third leading cause of AP. Despite significant improvements in the treatment and management of patients with SAP, the mortality rate remains high. Therefore, it is very important to study the pathogenesis of AP [1-4].
Over the past decade, immune system activation has been identified as a key trigger and regulator of inflammatory injury in the pancreas, affecting the extent of pancreatic necrosis, organ failure and disease deterioration. AP leads to overactivation of leukocytes and increased neutrophil metastasis to inflammation, with a consequent release of proinflammatory factors, including several forms of leukocyte interleukins, procalcitonin, transforming growth factor, and tumor necrosis factor. The study by Li et al., compared the performance of Interleukin-6 (IL-6) and Creactive Protein (CRP) as a potential predictor of SAP, organ failure, pancreatic necrosis, infected pancreatic necrosis and mortality. Their study revealed that IL-6 is a better predictor of mortality and infected pancreatic necrosis in AP. The level of Procalcitonin (PCT) is closely related to the degree of inflammation. Blood PCT may assess the clinically relevant pancreatic infections and overall prognosis in AP. Similarly, our study found that PCT was an independent risk factor of SAP. Despite recent treatment approaches such as the surgical and endoscopic step-up approaches that have been adopted in most practices, infected (peri-) pancreatic necrosis remains a challenge for clinicians [5-7].
The onset of acute pancreatitis is acute, rapid, with many complications and the mortality rate of patients with systemic complications is high. It is very important to take effective treatment measures according to the changes of the condition. Therefore, this study conducted a retrospective analysis of the clinical characteristics, biochemical tests and inflammatory indexes of acute pancreatitis patients admitted to Puren Hospital affiliated to Wuhan University of Science and Technology in recent years, in order to provide a theoretical basis for the early diagnosis, treatment and prognosis of acute pancreatitis.
Materials and Methods
General materials
Diagnosis of AP is based on clinical presentation, laboratory tests, and imaging findings and requires two out of the following three criteria to be present: Clinical (acute pain attack in the upper abdomen spreading to the back), laboratory (serum lipase and/or amylase levels are three or more times higher than normal values) and typical imaging (Computed Tomography (CT), magnetic resonance imaging, ultrasonography) findings that are characteristic for AP [8-12].
A total of 116 patients with acute pancreatitis admitted to the Department of Hepatobiliary Surgery, Puren Hospital Affiliated to Wuhan University of Science and Technology from January 1, 2018 to December 31, 2019 were collected as study subjects, including adult patients (≥ 18 and ≤ 80 years of age). There were 69 males with an average age of 52.55 ± 17.83 years and 47 females with an average age of 54.51 ± 17.50 years.
Clinical classification
Based on the severity of the disease, acute pancreatitis is divided into the following types;
• In Mild Acute Pancreatitis (MAP), there is the absence of local or systemic complications and organ failure.
• In Moderately Severe Acute Pancreatitis (MSAP) are local complications with or without organic failure for less than 48 hours.
• In Severe Acute Pancreatitis (SAP), there is persistent organ failure for more than 48 hours with the involvement of one or more than one organs. To facilitate the statistical study of clinical characteristics of patients, mild acute pancreatitis and moderate severe acute pancreatitis were classified as non-severe group and severe acute pancreatitis was classified as severe group.
Laboratory inspections
Collect the patient's laboratory test results. These include plasma Amylase (AMY), Lipase (LPS), Fasting Blood Glucose (FBG), Calcium (Ca), total Cholesterol (CHOL), Triglycerides (TG), Activated Coagulation Time (ACT), D-dimer (D-D), Fibrinogen (FIB), Fibrin Degradation Products (FDP), Erythrocyte Sedimentation Rate (ESR) and small blood Plate count (PLT), Hemoglobin (Hb), Creatinine (Cr), Urea nitrogen (Urea), Lactic Acid (LAC), Lactate Dehydrogenase (LDH), Alanine Aminotransferase (ALT), Aspartate Aminotransferase (AST), Creatine Kinase (CK), Creatine Kinase Isoenzyme (CK-MB). White Blood Cell Count (WBC), Neutrophil Count (NEUT), hypersensitive CReactive Protein (hs-CRP), Interleukin-6 (IL-6), Procalcitonin (PCT), etc. [13-16].
