PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Directory of Research Journal Indexing (DRJI)
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
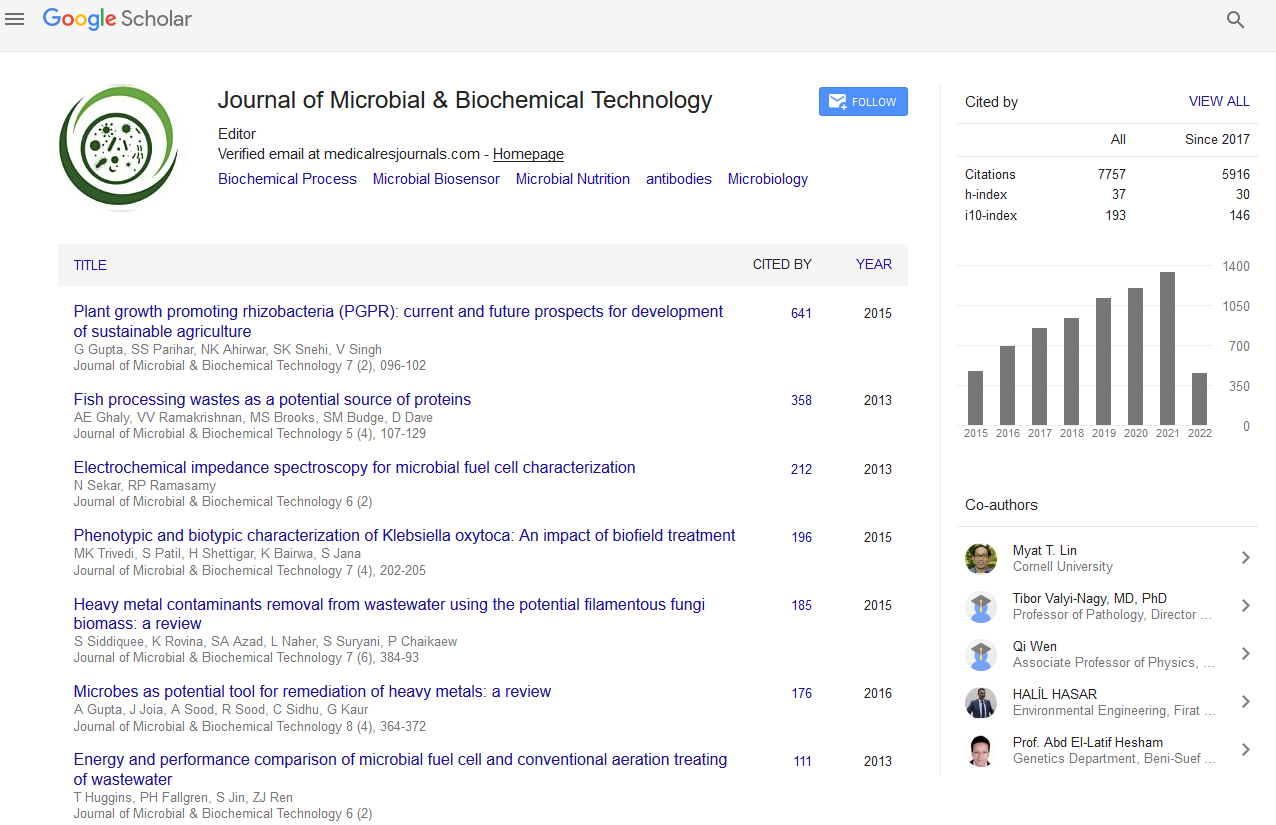
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Overcoming Pseudomonas aeruginosa Resistance Caused by Glycocalyx with Tobracef
Manu Chaudhary, Renu Bansal and Anurag Payasi
The present study was aimed to compare the binding ability of selected chemicals (adjuvants) in 23 glycocalyx positive Pseudomonas aeruginosa isolates. Fractional inhibitory concentration indexes (FICindex) and drug uptake study were conducted using selected adjuvants. Whole-cell alkaline phosphatase assay was used for assessment of outer membrane permeability. FICindex was calculated using a microdilution checkerboard method. Among the drugs tested, Tobracef was found to be the most effective against all the selected clinical isolates with minimum inhibitory concentrations (MICs) of about 8-16 μg/ml. Tobracef without adjuvants showed drug uptake of approximately 85.3%. When Tobracef was combined with either adjuvant CH1 or adjuvant CH2 the drug uptake was increased to 90.6% and 94.8% respectively but this increase was not statistically significant (P>0.05). The drug uptake of other comparator drugs including ceftazidime, tobramycin, amikacin, gentamycin, ceftazidime plus amikacin without adjuvants varied from 14 to 34%. Addition of adjuvant CH2 and adjuvant CH1with these drugs enhanced the drug uptake by 8 to 11% and 11 to 22%, respectively which was statistically significant (P<0.01 with adjuvant CH2 and P<0.001 with adjuvant CH1). Tobracef without adjuvants showed maximum outer membrane permeability with 8.5 ± 0.70 permeability index at 8 hrs. Addition of adjuvant CH2 or adjuvant CH1 into Tobracef produced 9.1 ± 0.71 and 9.5 ± 0.98 permeability index which was statistically non-significant (P>0.05). Other comparator drugs exhibited a very low (only 2.4 to 3.5) permeability index and incorporation of adjuvant CH2 and adjuvant CH1 enhanced significantly the permeability index (P<0.01 with adjuvant CH2 and P<0.001 with adjuvant CH1). Interestingly, all the drugs showed additive effects when tested with both the adjuvants. However the exact mechanism of high membrane permeability of Tobracef is not known which needs to be explored. Thus, Tobracef is effective in dealing resistance from P. aeruginosa by increasing permeability and susceptibility towards P. aeruginosa.