Indexed In
- RefSeek
- Hamdard University
- EBSCO A-Z
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
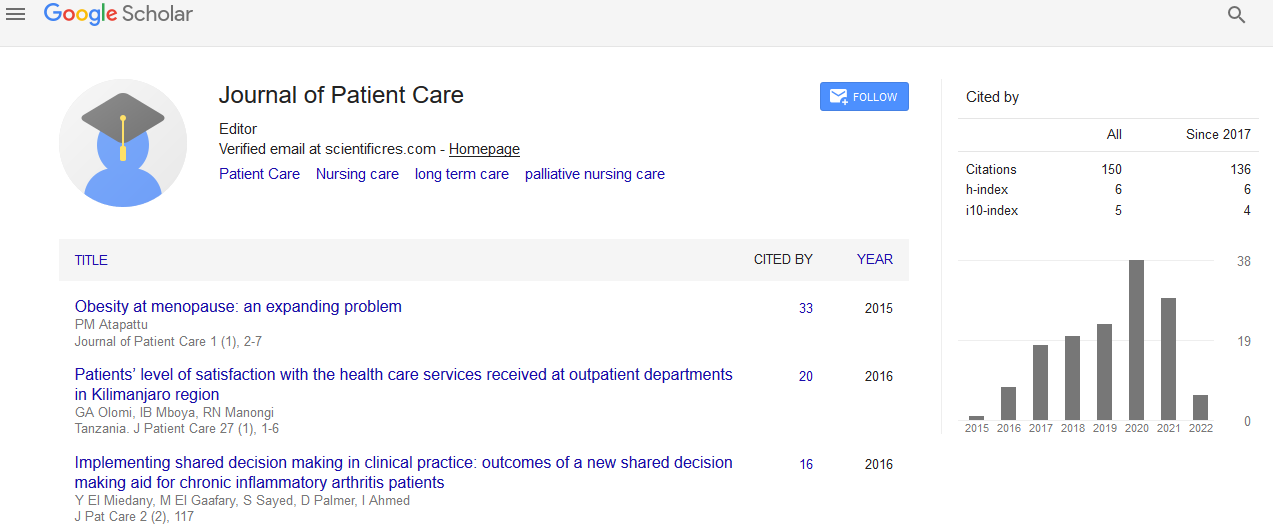
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
To Inoculate or Not To Inoculate: The Factors that Influence the Decision on Flu Inoculation
Yoram BT, Maksymiuk RA and Katarzyna Stasiuk
Objective: Patients’ poor adherence to medical advice is a major obstacle to the effective delivery of health care. The present research focuses on how patient preferences and physician preconceptions may affect a patient’s decision to comply with a physician’s recommendation regarding flu inoculation.
Methods: A 2 (physician’s recommendation: inoculate/not inoculate) by 3 (participant’s a priori attitude: pro/ neutral/against) by 2 (physician’s gender: male/female) by 2 (treatment setting: private/public) between-within-subjects design was used. One hundred eight-seven participants were asked to read four scenarios presented in random order, describing the circumstances that occur when visiting a physician who provides information about the possibility of flu inoculation. The participants’ a priori attitude toward this inoculation was then assessed. The key outcomes were the decision concerning flu inoculation and the certainty of that decision.
Results: In general, the decision on inoculation was negative. The participants who a priori objected to inoculation made a more negative choice than those who had neutral preferences and those who a priori approved of it. Compared with a negative recommendation, a positive recommendation by a physician was associated with a less negative decision. The participants were more certain when deciding against inoculation than in favor of it.
Conclusion: A positive physician’s recommendation caused the participants’ decision on inoculation to become less negative, but this suggestion was not sufficient to change the decision altogether. The participants’ a priori preference appeared to be a much more compelling factor in deciding whether to inoculate, and it also affected the conviction of that decision.