PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
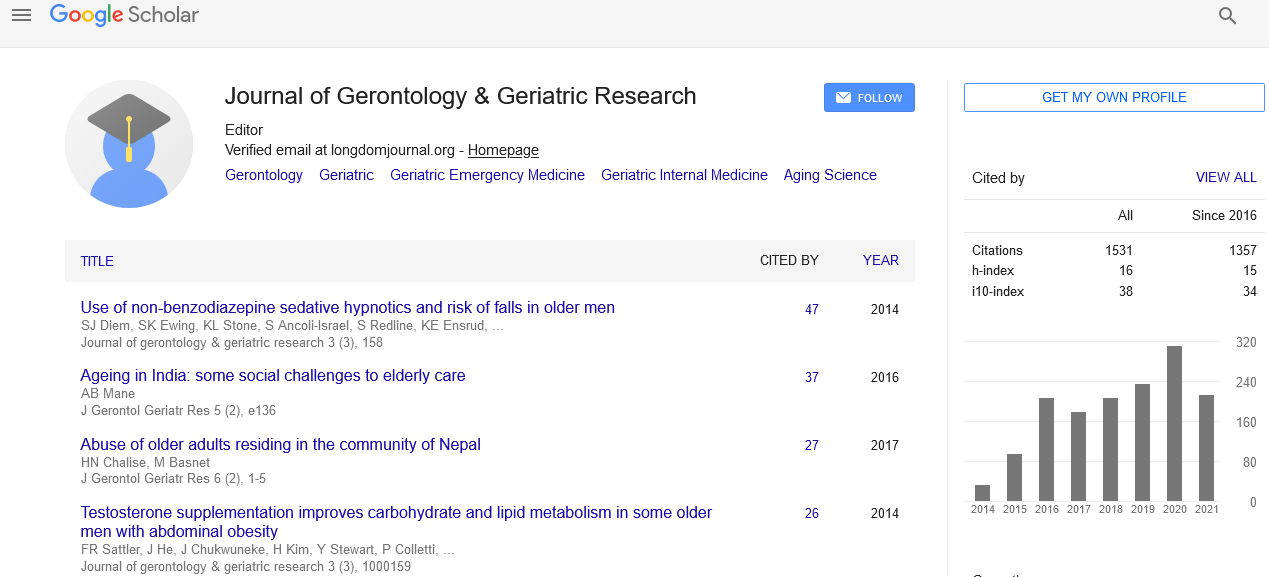
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A New Behavioural Assessment Tool for Patients with Major Neurocognitve Disorders: Results of a Clinical Study
120 residents with dementia in long term care facilities were recruited for the study. Pittsburg Agitation Scale was used to screen for the presence of BPSD. 60 patients were in the control group and 60 patients in the study group. Construct and criteria validity was established by comparing LuBAIR to BEHAVE-AD and Cohen-Mansfield Agitation Inventory. Intra- and inter-rater reliability of LuBAIR was also established. A Clinical Utility Survey (CUS) survey was developed for the study to determine the usefulness of LuBAIR on three variables: less labor intensive, more comprehensive and better categorization of behaviors in clinical meaningful categories. Intra-rater reliability was established for 8 of 12 and inter-rater reliability for 10 of 12 behavioral categories. LuBAIR had comparable Construct and Criteria Validity. CUS findings showed 23% of nurses found LuBAIR less labor intensive, 77% found it more comprehensive and 98% agreed LuBAIR helps understand behaviors in clinically meaningful ways.