PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
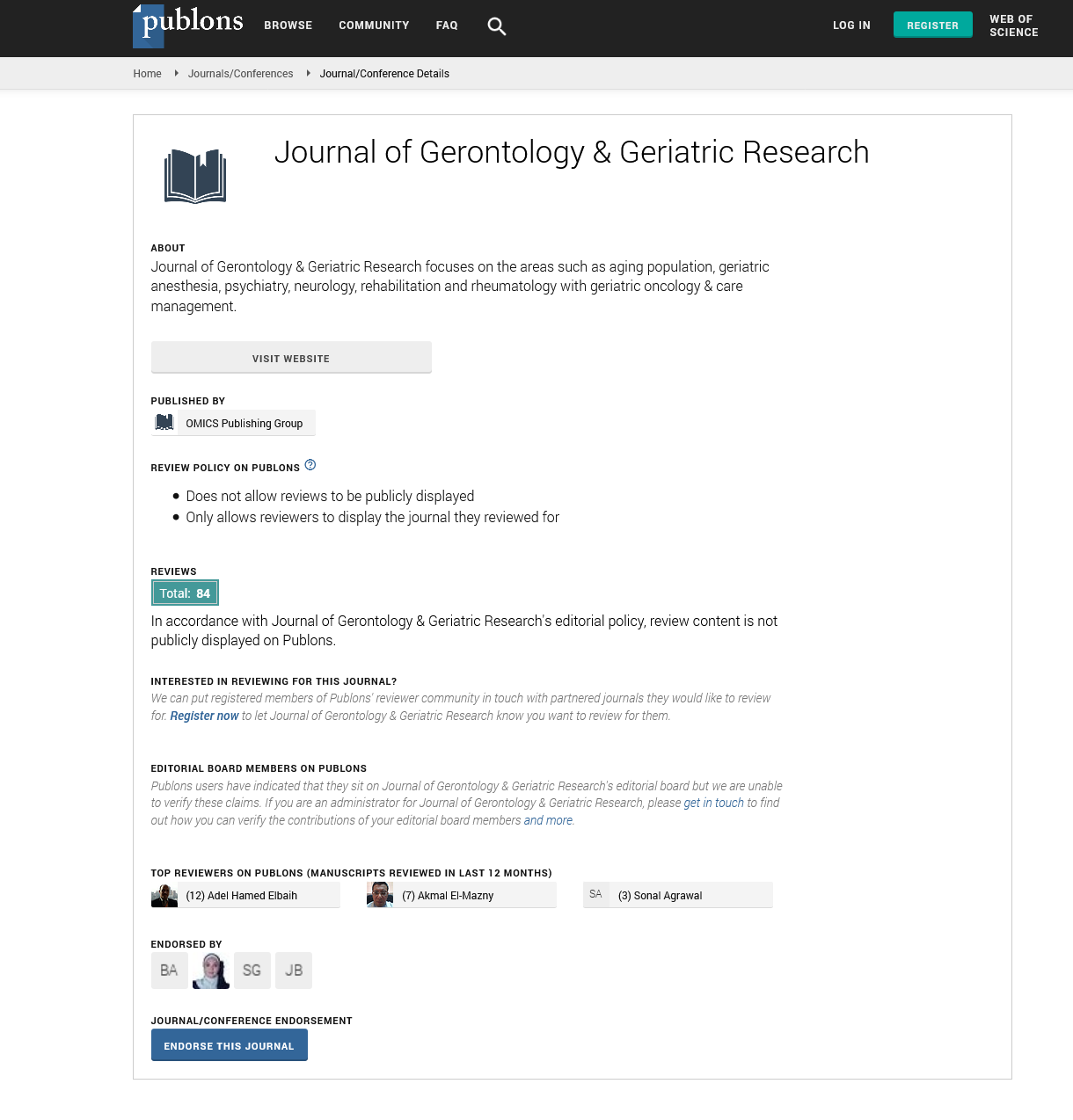
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
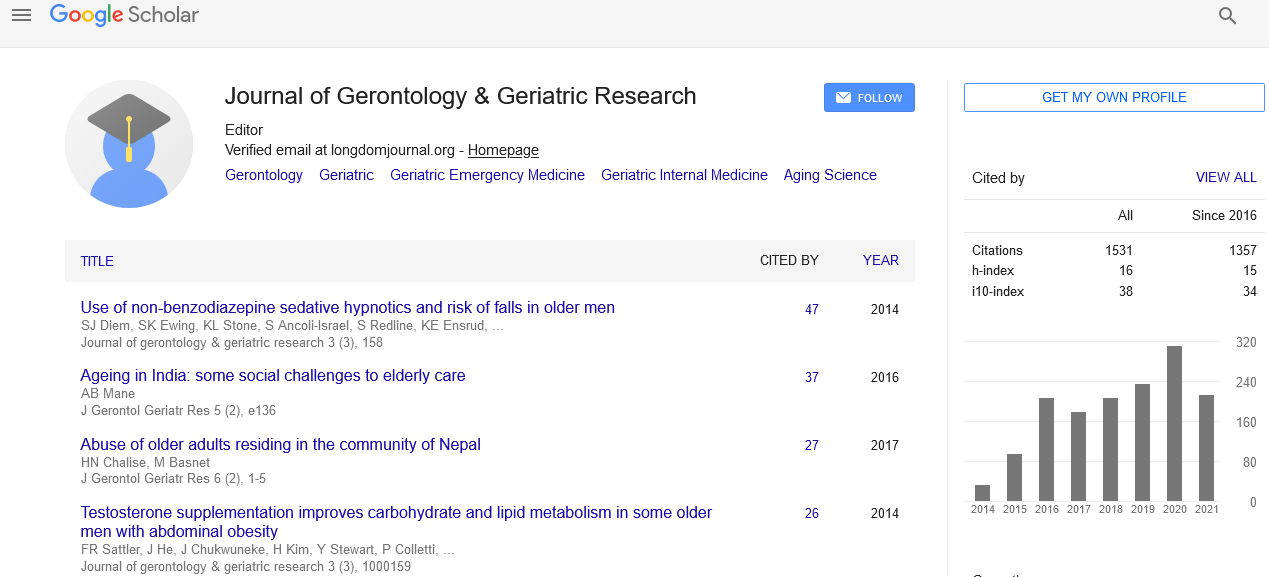
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Antihypertensive Drugs in the Elderly: Risks and Benefits as Evaluated by the FORTA Method
The management of polypharmacy in the elderly is a growing concern worldwide. Taking multiple medications can cause more harm than good, given that an estimated 100,000 medication-related deaths occur in the U.S. annually. Specific criteria were established by Beers (1997) for drugs to avoid in elderly patients. Although widely used, no clinical endpoints were improved, thus stressing the need for additional positive labeling of drugs as data on morbidity, mortality and safety become available for this patient collective. The FORTA (Fit fOR The Aged) method is the first approach combining positive and negative labeling of drugs. Class A drug is indispensable, B drugs have some restrictions, and C drugs are critical and need careful balancing of desired/undesired effects. D drugs should generally be avoided. Commonly-used medications for major diseases, among them hypertension, were assigned these labels in the FORTA list according to evidence as to age-appropriateness by an expert panel in a Delphi Consensus Procedure. In hypertension, RAS-inhibitors and long-acting dihydropyridine calcium blockers are A drugs, diuretics and beta blockers B drugs. This means that uncomplicated hypertension is preferentially treated by A drugs, B drugs are only given if A drugs are exhausted. C drugs represent second line compounds such as moxonidine or spironolactone which are difficult to use. The D drugs clonidine or verapamil should be avoided in the elderly. Use of the FORTA list will support general practitioners struggling with polypharmacy with multiple diagnoses, as prioritization is possible not only for one disease, but also across therapeutic areas.