PMC/PubMed Indexed Articles
Indexed In
- Academic Journals Database
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- CiteFactor
- Scimago
- Ulrich's Periodicals Directory
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
- Publons
- MIAR
- University Grants Commission
- Geneva Foundation for Medical Education and Research
- Euro Pub
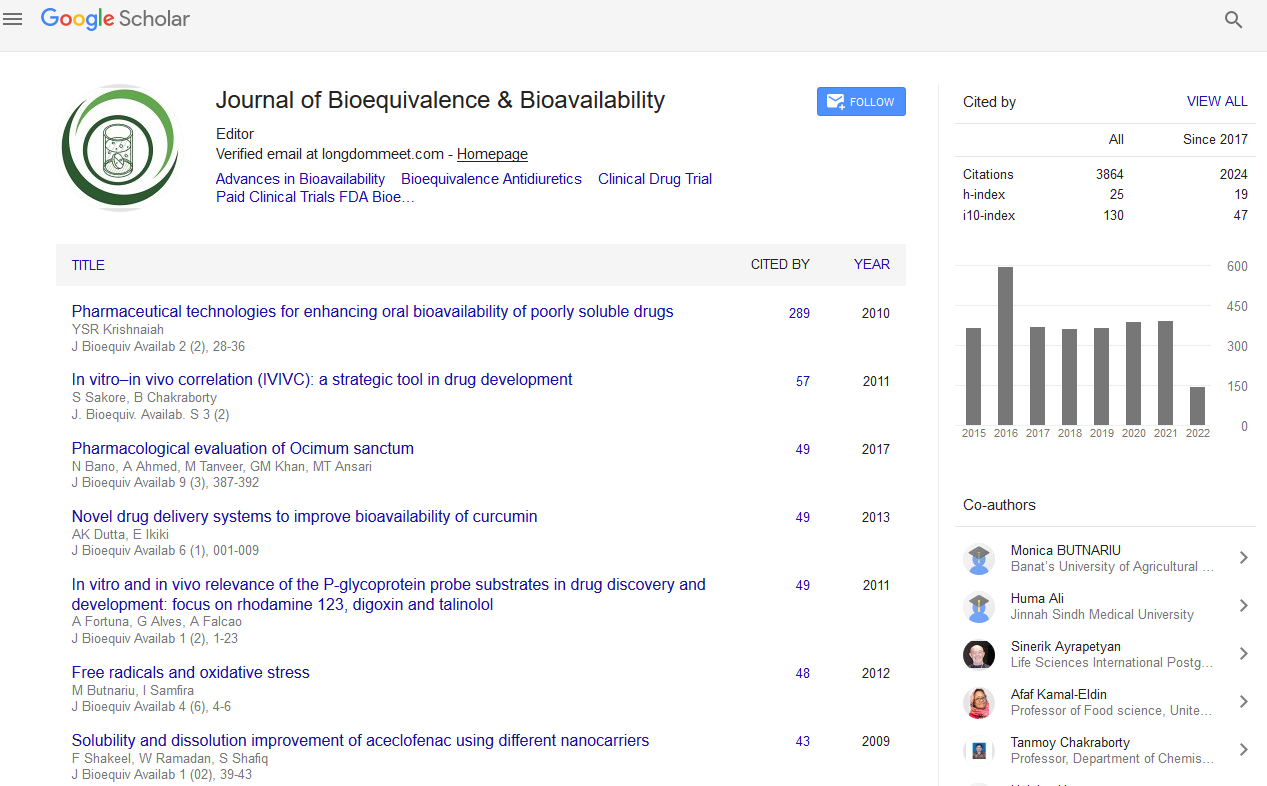
- Google Scholar
Useful Links
Share This Page
Journal Flyer
Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Use of Recombinant Factor VIIA as a Risk Factor for Graft Loss after Orthotopic Liver Transplantation Due to Hepatic Artery Thrombosis
Fabian A Helfritz, Penelope Stiefel, Michael P Manns, Jürgen Klempnauer, Frank Lehner, Henrike Lenzen and Sandra Ciesek
Background: The genetically engineered recombinant activated factor VII (rFVIIa) was primarily developed for the treatment of bleeding episodes in haemophilia patients with inhibitors. Different outcomes have been described in a number of studies evaluating the off-label use in patients with liver disease and consequently with complex coagulopathies. We here evaluated the use of rFVIIa in patients undergoing orthotopic liver transplantation (OLT). The aim of this study was to determine the safety within this patient population.
Methods: Overall, 1343 OLTs were performed at Hannover Medical School between 2002 and 2014. Out of this group we selected patients having received rFVIIa in the early phase after OLT. We retrospectively analyzed the outcome of patients treated with rFVIIa and compared our findings to those from other transplant centers.
Results: In a single center retrospective analysis we identified eight patients after OLT who received treatment with rFVIIa (0.59%). Five out of eight (62.5%) patients suffered graft loss due to hepatic artery thrombosis (HAT). None of these patients had a history of thrombosis or signs of hypercoagulopathy. 60% of the patients who developed HAT had a primary graft non-function. Interestingly, rFVIIa administration was the only risk factor for HAT and consequently for graft loss in our cohort. Other known risk factors such as cold ischaemic time, number of anastomoses, donor age of > 60 years and CMV status could be excluded.
Conclusion: This study shows that rFVIIa treatment is a highly likely risk factor for the development of HAT and consequently graft loss in patients after OLT. Thus, usage of rFVIIa in this patient population should be avoided.