Awards Nomination
20+ Million Readerbase

Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
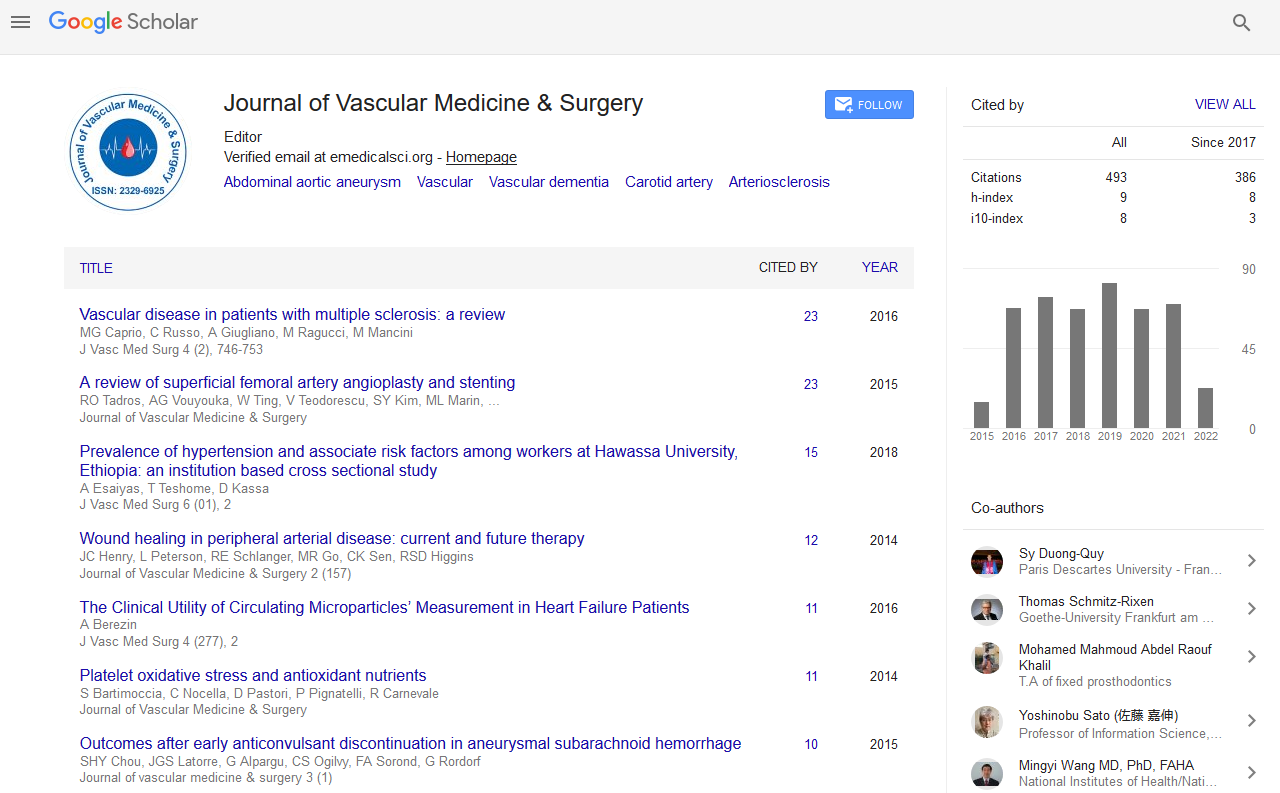
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
A Case of Disseminated Intravascular Coagulation Caused by a Ruptured Abdominal Aortic Aneurysm for which Recombinant Human Soluble Thrombomodulin was Effective
Recombinant human soluble thrombomodulin (rhTM) is a new anticoagulant agent that exerts anticoagulatory and anti-inflammatory effects and is effective in the treatment of disseminated intravascular coagulation (DIC). We herein report the case of a 67-year-old male with DIC that developed following the surgical repair of a ruptured abdominal aortic aneurysm (AAA). After the initial operation, DIC occurred and became prolonged. rhTM was then administered, and the DIC state was relieved. In this case, rhTM might be effective for the treatment of DIC after the repair of ruptured AAA.