Statistical method
The statistical analysis was conducted using the SPSS 25.0 software. Counting data were expressed as rate (%), X2 test was used and measurement data were expressed as mean ± standard deviation. Comparison between the two groups was performed by t-test and comparison between the mean of more than two samples was performed by a one-way Analysis of Variance (ANOVA). P<0.05 was considered to be statistically significant. Receiver Operating Curve (ROC) analysis was performed according to the inflammatory indicators of the two groups and the Area Under the Curve (AUC) and the Cut-Off value (CUT-OFF) are calculated respectively.
Results
Clinical features
Among the 116 patients, 74 (63.7%) were in the non-severe group and 42 (36.2%) were in the severe group. The mean age of patients in the non-severe group was 52.22 ± 17.73 years old and that in the severe group was 59.71 ± 19.56 years old (P<0.05).
Etiology: The causes of 116 patients were as follows: Binge-eating 53 (45.6%), bile and pancreatic duct obstruction 34 (29.3%), hyperlipidemia 25 (21.5%) and other 4 (3.4%), P>0.05 compared between the two groups, the difference was not statistically significant.
General clinical symptoms: Among the 116 patients, there were 109 (93.9%) nausea and vomiting, 107 (92.2%) abdominal pain, 105 (90.5%) abdominal distension and 39 (33.6%) fever. Compared between the two groups, P<0.05, the difference was statistically significant.
Previous history: Hypertension in 17 cases (14.6%), coronary heart disease in 7 cases (6.0%), diabetes in 15 cases (12.9%), cerebrovascular disease in 11 cases (9.4%), chronic obstructive pulmonary disease in 4 cases (3.4%), liver disease in 13 cases (11.2%), kidney disease in 7 cases (6.0%). Compared between the two groups, patients with hypertension, diabetes, cerebrovascular disease, liver disease and kidney disease, P<0.05, the difference was statistically significant; patients with coronary heart disease and chronic obstructive pulmonary disease, P>0.05, the difference was not statistically significant (Table 1).
Laboratory inspection
Biochemical detection: AMY, LPS, FBG, Ca, CHOL, TG, D-D, ACT, FIB, FDP, ESR, LAC, LDH, ALT as well as AST, P<0.05. PLT, Hb, Cr, Urea, CK, as well as CK-MB, P>0.05, the difference was not statistically significant (Table 2).
Inflammatory indexes: Through the detection of WBC, NEUT, hsCRP, IL-6 and PCT, we found that the inflammatory indexes of all groups in the severe group were higher than those in the non-severe group and all were P<0.05 (Table 3).
ROC curve analysis: In this study, ROC curve analysis was performed on the inflammatory indexes: WBC, NEUT, hs-CRP, IL-6 and PCT and the CUT-OFF values of each inflammatory marks were 8.170, 9.455, 45.400, 8.530 and 1.000, respectively. The Area Under the Curve (AUC) was 0.629, 0.606, 0.602, 0.611 and 0.598 and the largest area under the curve was WBC (Figure 1).
| Parameter | Non-severe group (n=74) | Severe group (n=42) | χ2/t | P value |
| Male/Female (n) | 45/29 | 24/18 | 0.15 | 0.699 |
| Age (years) | 52.22 ± 17.73 | 59.71 ± 19.56 | 0.449 | 0.037 |
| Etiology (n (%)) | ||||
| Binge-eating | 32 (43.2%) | 21 (50.0%) | 0.493 | 0.483 |
| Bile and pancreatic duct obstruction | 22 (29.7%) | 12 (28.5%) | 0.017 | 0.895 |
| Hyperlipidemia | 17 (22.9%) | 8 (19.0%) | 0.244 | 0.621 |
| Other | 3 (4.0%) | 1 (2.3%) | 0.225 | 0.635 |
| General clinical symptoms (n (%)) | ||||
| Nausea and vomiting | 67 (90.5%) | 42 (100.0%) | 4.228 | 0.04 |
| Abdominal pain | 65 (87.8%) | 42 (100.0%) | 5.538 | 0.019 |
| Abdominal distension | 64 (86.4%) | 41 (97.6%) | 3.869 | 0.049 |
| Fever | 20 (27.0%) | 19 (45.2%) | 3.982 | 0.046 |
| Previous history (n (%)) | ||||
| Hypertension | 7 (9.4%) | 10 (23.8%) | 4.411 | 0.036 |
| Coronary heart disease | 3 (4.0%) | 4 (9.5%) | 1.414 | 0.234 |
| Diabetes | 6 (8.1%) | 9 (21.4%) | 4.222 | 0.04 |
| Cerebrovascular disease | 4 (5.4%) | 7 (16.6%) | 3.959 | 0.047 |
| Chronic obstructive pulmonary disease | 2 (2.7%) | 2 (4.7%) | 0.341 | 0.559 |
| Liver disease | 5 (6.7%) | 8 (19.0%) | 4.067 | 0.044 |
| Kidney disease | 2 (2.7%) | 5 (11.9%) | 4.001 | 0.045 |
| Note: Data are expressed as mean ± SD and percentage | ||||
Table 1: Comparison of clinical features in patients with acute pancreatitis (n (%)).
