Review Article Open Access
Endoscopic Retrograde Cholangiopancreatography: A Review of Technique and Clinical Indications
Kerollos N Wanis1, Samson Haimanot2 and Rani Kanthan3*
1College of Medicine, University of Saskatchewan, Saskatoon, Canada
2Department of Gastroenterology, University of Saskatchewan, Saskatoon, Canada
3Department of Pathology and Laboratory Medicine, University of Saskatchewan, Saskatoon, Canada
- Corresponding Author:
- Rani Kanthan
Room 2868 G-Wing
Royal University Hospital
103 Hospital Drive, Saskatoon
Saskatchewan, S7N 0W8, Canada
Tel: 3066552158
E-mail: rani.kanthan@saskatoonhealthregion.ca
Received Date: July 08, 2014; Accepted Date: August 05, 2014; Published Date: August 12, 2014
Citation: Wanis KN, Haimanot S and Kanthan R (2014) Endoscopic Retrograde Cholangiopancreatography: A Review of Technique and Clinical Indications. J Gastroint Dig Syst 4:208. doi:10.4172/2161-069X.1000208
Copyright: © 2014 Wanis KN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) was introduced over 4 decades ago. This challenging procedure has evolved significantly with experienced endoscopists performing this procedure safely and effectively with almost 100% biliary cannulation success rates. Since first used for biliary drainage in patients with choledocholithiasis, ERCP continues to play a critical role in the management of biliary and pancreatic diseases. Though currently it is almost exclusively used for therapeutic purposes, it remains an important tool in the investigation of biliary disease, particularly malignancy. In this focussed review, we discuss the history, technique, and current clinical indications for ERCP.
Keywords
Endoscopic retrograde cholangiopancreatography; Common bile duct; Choledocholithiasis
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) was introduced in 1968 by Drs. McCune, Shorb, and Moscovitz. This was the first time that endoscopy was used to visualise the common bile duct (CBD) and the pancreatic duct. The preliminary results had a poor success rates with failure in 50% of patients to reach the duodenum, and failure in another 50% to cannulate the ampulla of Vater [1]. Few years following this preliminary experience, several technological improvements to the duodenoscope were made to facilitate higher procedural success rates. The duodenoscope was redesigned, with a single side-viewing lens, and was lengthened with integration of a larger working channel [2]. Within 6 years of the first endoscopic visualisation of the common bile duct and pancreatic duct, endoscopic treatment of choledocholithiasis with sphincterotomy of the ampulla was first performed. Two cases of successful stone passage following sphincterotomy were described, and the value of ERCP as a therapeutic procedure was established [3].
Technique
ERCP can often be a longer duration procedure than other endoscopies, requiring patient co-operation, and carries additional risks. This combination of factors necessitates adequate and safe anesthetic sedation. While most ERCPs can be performed under conscious sedation, it is recommended that in high risk cardiopulmonary patients and patients who develop severe hypoxemia or hypotension, either before or during the ERCP should have a general anesthetic [4].
ERCP itself is a technically demanding procedure. Deep cannulation of the CBD is required for biliary interventions. A successful cannulation rate of over 80% requires 350-400 supervised procedures, and several hundred more procedures are required to achieve >96% success rates [5]. The overall success rate for experienced endoscopists in the community setting is reported to be around 94% [6]. Mechanical simulator practice could be an important adjunct in early clinical training to help trainees achieve the necessary competence for rapid and successful cannulation [7].
Given the relatively high rates of cannulation failure during ERCP and the important procedural risks, most notably post-ERCP pancreatitis, several techniques for successful deep cannulation of the CBD have emerged. The options for initial biliary cannulation include either a standard catheter or a sphincterotome, which differs from a standard catheter due to the presence of an electrosurgical cutting wire at the distal end of the catheter. This cutting wire, which is intended to incise the papilla after cannulation, also assists in alignment of the catheter for achieving successful duct cannulation. As such, use of a sphincterotome rather than a standard catheter has been shown to improve initial biliary cannulation success rates [8]. If the initial approach is unsuccessful, a guidewire can be used in conjunction with the sphincterotome to achieve deep cannulation. The guidewire is inserted, under fluoroscopy, in the direction of the CBD, and the sphincterotome can then be passed over the guidewire. This adjunct significantly improves primary biliary cannulation success rates [9].
