PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Academic Keys
- JournalTOCs
- ResearchBible
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
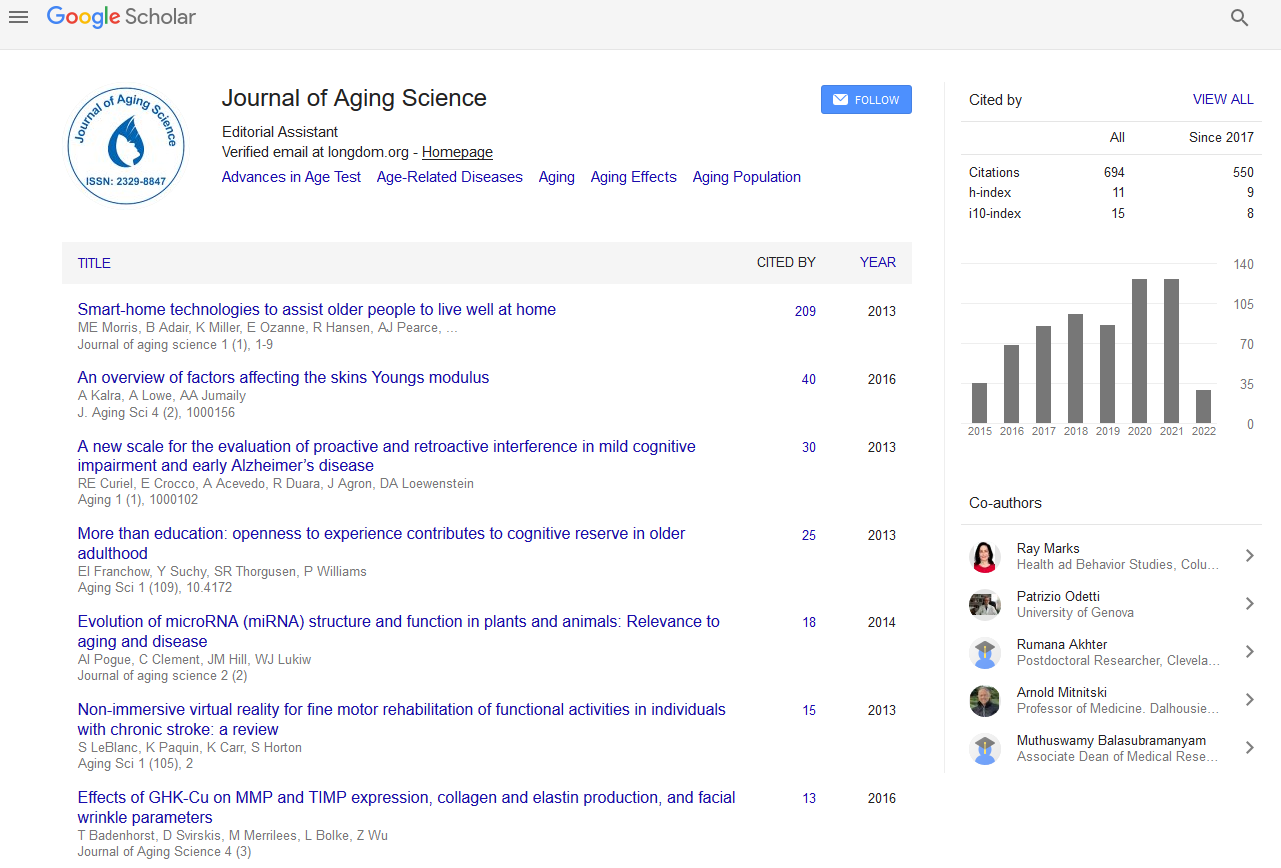
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Relationship between Hemorrhagic Stroke and Mortality in Chronic Complex Outpatients: Results from a Community Cohort of Patients
González-Henares MA, Clua-Espuny JL, Queralt-Tomas MLL, Campo-Tamayo W, Muria-Subirats E, Panisello-Tafalla A, Lucas-Noll J, Forcadell-Arenas T and Gil-Guillen VF
Question: Around 3-5% of people can be identified as chronic complex patients(CCP) and are increasingly at risk of hemorrhagic stroke.The main objective was to explore differences in risk factors and the association with outcome factors on mortality.
Materials and Methods: Multicenter and prospective cohort study from January 1 2013 to September 30 2016 among patients registered as chronic complex outpatients. To predict hazard ratios, mean survival time, and survival probabilities, multivariate Cox regression was used.
Results: 932 CCP were included (52.3% women). Average age was 82.5 years (95% CI 81.8-83.2). During a mean follow-up period of 2.8 years, 65 (6.98%) stroke episodes happened (37 (56.9%) ischemic; 28 (43.1%) hemorrhagic). The percentage of ICH almost doubled (21.0% to 43.1) after CCP diagnosis; 26.1% had polypharmacy (≥ 10), 57.6% VKA-treated patientsshowed TTR <60%, and had a higher incidence of falling (31.9% vs. 19.2%, p 0.002).The average survival time was significantly shorter associated with age (HR 1.03 95% CI 1.14-1.53, p 0.001), previous stroke (HR 13.54 95%, CI 9.23-19.81, p<0.001), antiagreggant treatment (HR 1.97 95% CI 1.21-3.21, p 0.006), anticoagulant treatment (HR 1.78 95%, CI 1.22-2.60, p 0.002), and Barthel score <60 (HR 1.43 95% CI 1.04-1.97, p 0.024).
Conclusions: Given the co-occurrence of hemorrhagic strokes with poor performance status, multi-morbidity, and polypharmacy, multi-dimensional interventions are needed to improve health outcomes.