PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Access to Global Online Research in Agriculture (AGORA)
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
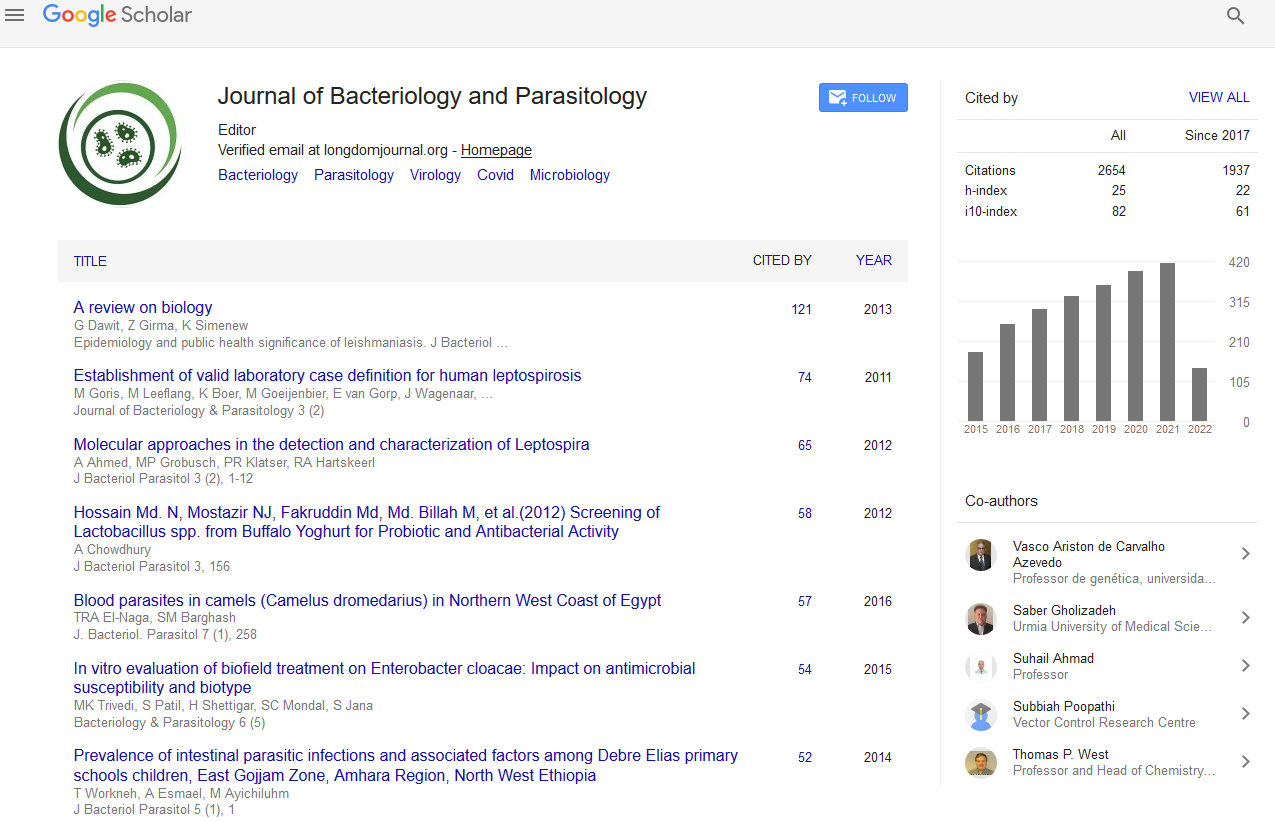
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Antibiotic resistance patterns of coagulase-negative Staphylococcus strains isolated from hospitalized patients in Cluj-Napoca, Romania
6th International Congress on Bacteriology & Infectious Diseases
May 21-22, 2018 | New York, USA
Lia Monica Junie
University of Medicine and Pharmacy, Romania
Keynote: J Bacteriol Parasitol
Abstract:
Background: Methicillin resistant S. aureus (MRSA) is responsible for hospital (HA-MRSA) and community-acquired infections (CA-MRSA). MRSA strains were identified after the introduction of methicillin in therapy. The purpose was to evaluate the antibiotic resistance phenotypes of CoNS strains isolated from hospitalized patients. Materials and methods: The study included strains isolated from hospitalized patients in Cluj-Napoca. The identification and the antibiotic resistance profiles of the strains were performed by standard and automated methods (ApiStaph galery and Vitek2Compact). Results: Of all isolates, 37.5% were CoNS: S. epidermidis (20.8%), S. intermedius (4.2%), S. capitis (2.1%), S. hominis (2.1%), S. haemoliticus (4.2%), S. saprophyticus (2.1%) and other CNS (2.1%). From all the CNS strains, 26 strains (27.18%) showed Meticiline resistance (MR). The CNS strains showed high rates resistance to Penicillin (25%), to Erythromycin (22.9%), to Imipenem (16.7%), to Rifampycin (10.41%) and to Fosfomycin (29.16%). The CNS strains resistant to Meticiline were: S. Epidermidis (20.8%), S. Intermedius (4,2%), S. Haemoliticus (4.2%), S. saprophyticus (2.1%) and other SCN (21%). The MR CNS strains were resistant to Eritromycin (14.6%), Clindamycin (14.6%), Ciprofloxacin (16.7%), Gentamycin (16.7%), Rifampycin (14.6%), Tetracyclin (25%) and Imipenem (22.9%). The resistance to Moxifloxacin was 10.41%. All strains were susceptible to Teicoplanin and Vancomycin. Conclusion: Following the strains antibiotics resistance profile, we conclude to the circulation in our geographic area of strains with different resistance phenotypes. This finding indicates the necessity to detect them by PCR, for limiting the spread of these strains in hospitals and community.
Biography :
Professor, MD, PhD, Lia Monica Junie, from the Microbiology Department of “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania. She is head of the department, coordinating also, the activities of both laboratory medicine specialty resident doctors and PhD doctor’s thesis in the medicine field. She unfolds a fruitful national and international scientific activity as an experienced microbiologist, having an impressive CV. She is member in the Board of Scientific Societies, reviewer in many peer-reviewed journals, expert of the Ministry of Education and Research and Evaluator. She coordinated research projects, published books and more than 200 scientific articles in prestigious Journals. She organized and attended numerous national, international congresses, as president, member in the Organizing Committees, Invited speaker, Keynote speaker or Chairperson. She unfolds a high level activity after years of experience in research, evaluation, teaching and administration both in hospital and education institutions.
Email:monicajunie@yahoo.com