If initial cannulation attempts are unsuccessful, further attempts at cannulation can exacerbate sphincter of Oddi spasm and edema which increases the risk of post-ERCP pancreatitis [10]. Therefore, initial cannulation should be supplemented with advanced techniques after several failed attempts [10,11]. The majority of endoscopists prefer to proceed with pre-cut sphincterotomy after initial failed cannulation [12], however incorporation of the double guide wire technique prior to pre-cut techniques has been shown by Vihervaara et al. to achieve a 99% success rate in experienced hands [13]. The double-guide wire technique involves first placing a guide wire into the pancreatic duct. This helps to stabilize the papilla and to block the pancreatic duct, helping to guide the second wire into the common bile duct. In a study by Ito et al. the double guide wire technique achieved successful primary biliary cannulation in 73% of patients with a difficult biliary cannulation, defined as unsuccessful cannulation within 15 minutes [14]. However, in a multicenter randomised controlled trial in which a difficult cannulation was defined as one that was unsuccessful after five attempts, the double guide wire technique did not expedite CBD cannulation and may have increased the risk of post-ERCP pancreatitis [15]. Therefore the timing of the double guide wire technique is an important consideration that calls into question the definition of a difficult cannulation. Thus, the ideal number of failed standard cannulation attempts prior to pancreatic duct guidewire placement is unclear, although five attempts has been suggested as a recommended figure [11]. Nevertheless, due to lack of robust evidence, the usefulness of the double guidewire technique versus pre-cut techniques has yet to be determined. With the pancreatic guide wire in place, a pancreatic stent can be passed into the duct if desired, to reduce the risk of post-ERCP pancreatitis [16]. A pancreatic duct stent may also help facilitate a pre-cut sphincterotomy if this is subsequently planned.
There are three pre-cut techniques which can be used to salvage a difficult cannulation: i) a cut can be made beginning at the superior border of the ampulla and extending in the cephalad direction (needle knife sphincterotomy; NKS), ii) a cut can be made beginning above the ampulla and exposing the distal common bile duct (needle knife fistulotomy; NKF), or iii) a sphincterotome can be passed over a pancreatic duct guidewire to create a pancreatic duct sphincterotomy in the direction of the common bile duct (pancreatic sphincterotomy; PS) [11]. Lim et al. examined the cannulation success rate with a protocol that employed NKF after initial failed cannulation. NKF was successful in 94.4% of patients in which initial cannulation failed, and the overall success rate of the ERCP procedure rose to 98.2%. Additionally, the rate of pancreatitis did not increase as a result of NKF [17]. In comparison, a study examining NKS demonstrated a success rate of 85% following failed initial cannulation, with an overall success rate of 97.7%. Similar to NKF, in multivariate analysis, NKS was not independently associated with incidence of post-ERCP pancreatitis [18]. Though there is limited data comparing the two techniques, a randomized trial comparing NKS versus NKF found similar cannulation success rates, but more frequent pancreatic complications in the NKS group [19]. Halttunen et al. demonstrated a very high success rate of 97.3% for pancreatic sphincterotomy in difficult cannulation cases. They also compared PS against NKS and found no difference in the rates of post-ERCP pancreatitis [20]. However, concern over the consequences of unnecessary pancreatic sphincterotomy still exists for this newer technique [8].