| Parameter | Non-severe group (n=74) | Severe group (n=42) | t | p value |
| AMY (U/L) | 493.42 ± 276.94 | 647.57 ± 403.65 | 4.091 | 0.017 |
| LPS (U/L) | 479.66 ± 258.29 | 651.69 ± 367.50 | 3.839 | 0.004 |
| FBG (mmol/L) | 7.00 ± 3.11 | 8.76 ± 4.54 | 7.379 | 0.015 |
| Ca (mmol/L) | 2.13 ± 0.22 | 2.03 ± 0.21 | 0.075 | 0.021 |
| CHOL (mmol/L) | 6.85 ± 2.77 | 8.03 ± 3.09 | 0.77 | 0.037 |
| TG (mmol/L) | 7.16 ± 2.87 | 8.57 ± 3.34 | 1.659 | 0.018 |
| D-D (ug/mL) | 3.75 ± 2.17 | 4.84 ± 3.04 | 9.336 | 0.027 |
| ACT (sec) | 135.45 ± 52.04 | 158.62 ± 57.45 | 0.292 | 0.028 |
| FIB (g/L) | 6.60 ± 2.52 | 7.91 ± 3.60 | 8.456 | 0.024 |
| FDP (ug/mL) | 8.08 ± 3.93 | 9.86 ± 3.97 | 0.142 | 0.022 |
| ESR (mm/h) | 20.01 ± 11.25 | 24.76 ± 9.63 | 5.63 | 0.023 |
| PLT (109/L) | 192.00 ± 104.03 | 218.36 ± 107.38 | 0.061 | 0.197 |
| Hb (g/L) | 123.34 ± 26.28 | 128.71 ± 27.68 | 0.248 | 0.301 |
| Cr (umol/L) | 94.03 ± 39.08 | 112.50 ± 77.17 | 6.555 | 0.09 |
| Urea (mmol/L) | 6.14 ± 2.94 | 7.13 ± 4.68 | 5.377 | 0.161 |
| LAC (nmol/L) | 2.46 ± 1.17 | 3.05 ± 1.63 | 15.581 | 0.026 |
| LDH (U/L) | 488.92 ± 277.06 | 618.83 ± 373.98 | 3.136 | 0.035 |
| ALT (U/L) | 74.77 ± 25.10 | 92.89 ± 53.35 | 8.482 | 0.014 |
| AST (U/L) | 56.70 ± 22.76 | 71.75 ± 52.09 | 5.149 | 0.033 |
| CK (U/L) | 95.19 ± 68.02 | 103.75 ± 74.62 | 0.717 | 0.531 |
| CK-MB (ng/mL) | 2.89 ± 1.22 | 3.24 ± 1.68 | 15.788 | 0.193 |
Table 2: Analysis of laboratory tests in patients with acute pancreatitis.
| Parameter | Non-severe group (n=74) | Severe group (n=42) | t | p value |
| WBC (109/L) | 8.55 ± 4.21 | 10.38 ± 4.63 | 1.745 | 0.032 |
| NEUT (109/L) | 5.30 ± 3.21 | 6.77 ± 3.77 | 1.141 | 0.028 |
| hs-CRP (mg/L) | 46.44 ± 30.71 | 64.52 ± 57.41 | 4.172 | 0.029 |
| IL-6 (pg/mL) | 7.92 ± 4.06 | 9.70 ± 5.02 | 3.079 | 0.04 |
| PCT (ng/mL) | 0.38 ± 0.35 | 0.59 ± 0.55 | 10.348 | 0.011 |
Table 3: Analysis of laboratory inflammation indexes in patients with acute pancreatitis.
