Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
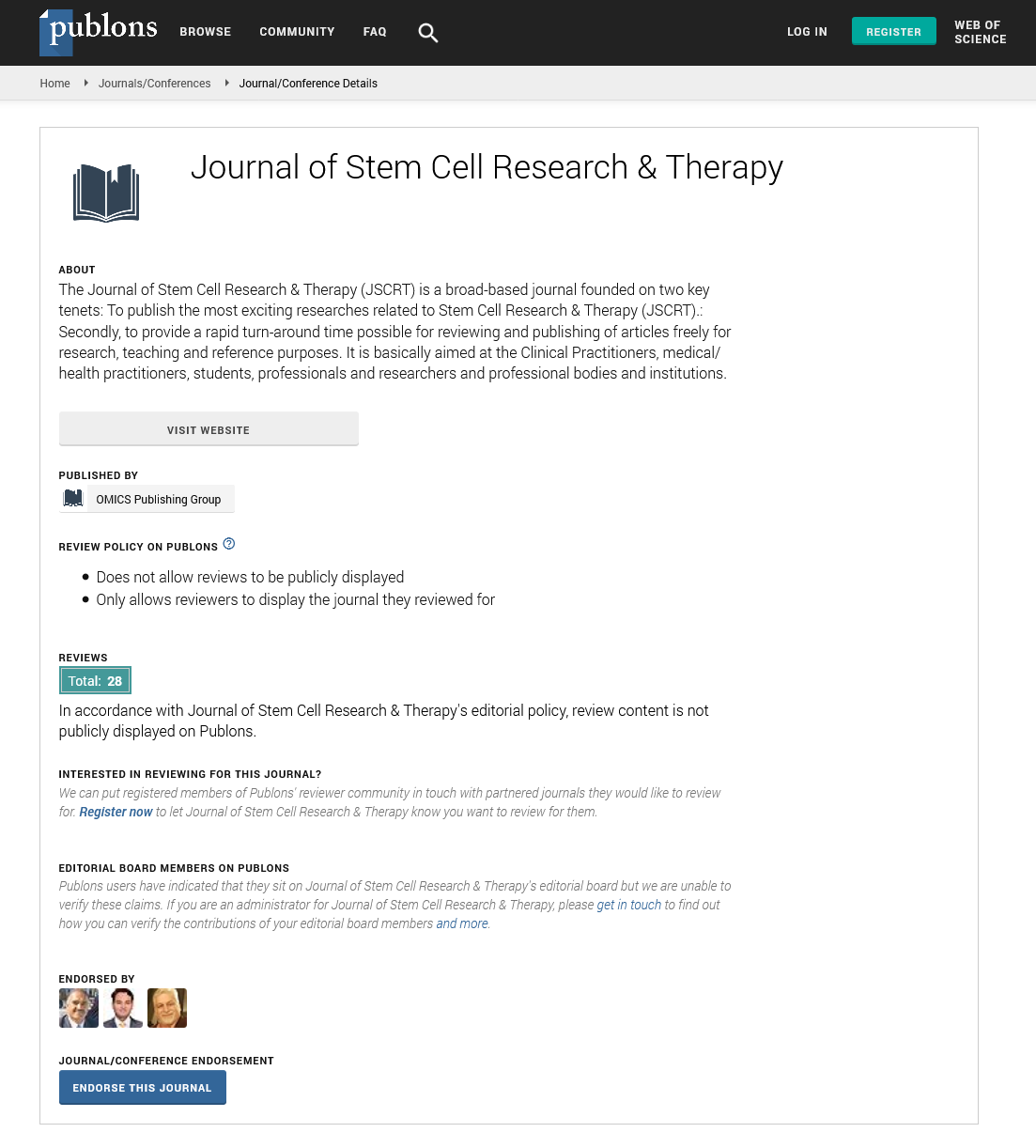
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Comparison between healthy donor-derived bone marrow mesenchymal stem cells BM-MSCS and human dermal fibroblasts: Impact on clinical applications of HMSCS
4th International Conference and Exhibition on Cell & Gene Therapy
August 10-12, 2015 London, UK
Mohammed Al Bagami, Hakim Ouled Haddou, Ingrid Marcq, Véronique Debuysscher, Christèle Ossart, Aline Regnier, Jean-Pierre Marolleau and Hicham Bouhlal
Scientific Tracks Abstracts: J Stem Cell Res Ther
Abstract:
Objective: The results of clinical applications of human Mesenchymal Stem Cells (hMSCs) depend on clinical and biological
factors. The quality of stem cell culture will affect success rate. Stem cell culture contamination by fibroblasts can be happened.
