PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
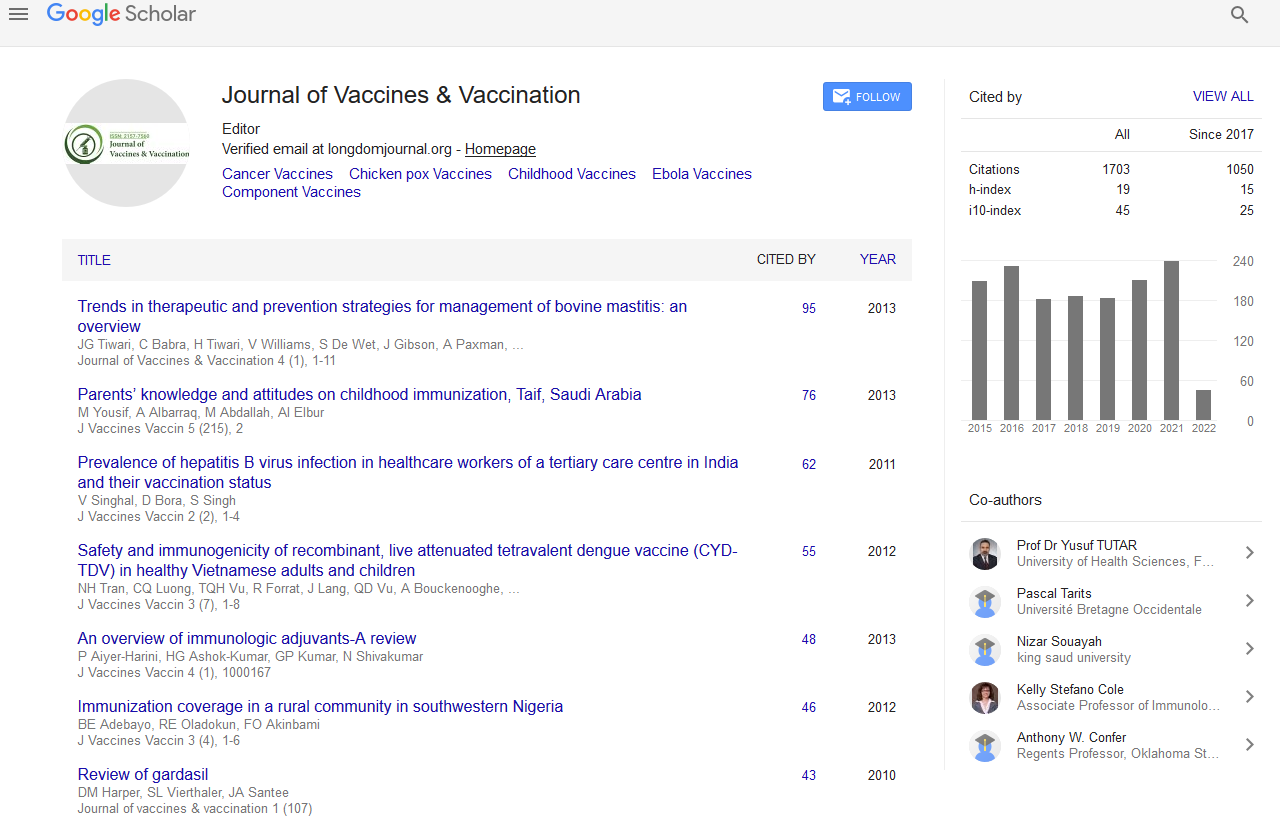
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Carbohydrate based vaccines for the treatment of cancer
International Conference & Exhibition on Vaccines & Vaccination
22-24 Nov 2011 Philadelphia Airport Marriott, USA
Livingston P.O and Ragupathi G
Scientific Tracks Abstracts: J Vaccines Vaccin
Abstract:
As vaccines against cancers (and infectious diseases) have employed increasingly focused and homogeneous antigens for vaccine construction, the immunogenicity of these antigens has been observed to markedly decrease. Th is can be off set by conjugating these homogeneous antigens to an immunogenic carrier protein such as keyhole limpet hemocyanin (KLH) or the use of a potent immunological adjuvant such as the saponin QS-21. Especially in the case of vaccines against cancer antigens (generally autoantigens), both carrier protein conjugation and immunological adjuvant have been required. Many of the antigens over-expressed on the cancer cell surface are carbohydrate antigens expressed on cells of particular lineages. Th ese have been surprisingly potent targets for immune recognition and attack by antibodies, both because of their abundance at the cell surface and their unexpected immunogenicity in KLH- conjugate+QS-21 vaccines. Passively administered and vaccine induced antibodies targeting carbohydrate antigens have eliminated circu lating tumor cells and systemic micrometastases in a variety of preclinical models. A series of these cancer cell-surface diff erentiation antigens have now been identifi ed, synthesized, KLH conjugated, and demonstrated to induce antibodies in the majority of vaccinated cancer patients. Th ese include GM2, GD2, GD3, Fucosyl GM1 and sialyl Lewis A (sLea) gangliosides, globo H glycolipid, Tn, sTn and TF blood group related antigens, polysialic acid, and MUC1 peptide. For maximal impact, largely due to tumor cell heterogeneity, polyvalent vaccines will be required. A series of double blind, randomized trials with diff erent polyvalent vaccines designed to test clinical impact against particular cancer types in the adjuvant setting are currently in progress. Th e trivalent ganglioside vaccine against sarcomas is a good example. It is based on the immunogenicity of each of its 3 conjugates:
Biography :
Philip Livingston received his MD degree from and is currently Professor of Medicine in the Joan and Sanford Weill Medical College at Cornell University and Attending Physician and Member in Memorial Sloan-Kettering Cancer Center where he has treated patients and run a research lab for 36 years. His research has focused on: identi fi cation of suitable targets for immunotherapy of a variety of cancers, construction of polyvalent conjugate vaccines speci fi cally designed to augment antibody responses against these targets, and identi fi cation of optimal immunological adjuvants to further augment the potency of these vaccines. He has over 150 publications and 4 issued and 3 pending patents concerning cancer vaccines. Recently, he helped establish MabVax Therapeutics, Inc., a small biotech company. MabVax supports several randomized Phase II trials with these polyvalent vaccines and establishment of human monoclonal antibodies against cancer antigens from the immunized patients