Role of ERCP in The Biliary Tract
Choledocholithiasis
The first therapeutic use of ERCP was in patients with common bile duct stones [3]. For diagnosis of CBD stones, ERCP has been replaced by less invasive modalities such as abdominal ultrasound, CT scan, endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP). In most cases, these modalities will identify the presence of choledocholithiasis. In the exceptional cases where choledocholithiasis is suspected but not identified, endoscopic ultrasound has been suggested as a preferred next-line diagnostic modality in order to avoid ERCP [21]. Currently, EUS is gaining popularly in most centres and often replaces MRCP as the primary imaging modality of choice for the diagnosis of CBD stones. However, there are still many clinical scenarios where an ERCP is required despite the lack of definitive pre-procedure imaging. This is often related to patients’ clinical presentations and the likelihood for the need of urgent intervention for definitive therapy (e.g. patients who are suspected to have ascending cholangitis).
The advantage of ERCP is that it is both diagnostic and therapeutic in choledocholithiasis. ERCP allows for biliary drainage as well as clearance of CBD stones. This was first shown in a landmark trial by Lai et al. who compared surgical drainage versus endoscopic drainage and found that ERCP was associated with a significantly lower mortality rate [22]. A later study demonstrated that delay of ERCP in patients with severe ascending cholangitis resulted in a significantly higher mortality and morbidity rate [23]. However, in patients with clinically mild cholangitis, delaying ERCP for a period of antibiotic therapy did not affect outcome and may allow for spontaneous passage of the CBD stone [23]. This finding, for mild cholangitis, was later challenged. Chak et al. and Khashab et al. demonstrated worse patient outcomes as measured by length of hospital stay, rate of ICU admission, and mortality rate for delayed ERCP [24,25]. As such, it is recommended that ERCP be performed within 24 to 48 hours in patients who respond to antibiotics, and urgently in patients with severe cholangitis [26].
In patients who have CBD stones, without ascending cholangitis, ERCP may still have a therapeutic role. This is particularly relevant in older patients who may not be suitable surgical candidates. These patients have not been shown to have increased ERCP procedure-related mortality and morbidity, and the prognosis is similar to that of a cohort of younger patients [27]. Thus age does not appear to be an independent limiting factor for ERCP, in contrast to cholecystectomy. Furthermore, Pereira-Lima et al. found that sphincterotomy alone reduced the long-term recurrence rate of biliary symptoms to 20.2% in patients with an in situ gallbladder, compared to 11% in patients who underwent cholecystectomy [28]. For patients who do undergo cholecystectomy, and present with retained or recurrent CBD stones, ERCP is the standard of care to avert the high risk of future complications (i.e. ascending cholangitis, recurrent pain, or acute gallstone pancreatitis). This holds true for patients of all age groups, as well as pregnant mothers [29].
Biliary Strictures
The most common causes of biliary strictures are postoperative (i.e. post-cholecystectomy, or post-biliary reconstruction), inflammatory (i.e. primary sclerosing cholangitis, or recurrent cholangitis), and malignancy. Other rare causes include trauma, ischemia, infections, and post-radiation [30]. The presence of a biliary stricture is usually diagnosed on the clinical presentation of biliary obstruction. ERCP has replaced surgery as the gold standard for both diagnosis of biliary strictures, and the treatment of benign biliary strictures.
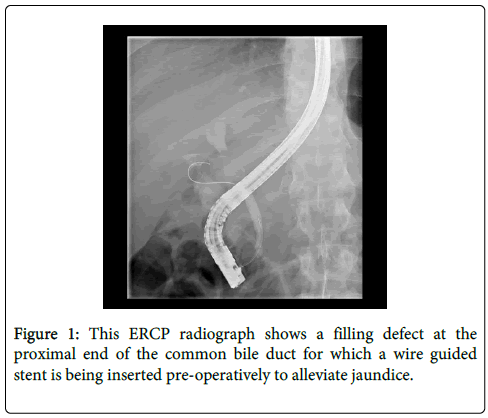
In patients who present with clinical biliary obstruction, the first step in work-up is to characterise the cause of the biliary obstruction, which should be done by MRCP or CT scan (to rule out an associated mass) [30]. Next, tissue diagnosis and evaluation of the appearance of the stricture should be performed by ERCP as shown in Figure 1. Brushings obtained from ERCP have been shown to have a nearly 100% specificity for cancer diagnosis, but with poor sensitivity of around 50% [31]. Newer techniques, including choledochoscopy and EUS have improved the diagnostic yield for accurately identifying malignant strictures by allowing the endoscopist to better target tissues that can increase the yield of sampling and thereby increase sensitivity of diagnosis [2,31].
