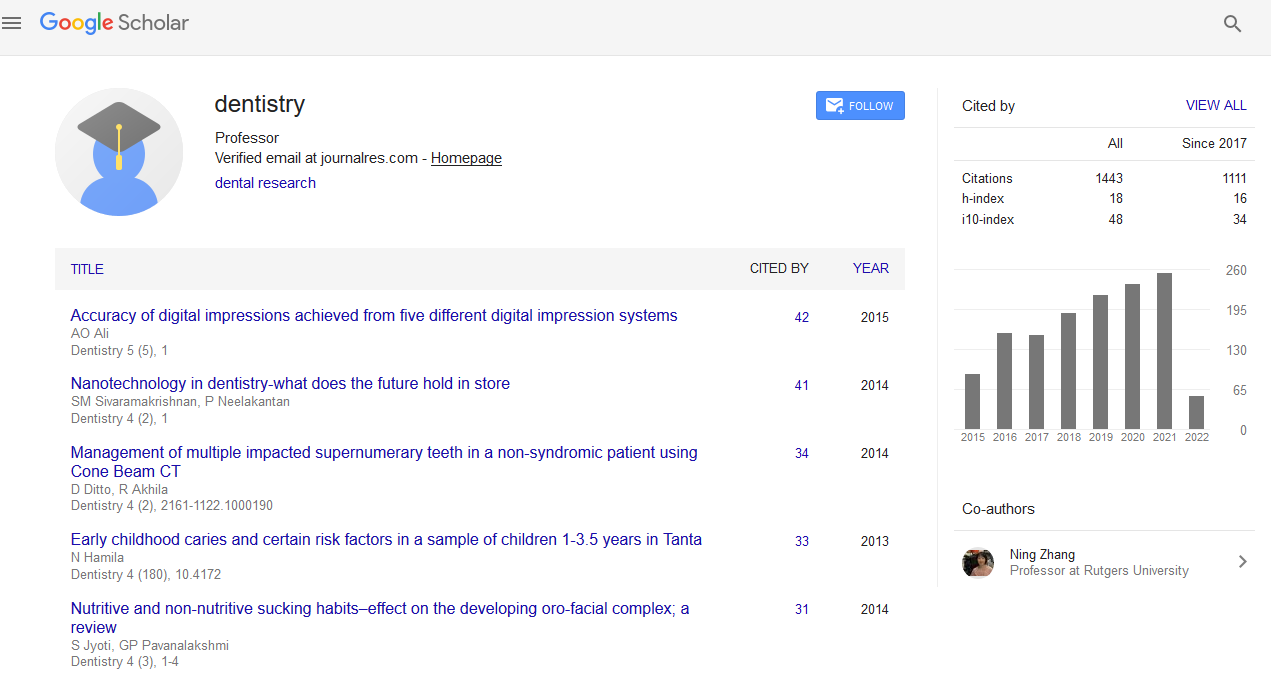
Citations : 1817
Dentistry received 1817 citations as per Google Scholar report
Indexed In
- Genamics JournalSeek
- JournalTOCs
- CiteFactor
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Periodontal wound healing/regeneration: Biologic directives for clinical
International Conference on Dental & Oral Health
August 19-21, 2013 Embassy Suites Las Vegas, NV, USA
Ulf ME Wikesj?
Accepted Abstracts: Dentistry
Abstract:
Current clinical protocol aimed at regeneration of the periodontal attachment generally meets limited success. The procedures are either unpredictable or, with few exceptions, result in only incremental improvements. Limited treatment outcomes may result from incomplete understanding of biologic processes critical to periodontal wound healing. Our laboratory has developed discriminating preclinical models to evaluate the biology of periodontal wound healing/regeneration under optimized conditions, and to evaluate the efficacy and safety of candidate biomaterials, devices, and biologic factors intended for periodontal regeneration prior to clinical introduction. We have evaluated occlusive and novel macro-porous devices (developed in our laboratories) for guided tissue regeneration (GTR), various bone derivatives and bone substitutes, and matrix, growth and differentiation factors including fibronectin, PGE 1 , rhTGF-? 1 , rhBMP-2, rhBMP-12/rhGDF-7, and rhGDF-5/rhCDMP-1 in advanced periodontal defects. This presentation will discuss biologic requirements for successful periodontal regenerative procedures unrelated to adjunctive devices, biomaterials, and biologics. This presentation will also discuss background and biologic potential of current treatment concepts including root conditioning, GTR, bone biomaterials, and candidate therapies including growth and differentiation factors as standalone protocols or in combinations. Our studies suggest that wound stability during the early healing phase will allow maturation of the tooth gingival flap interface into a new connective tissue attachment rather than formation of an epithelial attachment (long junctional epithelium). Root conditioning and/or surgical implantation of biologic agents, bone biomaterials, and devices for GTR may dramatically alter the outcomes of healing for better or worse.
Biography :
Ulf ME Wikesj? received his DDS from the Faculty of Odontology, Lund University, Malm?, Sweden, and DMD from Temple University, Philadelphia, PA, USA; certification for advanced training in periodontology at Lund University, Sweden conferred by the National Board of Health and Welfare, Sweden, and from Loma Linda University, Loma Linda, CA, USA; and a Ph.D. (Odont Dr) on Experimental Wound Healing from Lund University, Sweden. He is an Adjunct Professor of Periodontology, Malm? University, Centre for Oral Health Sciences, Malm?, Sweden, and a Diplomate of the American Board of Periodontology. He serves on the editorial board of scientific journals in periodontology, implant dentistry and tissue engineering.