Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Euro Pub
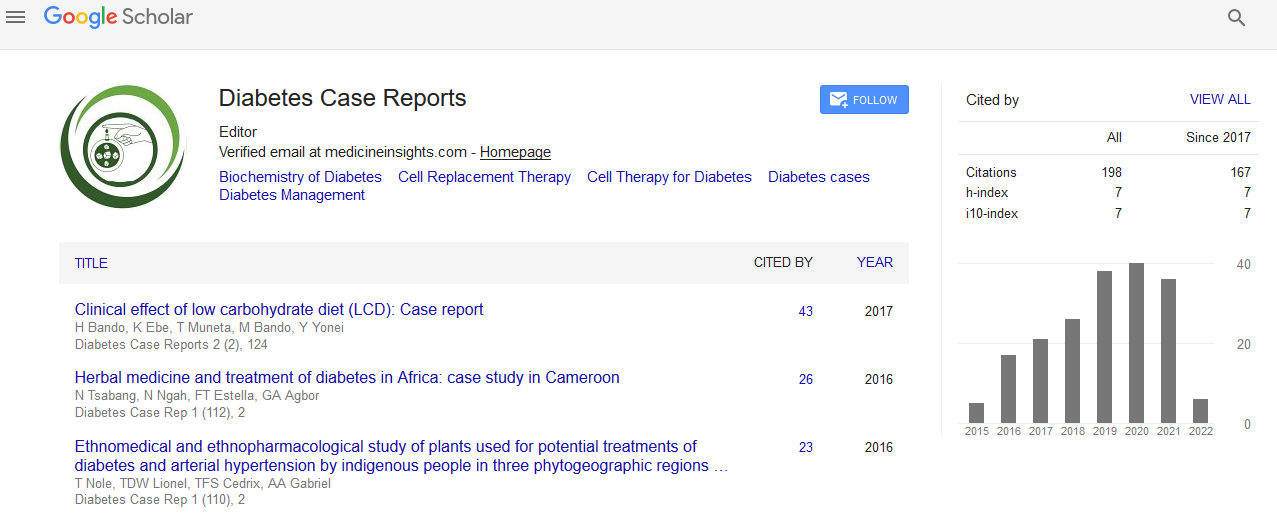
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Diabetes Mellitus and Polycystic Ovary Syndrome: Beyond A Dermatological Problem
Ana Raquel Marques, Carla Silva, Sílvia Colmonero and Pedro Andrade
Background and aim: Polycystic ovarian syndrome is a common endocrine disorder in reproductive age, with unknown etiology and a variable clinical presentation. Recognizing polycystic ovary syndrome in women presenting with oligo-ovulation and hyperandrogenism offers an important opportunity to begin a life-long conversation about prevention and treatment of a condition that has a multi-system impact on affected women. Recognition offers the chance for providers and patients to engage in discussions about prevention and early treatment of metabolic derangements. This review aims to review the polycystic ovarian syndrome and the approach to the metabolic complications such as insulin resistance and associated hyperinsulinemia. Methods: It was performed a research on PubMed database of English and Portuguese publications (2004-2015), using the terms: ?Polycystic Ovary Syndrome?, ?Dermatological manifestations? and ?Diabetes Mellitus?. Review: Hyperandrogenism occurs in 60% to 80% with PCOS and presents with the following: hirsutism, acne and androgenetic alopecia. Metabolic complications are common, such as obesity, insulin resistance, dyslipidemia and high blood pressure. Thus, lifestyle modifications are essential and metformin or thiazolidinediones can be used. The combined hormonal contraception is the first-line treatment, being more effective with progestins with anti-androgenic activity. Antiandrogens may be used, too. Metformin and weight loss can improve ovulation rate. Conclusion: It emphasizes the importance of early diagnosis and treatment, in order to prevent metabolic complications and the emotional impact associated with skin manifestations. The family doctor plays a key role in early diagnosis and managing the recommended multidisciplinary approach, including dermatology, endocrinology, obstetrics-gynecology, nutrition and psychology.