The most common cause of benign post-operative biliary strictures is post-cholecystectomy. Endoscopic treatment for these patients involves stenting of the stricture, with stent replacements to prevent cholangitis, and eventual stent removal. Treatment of these strictures can often take up to 1 year with repeated ERCP sessions. The evidence supporting stenting of post-cholecystectomy strictures is excellent with long-term restenosis rates of 20-30% in patients successfully stented [32,33]. Draganov et al. achieved similar long-term success rates of 62% in patients with benign strictures of all etiologies, including post-operative, chronic pancreatitis, and idiopathic strictures [34]. This compares favourably with surgery, and avoids the high morbidity and mortality of biliary surgery (33.3% and 1.3% respectively in one large series) [35].
Biliary obstruction secondary to primary sclerosing cholangitis (PSC) may occur in the presence of a dominant stricture which is defined as a stenosis with a residual diameter of <1.5 mm in the CBD, or <1 mm in the hepatic duct [36]. These strictures occur in approximately half of patients with PSC [36]. Patients presenting with dominant strictures are at high risk of developing cholangiocarcinoma, so a thorough evaluation should be performed including MRI or CT scan, and CA 19-9 levels [37]. In this context, repeated ERCP should be performed for brushings and biopsies, with or without the aid of choledochoscopy. After malignancy has been excluded, therapeutic ERCP may be performed to relieve symptoms of pruritus or recurrent cholangitis. Dilation and stenting of dominant strictures has been shown to be equally efficacious. However, stenting carries the risk of bacterial cholangitis and therefore these patients require frequent stent changes [34,38]. As such, the American Association for the Study of Liver Diseases guidelines recommend endoscopic dilation with or without stenting as the initial management of patients with dominant strictures from PSC [36].
Cholangiocarcinoma
In patients who do develop cholangiocarcinoma, ERCP has a mainly diagnostic and palliative role. Though surgical resection is the only potential curative option, more than half of these patients present with unresectable disease [39]. For patients with cholangiocarcinoma distal to the hepatic duct bifurcation, a single stent is recommended to relieve jaundice [39]. However, evidence is lacking on the ideal management strategy for patients with hilar cholangiocarcinomas. Only 25% of the liver needs to be drained in order to resolve jaundice, so unilateral stenting is adequate and avoids the additional risks and expense of bilateral stenting [40,41]. We anticipate a large scale randomised controlled trial in the future to clarify the superior stenting strategy for these patients who have unresectable tumors. In patients with resectable tumors, the role of pre-operative biliary decompression is still debated, but has not been shown to improve overall clinical outcome and may be associated with increased length of hospital stay, especially if surgery is planned within two weeks of diagnosis [41,42]. This continues to be debated in the literature due to lack of prospective randomised trials. However, pre-operative biliary drainage is recommended in selected patients with cholangitis, long-standing jaundice, impaired renal function, and severe malnutritional state [42].