The identification of the differences between these two cell types plays an important role to improve the quality of the therapeutic
uses of hMSCs. Our present work is the first work to compare the phenotype and functional properties of primary human dermal
fibroblasts HDF to hMSC from Bone Marrow BM to reflect the impact of the possible contamination of bone morrow derived
hMSC (BM-hMSC) by fibroblasts.
Methods: In this study, hMSCs were obtained from the BM of (Healthy donor, n=5) and compared to primary HDF. The following parameters
were used for this comparison: Cell morphology, cell proliferation tests, cell cycle, immunophenotype, pluripotent and differentiation capacity
into osteoblastic and adipogenic lineages. Gene expression profile was determined in BM-MSCs and HDF by Q-PCR.
Results: Our results show that both of BM-hMSCs and HDF cells have homogenous fusiform, fibroblast-like appearance. Human
derived fibroblasts showed, significantly (p<0.001), high proliferative ability than hMSCs, which induces a shortening of doubling time
(27.3-/+3h vs. 44.5-/+ 8h for HDF and BM-MSCs, respectively; p<0.0001). The analysis of cell cycle shows that HDF cultures contained,
significantly p<0.001, two-fold higher cell number at synthesis stage (S) than in BM-hMSC cultures. Both cell types share the same
immunophenotypic feature for these surfaces markers CD45(-), HLA-DR(-), CD73(+), CD90(+), CD105(+), and CD166(+) but CD146
and CD10 were differently expressed on BM MSCs Vs. HDF. Both of cell types have a potential to differentiate into osteoblastic and
adipogenic lineages showed by specific stains. This result was confirmed by the expression levels of Runx2, PAL and Osterix (osteoblasts);
and PPAR-γ2 (adipocytes). However, expression of these genes in osteoblasts and adipocytes derived from HDF remains, significantly
p<0.05, two times lower than the expression in osteoblasts and adipocytes obtained in BM-MSCs differenced cells.
Conclusion: Our results confirm the similarities of morphology and phenotype of both HDF and BM-MSCs. The differentiation
potential of BM-MSCs cannot be used to distinguish between HDF and BM-MSCs as we showed that HDF could differentiate into
other cell types as osteoblasts and adipocytes. The genes expression profile in osteoblasts and adipocytes derived from BM-MSCs
and HDF can be used to distinguish between these two cell types as we found the genes expression in osteoblasts and adipocytes
derived from HDF were significantly lower than in BM- hMSCs. These results may explain the unexpected results of hMSCs
in therapeutic applications. In this current study, new marker was identified to discriminate HDF from BM-hMSCs in order to
improve the quality of the therapeutic uses of hMSCs.
Biography :
Mohammed Al Bagami completed MBBS at the King Faisal University – College of Medicine, Dammam, 1999-2004. He has completed his MSc in Therapeutic uses of Stem
Cells, Master II in 2012 – 2014 at Université de Picardie Jules Verne (Amiens). Currently, he is working as a PhD Scholar in Université de Picardie Jules Verne (Amiens). He
also has an experience in Clinical Fellow - Paediatric Hematology Oncology & BMT, CHU-Hôpitaux de Rouen, 2011 – 2013 (2 years); Clinical Fellow, Gustave Roussy, May
2012–October 2012 (6 months); Pediatric Resident, King Fahad Specialist Hospital Dammam, 2005–2007 (2 years), Pediatric Hematology/Oncology; Internship Training,
King Fahd Hospital of the University - AL-Khobar, August 2004 – July 2005 (1 year).