PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Scimago
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
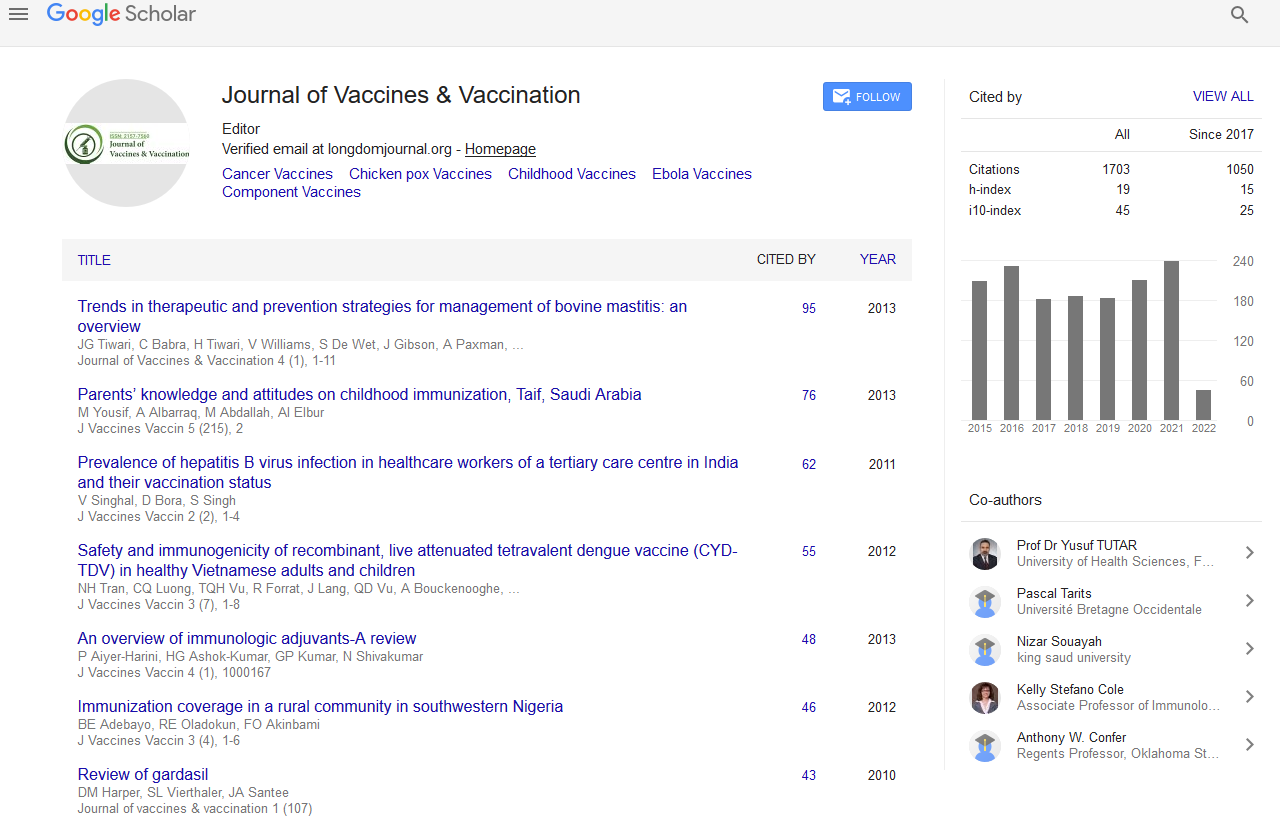
- Google Scholar
Useful Links
Share This Page
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Immunological pattern of hepatitis B infection among exposed and non-exposed babies in a PMTCT program in low resource setting: Does every exposed newborn require 200 IU of hepatitis B immunoglobulin?
3rd International Conference on Vaccines & Vaccination
July 29-31, 2013 Embassy Suites Las Vegas, NV, USA
Joseph Onakewhor, Charurat M, Matthew O, Esosa Osagie, Asemota and Sadoh W. E
Scientific Tracks Abstracts: J Vaccines Vaccin
Abstract:
G lobally, about 2 billion people have markers of current or past hepatitis (HBV) infection and estimated 350-400 million are chronically afflicted. In Nigeria, 4.3% and 6.8% of pregnant women and partners of infected women respectively are infected. Though, a vertically transmissible and vaccine preventable infection, data on mother-to-child transmission (MTCT) of HBV in Nigeria is scarce. Immunoprophylaxis with immunoglobulin (HBIG) for exposed babies plus a course of 3 vaccinations is expected to produce adequate immune response (antibodies>100 mIU/ml) and protection for at least 25 years. We investigated the immunological pattern of HBV-infected mothers and their exposed infants and compared them with HBV-non-exposed babies in a prospective case-control pilot study in a PMTCT program in low-resource setting (LRS). The Nigerian Government/ UNICEF provides free to children HBV immunization but HBIG is provided at personal cost that is prohibitive to majority of parents. When exposed infants did not receive HBIG, parents exhibit a lot of anxiety about the potential for their infection. Consequently, we determined if every exposed newborn required standard dose 200iu HBIG in LRS. We compared the pattern of immunological response of infants that received 200iu with those that received 100iu HBIG. All babies received in addition three doses of HBV vaccine. The median period of followed-up was 9 (range 0-15) months. The MTCT rate was zero. However, exposed babies were less likely than their unexposed counterparts to respond to vaccination (p<0.0001; RR 0.055). We advocate large multicenter studies as our findings may elicit policy change beneficial to people from LRS.
Biography :
Joseph Onakewhor obtained his M.D. and M.P.H. from the University of Benin, Nigeria and M.Sc. in Human Anatomy for the University of Calabar, Nigeria. He had his residency training at the University of Benin Teaching Hospital (UBTH), and bagged the fellowship of the West African College of Surgeons (FWACS) in the Faculty of Obstetrics and Gynecology. He was awarded the fellowship of the International College of Surgeons (FICS) 2004. He also had training at the Institute of Human Virology, University of Maryland, Baltimore and an ISID-sponsored fellowship at the Memorial Sloan Kettering Cancer Center, New York. He is a Professor and Consultant OB-Gyn in Maternal-Fetal Medicine at UBTH with over thirty five publications in reputable journals, member of the National Task Team PMTCT of HIV in Nigerian, Focal Point PMTCT, UBTH and member of two editorial boards.