PMC/PubMed Indexed Articles
Indexed In
- Open J Gate
- Genamics JournalSeek
- SafetyLit
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
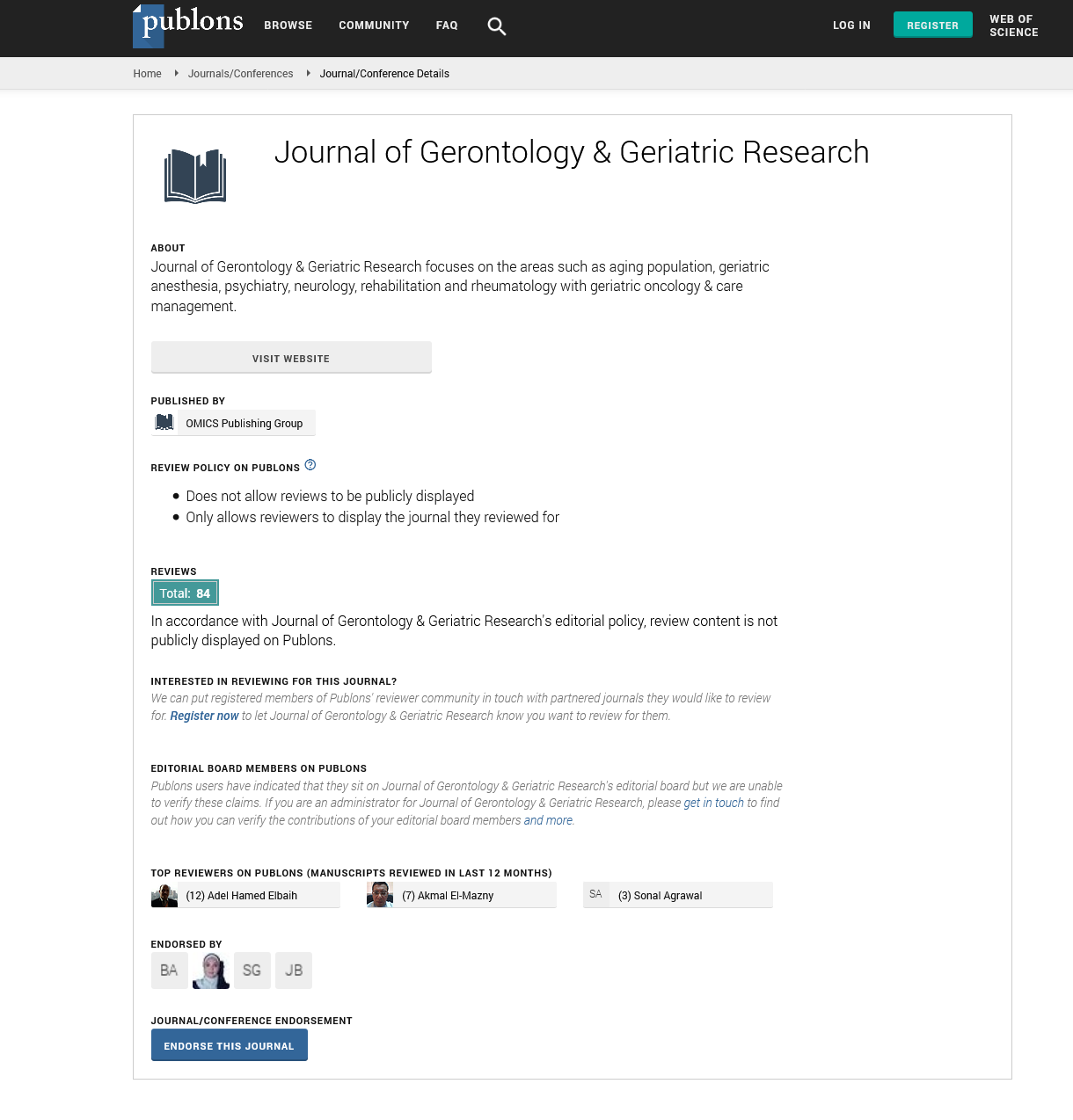
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
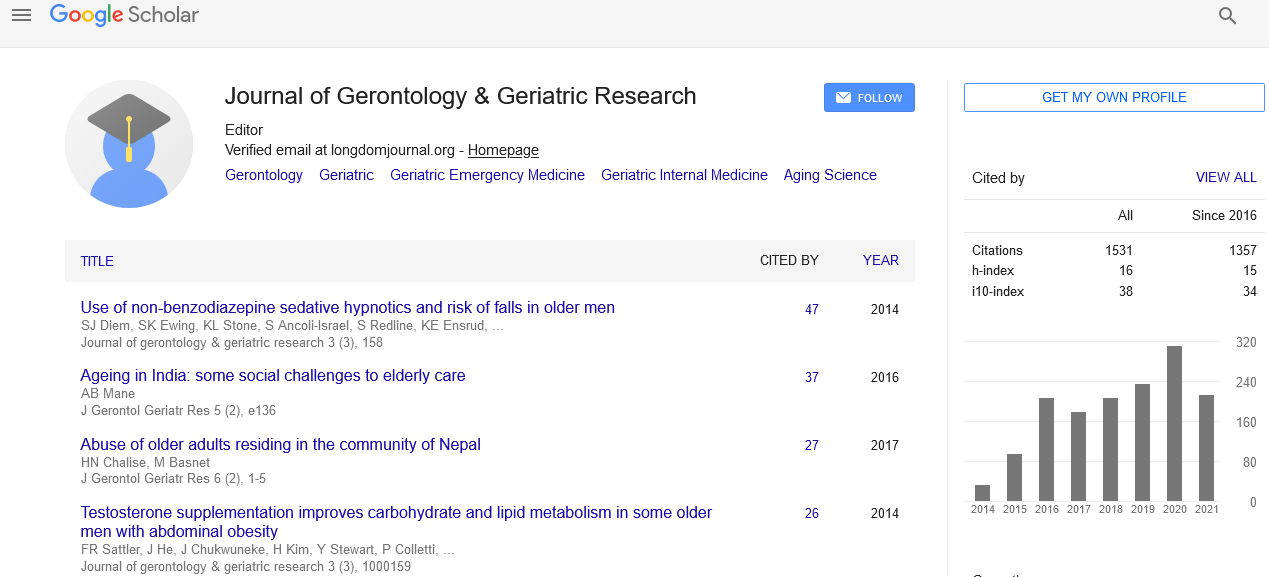
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
INTEGRATING FRAILTY AND MULTI-MORBID ASSESSMENT INTO HEART FAILURE MANAGEMENT DECISION-MAKING IN OLDER PATIENTS
2nd International Conference on Aging & Gerontology
June 26-27, 2017 San Diego, CA, USA
Nahid Azada
aUniversity of Ottawa, Canada
Posters & Accepted Abstracts: J Gerontol Geriatr Res
Abstract:
The phenotype of patients with cardiovascular disease (CVD) has changed substantially over the last 2 decades. Heart failure (HF) is considered the �??poster-child�?? of the blend of CVD and multi-morbidity in the aging population. Aging demographics indicate that HF cases will rise continuously over the next few decades. Care of these patients is often confounded by common geriatric conditions (e.g. dementia, frailty, falls, poly-pharmacy and medication intolerance) contributing to functional disability, poorer quality of life, and increase use of hospitalization. HF is significantly associated with more cognitive impairment and frailty resulting in increased vulnerability and reduced homeostatic reserve. These individuals consume more health care services and have worse clinical outcomes. The course of HF is characterized by periods of relative stability, punctuated by unpredictable exacerbations leading to emergency department visits and hospitalizations. Between 25 and 50% of individuals with HF can die suddenly. Those who escape sudden death experience over time and with each HF exacerbation, progressive loss of functional capacity. These individuals become increasingly reliant on family and community support services and ultimately many require institutionalization. At present, health care provision is too fragmented at a time when patient complexity is greater than ever. We need to fundamentally rethink the relationship between specialists and primary care and leverage capacity of all health professions to achieve better patient level and system level outcomes. Improved care of the older cardiac patient is based on collaboration and teamwork between the primary care physician, geriatrician, and cardiologist to accommodate the heterogeneity of aging, frailty, multi-morbidity, and the complexity of care delivery. Cardio-geriatric support is needed for primary care to establish more integrated care models at the ambulatory level and by providing comprehensive geriatric assessment in a proactive way to guide a care planning discussion, particularly at the advanced stage, focusing on patients�?? values and preferences.