Indexed In
- Genamics JournalSeek
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
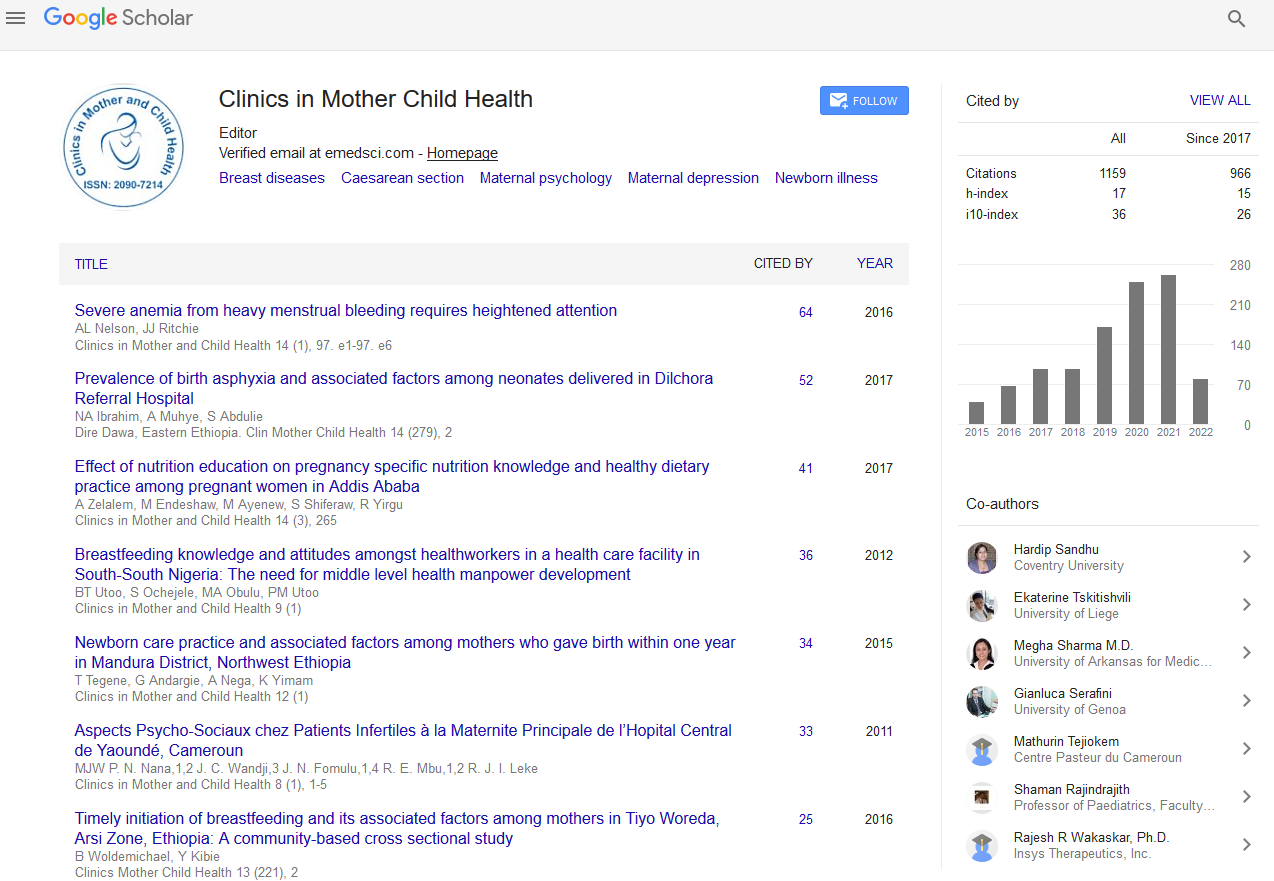
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Factors Associated with Maternal and Child Health Services Uptake and Their Association with Health Outcomes in Mashonaland East, Zimbabwe
Maxwell Mhlanga, Zvinavashe M, Gwanzura L and Babill Stray-Pedersen
This study aimed at determining the factors associated with maternal and child health services uptake and their association with maternal and child health outcomes.
Design and setting: The study was conducted in two districts in Mashonaland East namely Murewa and Seke in Zimbabwe. An analytical cross sectional study design was conducted between November 2016 and March 2017. Women with children 0-48 months who were being recruited for an interventional study were targeted with an aim of determining the baseline characteristics and comparability of participants in the intervention and control arm. A sample of 672 mothers was interviewed. Data was analyzed in SPSS version 20 and STATA 13.
Main outcome(s): The study focused on maternal and child health outcomes.
Results: The mean age for the women was 28.0 years (SD=6.8) and the mean birth weight for children was 3061 g (SD=537). Women had a mean weight of 62.5 kg (SD=11.5) and the mean number of children per woman were 2.6 (SD=1.5). In this study 154 (22.9%) of the participants booked for Antenatal Care (ANC) in the first trimester and 321 (47.7%) and 171 (25.4%) booking in the second and third trimester respectively. There was a statistically significant association between a child’s gestational age and birth weight (OR=2.14; 95% CI: 1.22-3.75). Maternal complications were significantly associated with the number of children delivered prior to the last pregnancy (OR=4.4; 95% CI: 2.45- 8.04). First ANC timing was strongly associated with the place of delivery (OR=2.84, 95% CI: 1.53-5.25) and so was ANC registration decision making (OR=3.52; 95% CI: 1.88-6.58). The weaning time was significantly associated with child morbidity (OR=5.28; 95% CI: 2.57-9.86).
Conclusion: This study revealed that though there is a satisfactory health seeking behavior among pregnant and lactating women, there is still a significant gap in knowledge of critical recommended Maternal Neonatal and Child Health (MNCH) practices. Good knowledge and practices are essential in the reduction of preventable maternal and child morbidity and mortality. Universal maternal health access is only achievable if the women and the community take decisions about their own health in a supportive environment; hence the need to have community based interventions for maternal health access. The results of the study have shown that the quality and methods of delivery of antenatal care education need to reviewed to improve effectiveness of antenatal care.