PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
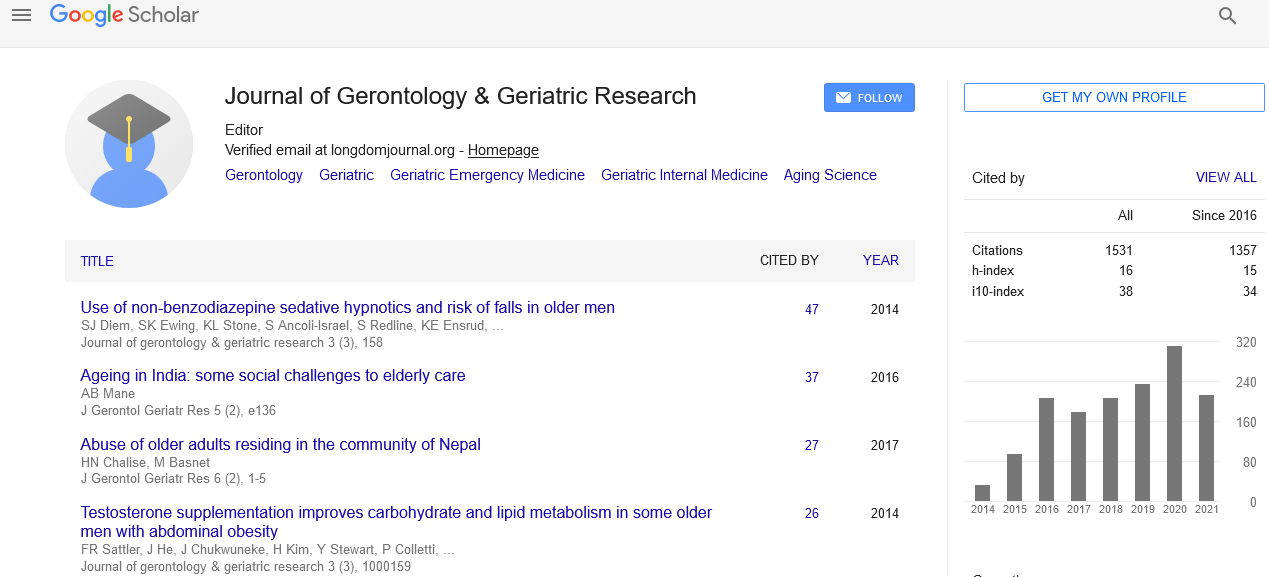
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
The partnership between primary and palliative care: A collaboration that can facilitate interdisciplinary care to improve patient outcomes
2nd International Conference on Geriatrics & Gerontology
August 24-26, 2015 Toronto, Canada
Wendy Stoelting-Gettelfinger
University of Indianapolis, USA
Scientific Tracks Abstracts: J Gerontol Geriat Res
Abstract:
An effective partnership between primary care and palliative care is crucial to improving the quality of life for many patients and their families. Innovative solutions must be developed to address the current shortage of palliative care specialists. One viable solution is the partnership between palliative and primary care referred to as �??primary palliative care�?�. Primary care providers including advance practice nurse providers (primary care providers) are in a unique position to manage symptoms, assist families with treatment plan decisions and make early referrals to coordinate interdisciplinary care with the ultimate goal of reducing patient suffering and improving quality of life. Primary care providers often have long-term relationships with their patients and an insightful understanding of family dynamics. Primary care providers are in a trusted position to assist families with difficult care decisions without infringing upon their autonomous rights. Unfortunately, primary care providers depending upon their background and expertise may or may not be knowledgeable in the difference between palliative care and end-oflife services. Understanding these key differences as well as the differences between primary, secondary and tertiary palliative care is fundamental for primary providers to provide appropriate care. Educating primary care providers regarding the key role that they can play in coordinating interdisciplinary palliative primary care is the first step to providing comprehensive, un-fragmented care for patients needing palliative care services. Understanding that palliative care can improve outcomes, save health care dollars while improving quality of life is essential to successful interdisciplinary partnerships and coordination of palliative care services.
Biography :
Wendy Stoelting-Gettelfinger completed her JD in 1993 with joint PhD in nursing in 1999 from Indiana University. She is the Coordinator for the Family Nurse Practitioner program at the University of Indianapolis and works as a Family Nurse Practitioner (FNP) in a comprehensive primary care practice. While she coordinates palliative and end-of-life services for her primary care patients, she recently experienced these issues on a personal level through the loss of her parents and developed an increased appreciation for the difference that palliative care can make to enhance quality of life for patients and their families.
Email: stoeltinggett@uindy.edu