PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
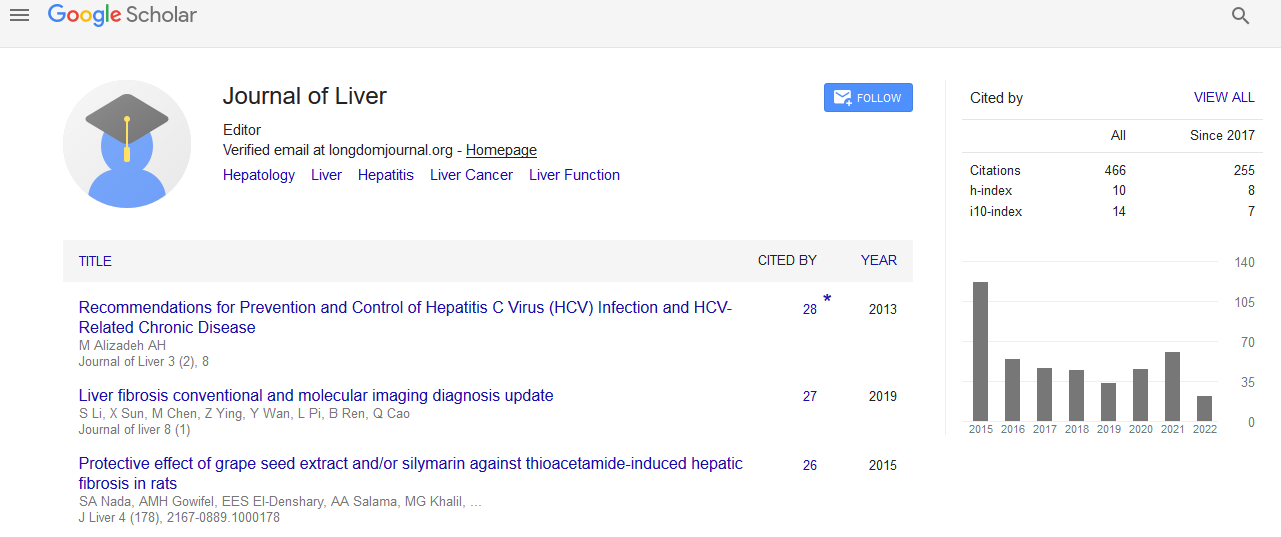
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Gene up and down-regulation with moderate magnetic fields via toll-receptors and WNT5a: Fatty liver/NASH cirrhosis and HCC in âMice and Menâ
World Congress on Hepatitis
July 20-22, 2015 Orlando, Florida, USA
Trent W Nichols1 and Kevin Yarema2
Scientific Tracks Abstracts: J Liver
Abstract:
Background: At DDW 2014, S Mittal showed that over 1500 Veterans in 2013 were diagnosed with HCC and that this trend is increasing every year. The greater percentage of patients with NAFLD-related HCC did not undergo HCC surveillance. Additionally, a previous report by L Bi has shown that WNT5a has been shown to be involved in cancer progression and was down-regulated in hepatocellular cancer. We have previously reported that many genes in obesity and fatty liver (NAFLD) are associated with insulin resistance and their association to Non-Alcoholic Steatohepatitis (NASH) and the progression to cirrhosis. We now report that many of these genes seen in NASH are regulated by static magnetic fields and that WNT5a is up-regulated. Methodology: Gene array analysis of 2 human embryonic stem cells lines in another experiment of 0.23-0.28 T Static Magnetic Fields (SMF) at JHU, as previously described, was conducted to exam the mechanism of DC EMF via the impact of altered Ca2+ flux and lipid membrane domain fluidity on signaling pathways via TRL4 and IL6. Some 2500 genes were found to be up and down-regulated. Recently, further inspection was conducted on Cell Cycle, Cancer, Cell to Cell Signaling, and Cellular Development. Results: Analysis of ingenuity pathways of the Affymetrix gene arrays revealed WNT5a up-regulation by SMF after down-regulation of IL6 mRNA at 5 days in stem cell lines. Down-regulation of tumor necrosis factor alpha and up-regulation of TLR 4 were demonstrated for this transformation. Chemokine genes CCL2, CXCl1, CXCL2, MMP9, SERPINE1, IL6, and IL1B (genes for fibrosis) were downregulated. TIMP1 and SOCS3 metalloproteinase inhibitors were up-regulated. Forkhead FOXO1 and 3 transcription factors were also up-regulated at 5 days. FOXM1 expression when silenced has been found to suppress human HCC cell growth in vitro by Park. Of the 47 genes up-regulated in NASH in obesity and NASH, 11 were identified as down-regulated by SMF and 2 up-regulated which can prevent fibrosis. Discussion: WNT5a up-regulation by SMF leads to NLK down regulation. Nemo Like Kinase -SETDB1 complex subsequently interacts with PPARG. Methylation of PPARG target promotes histone H3KP and transcriptional silencing inhibiting adipogenesis. Conclusions: Polygene up-regulation and down-regulation occurs in fatty liver/NASH. Moderate magnetic field therapy was found in 1 week of therapy of an animal model to reduce fat in Ob/Ob mice by this author and in human stem cells lines suggesting that such therapy may be helpful in therapy for NASH to prevent HCC. Adding electrons to the mitochondria electron transport chain is one of the suggested mechanisms. Accelerated liver detoxification by moderate magnetic therapy of obesogens in human subjects that disrupt homeostasis of metabolism of lipids ultimately resulting in obesity is also possible. Activation of AMPK inhibits cancer cell growth through AKT/FOXO3a/FOXM1 signaling cascade. Polygenic up and down-regulation in NASH and its progression to HCC via DC EMF is, therefore, a possible solution to this epidemic problem. High dose Vitamin D3 in a weekly oral dose of 50,000 U was used at VHA Martinsburg in 221 patients with HCV while undergoing Sof/Sim oral therapy and later Harvoni or Viekara to prevent HCC. A previous epidemiology study demonstrated that the risk of HCC was reduced by 49% in those Europeans with the highest levels of 25(OH) D. NASH/NAFLD patients and HBV patients on Entecovir were also given Cholecalciferol.
Biography :
Trent W. Nichols Jr. MD, is an internist, nutritionist, and gastroenterologist with more than 30 years of clinical experience. He is the founder and director of the CNDD and the Advanced Magnetic Research Institute in Hanover, Pennsylvania. He is a graduate of the University of Denver with a BS in Chemistry and Northwestern University with a MD. His postgraduate education medicine was at Northwestern University in Internal Medicine and Fellowship in Gastroenterology and Hepatology. He has been the lead investigator in over 50 pharmaceutical trials and has worked for the Veterans Administration, Kaiser Permanente, Good Samaritan Hospital in Lebanon PA, and Sinai Hospital In Baltimore MD. He is a member of the American Gastroenterology Association, Society for Neuroscience, and Bioelectromagnetic Society. He is on the editorial panel of the Journal of Liver OMICS and has been active researcher in the role of mitochondrial dysfunction in liver disease and therapy with EMF.