Figure 1: ROC curve of inflammatory indexes in patients with acute pancreatitis.
Discussion
Current literature on temporal trends reveals that the incidence of acute pancreatitis has been increasing globally over the past 20 years, with average annual per cent changes of 3.67 and 2.77% across North America and Europe, respectively. Acute Pancreatitis (AP) is among the most common clinical digestive system diseases. It is an inflammatory disease caused by the abnormal activation of pancreatic enzymes, leading to the digestion of pancreatic tissues. AP has a rapid onset and progression and can develop into Moderately Severe Acute Pancreatitis (MSAP) or Severe Acute Pancreatitis (SAP), which has many complications, dangerous conditions and high mortality [17-20].
Mortality for pancreatitis is approximately 1% overall, however, among hospitalized patients with pancreatitis and organ failure or pancreatic necrosis, mortality may be as high as 30%-40%.
Thus, active research into the microscopic mechanisms of immune imbalance and inflammatory amplification in SAP is essential for improving its prognosis. Pathology of AP begins with the early conversion of pancreatic enzymes from inactive to active forms inside the acinar cells which leads to auto digestion of the pancreatic tissue. On a molecular level, the triggers of acute pancreatitis induce injury of pancreatic acinar and ductal cells by disrupting normal intracellular calcium signaling that maintains stimulus-secretion coupling. Due to the limited understanding of AP pathophysiology, the treatment of this disease remains not specific. Hence, it is vitally important to investigate the mechanism underlying AP to find novel therapeutic strategy.
The main causes of acute pancreatitis in high-income countries are gallstones (45%), alcohol use (20%) and hypertriglyceridemia (10%). In this study, the three major causes of binge-eating, biliary and pancreatic duct obstruction, and hyperlipidemia were basically consistent with the above studies. AP is a common clinical acute abdominal disease with pancreatic inflammation, including pancreatic edema, bleeding and even necrosis. The clinical features of AP are acute epigastric pain, nausea, vomiting, fever and even slipping into shock. The mean age of participants was 45.3 ± 8.7 years and 82.7% were male. Abdominal pain was the most frequent clinical sign (100%), followed by dyspepsia (87.7%), nausea or vomiting (72.8%) and a bloated stomach (61.7%). Our statistical analysis of the general clinical symptoms of acute pancreatitis, including nausea, vomiting, abdominal pain, abdominal distension and fever, it was found that the severe group was significantly higher than the non-severe group (P<0.05). Meanwhile, the history of hypertension, diabetes, cerebrovascular disease, liver disease and kidney disease in the severe group was higher than that in the non-severe group (P<0.05). This indicates that those with underlying diseases are more likely to develop acute severe pancreatitis than previously healthy ones.
