PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- JournalTOCs
- ResearchBible
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Scholarsteer
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- Geneva Foundation for Medical Education and Research
- Euro Pub
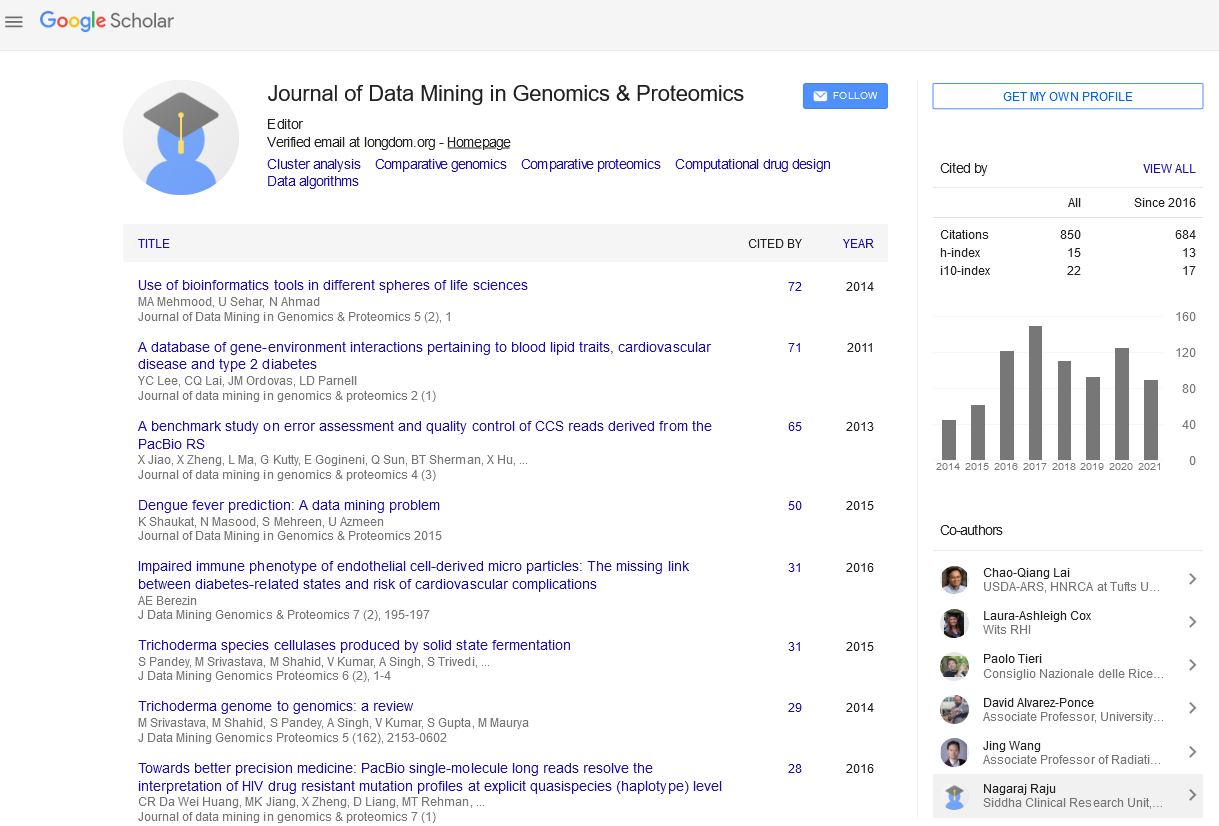
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Implementation of pharmacogenetics approaches at the NIH hospital
2nd International Conference on Big Data Analysis and Data Mining
November 30-December 01, 2015 San Antonio, USA
Tristan Sissung, Barry R. Goldspiel, Willy A. Flegel, Gary DiPatrizio, Sharon D. Adams, Scott Penzak1, Les Biesecker3, Thomas Fleisher, Jharana J. Patel, David Herion, William D. Figg, Juan Lertora1 and Jon W. McKeeby
National Institutes of Health Clinical Center, USA National
Cancer Institute, USA
National Human Genome Research Institute, USA
Posters-Accepted Abstracts: J Data Mining Genomics Proteomics
Abstract:
Pharmacogenetics-informed treatment has the potential to greatly reduce adverse drug reactions and increase the efficacy of therapeutics often used in hospital settings. We formed a multi-departmental Pharmacogenetics Testing Implementation Committee (PGTIC), overseen by the Pharmacy and Therapeutics Committee (PTC), to select important variants and to develop infrastructure for clinical decision support (CDS). The development, progress, challenges, and future perspective will be discussed. During the development stages, the committee considered only clinically actionable gene-drug interactions with sufficient levels of evidence. The PGTIC then made specific recommendations regarding alternative therapeutic strategies that were approved by the PTC. Implementation has, thus far, included avoidance of severe immune adverse drug reactions by genotyping HLA loci in patients treated with certain agents (i.e., abacavir, allopurinol, and carbamazapine) using existing infrastructure for genetic analysis. The electronic health record (EHR) was updated to flag important potential pharmacogenetic test results to prescribing physicians (i.e., result present, result absent, result pending, or test not ordered). The prescribing physician is then either prevented from administering the drug, or is allowed to over-ride the system by providing a reason. Suitable technology for acquiring genotypes is currently being ascertained; it appears that array-based platforms will be used for this purpose, although we will filter the results to include only relevant genetic variants. The EHR will be updated with these variants as the PGTIC decides on specific recommendations regarding therapeutic choice and/or dosing changes of certain drugs. The future of clinical implementation of pharmacogenetics data at the NIH Clinical Center depends on vigilance of curating important variants and networking with other organizations (i.e., FDA and the Pharmacogenetics Research Network).
Biography :
Tristan Sissang received his B.S. in biochemistry and his M.S. in organic chemistry from the University of California at Riverside. He earned a Ph.D. in genetics from The George Washington University. He is a staff scientist in the Clinical Pharmacology Program, within the Clinical Center, at NCI. His research focus is molecular genetics and translational pharmacogenetics. He has published over 40 peer-reviewed papers, and holds 4 patents relating to pharmacogenetics testing.