PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Proquest Summons
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
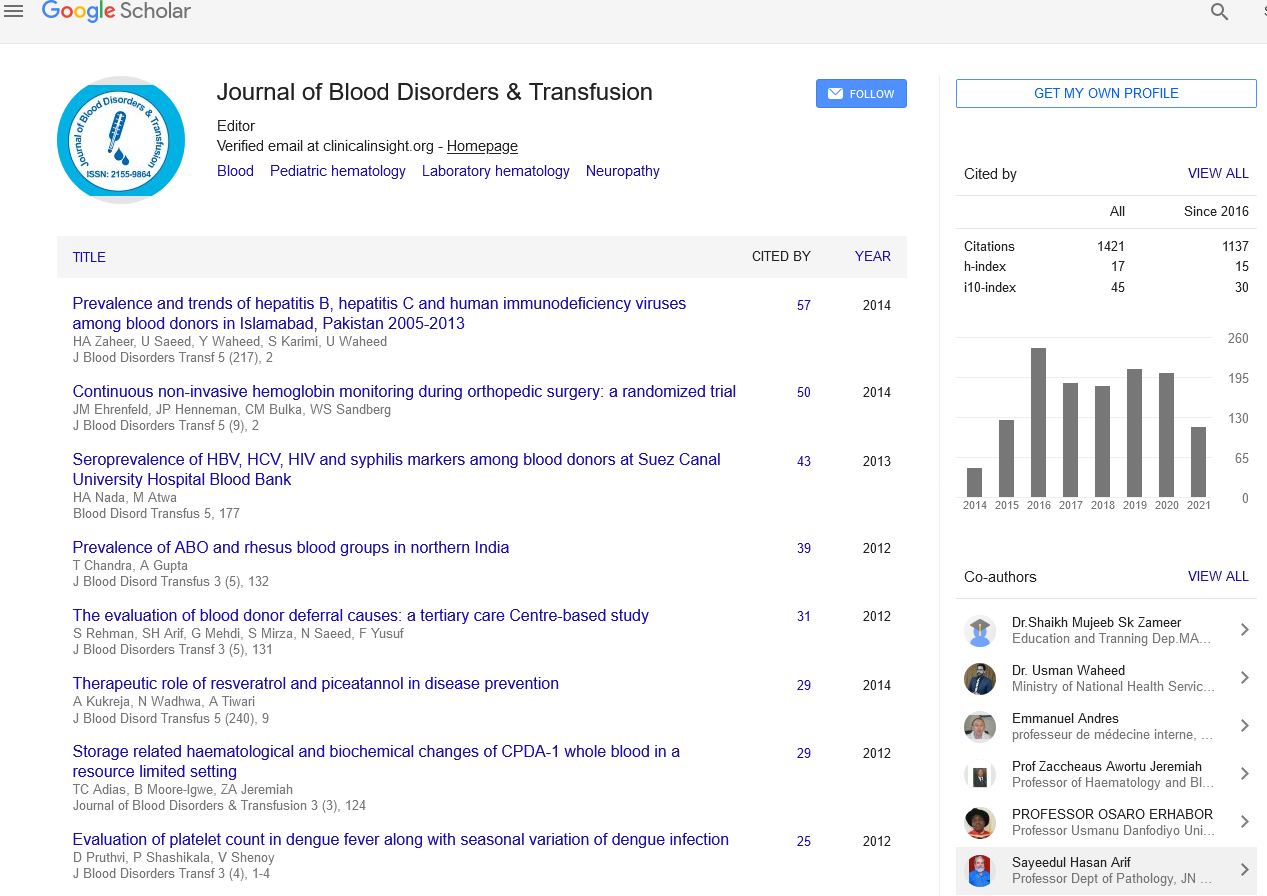
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Seroprevalence of Hepatitis B, Hepatits C, Human Immunodeficiency Virus and Syphilis in Donated Blood in Kenya, 2016: Situation Analysis
Mahuro GM, Gichangi PB, Mwangi CW and Kipkorir N
Background and Objective: Blood transfusion is a prevalent life-saving intervention that replaces blood or blood-products lost in severe malnutrition, infections, during surgical procedures, obstetrical emergencies and blood disorders or trauma. Transfusion of infected blood remains a public health concern. With all interventions aimed at reducing transfusion transmissible infections (TTIs), it’s imperative to review the Kenyan current situation. This presents TTIs prevalence among volunteer blood donors in Kenya 2016, and, relationship between volunteer blood donors’ health and risk characteristics and TTIs in donated blood. Materials and Methods: This adopts cross-sectional design for data collected for ten months in 2016. Only 17.8% of 20,230 volunteer blood donors recruited through mobile phone application, text for life (T4L), whose blood test results were uploaded into T4L and had complete data on TTI tests was included. Kenya National Blood Transfusion Services pre-screening assessment used prior to voluntary blood donation provided variables of interest for analysis. Descriptive frequencies, association test and odds ratio was performed using Stata V14.2. Result: Four in every five voluntary blood donors were male, and, had no or primary education. Hepatitis B, Hepatitis C, Human immunodeficiency viruses and Syphilis prevalence was 0.7%, 1.2%, 6.2% and 1.0% respectively. Having “disease" or “sexual” does not infer having any TTI but “stab” increases odds of having syphilis two fold (AOR=2.03, 95%CI=0.27-15.15, p=0.000). Conclusion: Excluding individuals who self-report as having had stab wounds could reduce the chances of having TTIs. Individuals found to be having TTIs should receive appropriate referrals for care and support.