Because of the relative inaccessibility of pancreatic tissue and the rapid course of AP, obtaining blood samples seems advantageous for establishing early diagnosis. At present, there is no gold standard laboratory test for diagnosing AP and serum lipase activity at least three times greater than the upper limit is often adopted to assess pancreatic inflammation. However, these biomarkers have not been incorporated into clinical use for various reasons, such as their low diagnostic accuracy and availability. In our laboratory analysis of acute pancreatitis, we found that: Serum amylase, lipase, fasting blood glucose, calcium, total cholesterol, triglyceride, activated coagulation time, D-dimer, fibrinogen, fibrin degradation products, erythrocyte sedimentation rate, lactic acid, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, etc., were significantly increased in severe group compared with non-severe group (P<0.05). D-dimer is a specific product of degradation of crosslinked fibrin, which indirectly reflects the coagulation disorder. Some studies have found that D-dimer is related to the severity and complications of acute pancreatitis and patients with acute pancreatitis may develop coagulation and microcirculation disorders in the acute phase. In the present study, the plasma levels of D-dimer in patients with AP, Recurrent Acute Pancreatitis (RAP) and Chronic Pancreatitis (CP) were measured. Subsequently, correlations between D-dimer levels and diferent types of pancreatitis were assessed. In diferent types of pancreatitis, D-dimer levels in AP patients and RAP patients were signifcantly higher than those in control group (p<0.05), and there was no signifcant diference in D-dimer levels between CP group and control group. Clinical studies revealed that the levels of plasma Fibrinogen Degradation Products (FDP) are significantly higher in AP patients compared to healthy individuals and higher levels of FDP are related to severity and portosplenomesenteric venous thrombosis occurs in about 17.86% of patients with early-stage SAP. These phenomena indicated that the hypercoagulable state during AP and the therapeutic strategies aimed at enhancing microcirculation by anticoagulant therapy might improve the outcomes in AP. Acute pancreatitis is a procoagulant state. The leakage of activated digestive enzymes from damaged pancreatic acinar cells results in injury to the adjacent vascular epithelial cells, leading to the exposure of tissue factor, activation of platelets and the initiation of the coagulation cascade.
Clinical study found that AP patients with complications, such as pseudocyst, acute respiratory failure, sepsis, infectious pancreatic necrosis and acute renal failure had significantly increased inflammatory indicators, such as WBC, neutrophils, CRP and ESR, while RBC, Hb decreased significantly, indicating that the pathological basis of AP complications is an inflammatory response and malnutrition and ischemia and hypoxia may further aggravate this inflammatory response. Animal studies have shown that cells of the innate immune response, such as neutrophils and macrophages rapidly migrate into the pancreas after the onset of the disease. Understanding the precise roles of these immune cells in AP will help develop targeted therapeutic strategies to modulate the immune response and improve patient outcomes. Further research is needed to elucidate the roles of these immune cells in the development of AP and to evaluate the potential of targeting specific immune cell populations for treating this complex and severe inflammatory disorder. Neutrophils can not only produce a large number of reactive oxygen species and reactive nitrogen, leading to worsening inflammation, but can also activate various immune cells and stromal cells to secrete inflammatory cytokines, leading to aggravation of inflammation. The CRP can also be applied as both an inflammatory mediator and a nonspecific sensitive indicator of the immune inflammation. Several biological markers have been proposed for the prediction of the severity and mortality of acute pancreatitis. These results suggest that CRP can be used to select mild cases of acute pancreatitis which can be discharged early and managed in an ambulatory setting. Other proposed markers were the white blood cell count, neutrophil number, erythrocyte sedimentation rate, and Hb level. C-Reactive Protein (CRP) levels above 150 mg/dL predict severe Acute Necrotizing Pancreatitis (ANP) on admission. Procalcitonin (PCT) above 0.5 ng/mL is a predictor of ANP from the first twenty-four hours. Serial assessment of changes in PCT reflects the course of the disease. Levels above 1.8 ng/mL are an indication of infected ANP. Lactate levels greater than 2 mmol/L (>18 mg/dL) indicate severe sepsis. Both IL-6 and CRP are known as inflammatory markers that predict severe AP and are useful in the early phase of AP. IL-6 is a prototypical cytokine that has redundant and pleiotropic activity, the synthesis of which is promptly induced to aid in host defense when tissue damage or inflammation because of infections or injuries occurs. Several studies have demonstrated an association between IL-6 and AP and found that IL-6 is a useful marker for the assessment of the severity of AP in its early stages. In the analysis of laboratory inflammation indicators of acute pancreatitis, we found that the leukocyte count, neutrophil count, hypersensitive C-reactive protein, interleukin-6, procalcitonin, etc., were significantly higher in the severe group than in the non-severe group (P<0.05). ROC curves can be used to improve clinical care by determining both cut of points and the best performing diagnostic tests. In this study, ROC curve analysis was performed on the inflammatory indexes: WBC, NEUT, hs-CRP, IL-6 and PCT and the CUT-OFF values of each inflammatory indicator were 8.170, 9.455, 45.400, 8.530 and 1.000, respectively. The Area Under the Curve (AUC) was 0.629, 0.606, 0.602, 0.611 and 0.598 and the largest area under the curve was WBC. The AUC is a measure of the overall performance of a diagnostic test and can be interpreted as the average value of sensitivities for all possible specificities. The AUC has a value between 0 and 1, but is meaningful as a diagnostic test only when it is >0.5. The larger the value, the better the overall performance of the test.
In summary, through the analysis of clinical characteristics and inflammatory indicators of 116 patients with acute pancreatitis in this paper, it is concluded that patients in the severe and non-severe groups have significant differences in age, underlying diseases, biochemistry, inflammatory indicators and clinical manifestations, which is conducive to early clinical detection, diagnosis, treatment and prevention in the future and to reduce mortality to a certain extent. Improve the quality of life and prognosis of patients and play a positive role in further standardizing the clinical diagnosis and treatment of AP.
In addition, this study is limited to retrospective studies, and there are still some limitations in evaluating the severity and prognosis of AP patients. First of all, this study is a single-center, small-sample study, which may cause statistical deviation due to sample size. Secondly, the course of acute pancreatitis is extremely complicated and the peripheral blood indexes change significantly at different time points and the results of a single blood collection have a certain chance. In the future, multi-source, multi-center, prospective and reproducible clinical data are still needed to verify its reliability.
Conclusion
Through this study, we found that elderly patients with acute pancreatitis accompanied by underlying diseases are more likely to develop into severe disease. In severe patients, biochemical tests are obviously abnormal and inflammatory indexes are increased or even excessive, which is helpful to judge the condition and prognosis of patients with acute pancreatitis.
Acknowledgements
The subjects of this study came from the Department of Hepatobiliary Surgery, Puren Hospital Affiliated to Wuhan University of Science and Technology. We sincerely thank Dr. Jiang Fan and his colleagues in the Department of Hepatobiliary Surgery for their strong support in data collection, laboratory testing and clinical data.
Authors’ Contributions
Minghua Han has given substantial contributions to the conception of the design of the manuscript. Jun Jiang and Lei Huang contributed to the acquisition, analysis and interpretation of the data. All authors have participated in drafting the manuscript, Minghua Han revised it critically. All authors read and approved the final version of the manuscript.
Funding
No founding.
Availability of Data and Materials
The datasets are not publicly available due to privacy or ethical restrictions but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study protocol was reviewed and approved by Wuhan Puren Hospital Ethical Board (LLSC-20240318001). Because all data were provided by the data base retrospectively, informed consent of the participants was not required.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
References
- Mao X, Huang C, Wang Y, Mao S, Li Z, et al. (2023) Association between dietary habits and pancreatitis among individuals of European ancestry: A two-sample Mendelian randomization study. Nutrients 15: 1153.
[Crossref] [Google Scholar] [PubMed]
- Wu H, Chen H, Zhou R (2023) Phospholipase D2 targeted by miR‐5132‐5p alleviates cerulein‐induced acute pancreatitis via the Nrf2/NFκB pathway. Immun Inflamm Dis 11: e831.
[Crossref] [Google Scholar] [PubMed]
- Ma Y, Liu L, Li B, Wang W, Zhao T (2022) Cdk2 suppresses IL‐23 expression and the onset of severe acute pancreatitis. Immun Inflamm Dis 10: e631.
[Crossref] [Google Scholar] [PubMed]
- Li H, Wu D, Zhang H, Li P (2023) New insights into regulatory cell death and acute pancreatitis. Heliyon 9: e18036.
[Crossref] [Google Scholar] [PubMed]
- Li G, Chen H, Liu L, Xiao P, Xie Y, et al. (2021) Role of interleukin-17 in acute pancreatitis. Front Immunol 12: 674803.
[Crossref] [Google Scholar] [PubMed]
- Hong W, Pan J, Goyal H, Zippi M (2023) Acute pancreatitis infection: Epidemiology, prevention, clinical characteristics, treatment, and prediction. Front Cell Infect Microbiol 13: 1175195.
[Crossref] [Google Scholar] [PubMed]
- Yin Y, Wei N, Zheng Z, Liang H (2022) Relationship between apoA-I, chemerin, Procalcitonin and severity of hyperlipidaemia-induced acute pancreatitis. J Pak Med Assoc 72: 1201-1204.
[Crossref] [Google Scholar] [PubMed]
- Li X, Zhang Y, Wang W, Meng Y, Chen H, et al. (2024) An inflammation-based model for identifying severe acute pancreatitis: A single-center retrospective study. BMC Gastroenterol 24: 63.
[Crossref] [Google Scholar] [PubMed]
- van den Berg FF, Boermeester MA (2023) Update on the management of acute pancreatitis. Curr Opin Crit Care 29: 145-151.
[Crossref] [Google Scholar] [PubMed]
- Zerem E, Kurtcehajic A, Kunosić S, Malkočević DZ, Zerem O (2023) Current trends in acute pancreatitis: Diagnostic and therapeutic challenges. World J Gastroenterol 29: 2747.
[Crossref] [Google Scholar] [PubMed]
- Redman I, Panahi P, Bananis K, Drymousis P (2024) Therapeutic anticoagulation in patients with acute pancreatitis and splanchnic vein thrombosis: A best evidence topic. Ann Med Surg (Lond) 86: 271-278.
[Crossref] [Google Scholar] [PubMed]
- Liu C, Shi Q, Zhang X, Xue E, Li H, et al. (2023) Incidence and risk factors of fasting hyperglycaemia following first-attack acute pancreatitis before discharge: A retrospective study. BMC Gastroenterol 23: 203.
[Crossref] [Google Scholar] [PubMed]
- Iannuzzi JP, King JA, Leong JH, Quan J, Windsor JW, et al. (2022) Global incidence of acute pancreatitis is increasing over time: A systematic review and meta-analysis. Gastroenterology 162: 122-134.
[Crossref] [Google Scholar] [PubMed]
- Wang Z, Liu J, Wang Y, Guo H, Li F, et al. (2023) Identification of key biomarker associated with immunogenic cell death and their regulatory mechanisms in severe acute pancreatitis based on WGCNA and machine learning. Int J Mol Sci 24: 3033.
[Crossref] [Google Scholar] [PubMed]
- Werawatganon D, Vivatvakin S, Somanawat K, Tumwasorn S, Klaikeaw N, et al. (2023) Effects of probiotics on pancreatic inflammation and intestinal integrity in mice with acute pancreatitis. BMC Complement Med Ther 23: 166.
[Crossref] [Google Scholar] [PubMed]
- Szatmary P, Grammatikopoulos T, Cai W, Huang W, Mukherjee R, et al. (2022) Acute pancreatitis: Diagnosis and treatment. Drugs 82: 1251-1276.
[Crossref] [Google Scholar] [PubMed]
- Chen H, Tu J, He L, Gao N, Yang W (2023) Mmu_circ_0000037 inhibits the progression of acute pancreatitis by miR‐92a‐3p/Pias1 axis. Immun Inflamm Dis 11: e819.
[Crossref] [Google Scholar] [PubMed]
- Sarshari B, Zareh-Khoshchehreh R, Keshavarz M, Manshadi SA, SeyedAlinaghi S, et al. (2023) The possible role of viral infections in acute pancreatitis: A review of literature. Gastroenterol Hepatol Bed Bench 16: 270-281.
[Crossref] [Google Scholar] [PubMed]
- Zhang D, Wang M, Zhang Y, Xia C, Peng L, et al. (2022) Novel insight on marker genes and pathogenic peripheral neutrophil subtypes in acute pancreatitis. Front Immunol 13: 964622.
[Crossref] [Google Scholar] [PubMed]
- Nguyen DC, Nguyen NA, Dinh QK, Le DT, Vu TB, et al. (2023) Effect of plasma exchange treatment in patients with hypertriglyceridemia-induced acute pancreatitis. Medicina (Kaunas) 59: 864.
[Crossref] [Google Scholar] [PubMed]
Citation: Han M, Jiang J, Huang L (2025) Analysis of Clinical Features, Biochemical and Inflammatory Indexes in Patients with Acute Pancreatitis. Diagnos Pathol Open 10: 254.
Copyright: © 2025 Han M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 151
- [From(publication date): 0-0 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 98
- PDF downloads: 53