Biliary Ascariasis
Ascariasis is the most common parasitic infestation of the human gastrointestinal tract, infecting approximately one quarter of the world’s population [43]. Ascariasis is only the third most common helminithic infection in the United States, but is highly endemic in Africa, Latin America, India, and the Far East [43]. Adult ascaris worms typically inhabit the small bowel, and patients remain asymptomatic until an excessive worm load is present. When a large number of worms accumulates, they may enter the bile ducts through the ampulla of Vater causing biliary symptoms. However, biliary ascariasis only accounts for a small minority (10%-19%) of ascariasis related hospital admissions [43]. Furthermore, almost all patients with biliary ascariasis have a past history of cholecystectomy or endoscopic sphincterotomy [44]. Typically, biliary ascariasis can be diagnosed with ultrasound which has high sensitivity and specificity for the detection of adult worms [43]. ERCP is typically reserved for patients who do not respond to conservative antihelmith treatment, or for patients who develop serious complications such as ascending cholangitis. In these patients, ERCP both confirms the diagnosis and allows for successful clearance of the biliary ducts in almost all patients [44].
Ampullary tumors
ERCP mainly plays a diagnostic role in ampullary tumors. A side-facing endoscopy lens is required for adequate differentiation of the prominent ampulla, and tissue biopsies may easily be obtained using a side-viewing endoscope. ERCP may be used for additional pre-treatment staging of the lesion, since involvement of the common bile duct or pancreatic duct makes complete resection with endoscopic ampullectomy unlikely [45]. If ampullectomy is performed, ERCP facilitates placement of a pancreatic duct stent which reduces the risk of pancreatitis after ampullectomy [45]. Palliative stenting may also be performed in patients with ampullary adenocarcinoma who are not suitable for definitive resection [45].
Role of ERCP for Pancreatic Diseases
Acute pancreatitis
The timing and indication for ERCP in gallstone pancreatitis, though well explored in the literature, remains inconclusive. van Geenen et al. in an examination of 8 meta-analyses and 12 guidelines, concluded that ERCP with sphincterotomy does not have a clear advantage in mild pancreatitis, though pancreatitis with synchronous cholangitis requires urgent ERCP and sphincterotomy [46]. However, for patients with severe acute biliary pancreatitis, there has yet to be a definite answer as to whether early ERCP is indicated. In 1999, a meta-analysis by Sharma et al. found a significant reduction in mortality and morbidity in patients who had ERCP and sphincterotomy for severe acute gallstone pancreatitis. They recommended routine early ERCP for these patients [47]. However, a recent Cochrane systematic review addressed this question and concluded that, in the absence of co-existing cholangitis or biliary obstruction, early ERCP does not reduce mortality or morbidity in pancreatitis regardless of severity [48]. Differences in meta-analysis study selection is the likely explanation for these differing conclusions, and more studies in the future are required to definitively answer this question. Nonetheless, only one set of published guidelines does not recommend emergency ERCP in severe pancreatitis [46]. There continues to be lack of consensus on the indications, timing, and procedural techniques in acute severe biliary pancreatitis. Furthermore, this inconsistency is reflected in clinical practice with most (86%) endoscopists in a national survey among Dutch gastroenterologists ignoring national guidelines and opting against routine ERCP in severe gallstone pancreatitis [49].
Similarly to choledocholithiasis, high risk surgical patients, and elderly, with gallstone pancreatitis may be considered candidates for endoscopic sphincterotomy. Bignell et al. performed ERCP with sphincterotomy as definitive treatment for 101 patients with gallstone pancreatitis. Of these patients, 89 were treated successfully and 84 had no recurrence of pancreatitis over a mean follow-up of 41 months [50].
Chronic pancreatitis
Patients with chronic pancreatitis suffer from chronic pain and loss of exocrine and endocrine function. ERCP has a diagnostic role in chronic pancreatitis, as an adjunct to CT, EUS, and MRCP. It has a sensitivity of 71-93%, and a specificity of 89-100% for the diagnosis of chronic pancreatitis [51]. The main advantage of ERCP is its effectiveness in visualising the pancreatic duct anatomy, allowing it to identify the presence of strictures or stones. However, given the improvements in EUS and MRCP, ERCP now mainly plays a therapeutic role in the management of chronic pancreatitis.
Pancreatic duct leaks and pancreatic pseudocysts
Pancreatic duct leaks and pseudocysts may occur as complications of chronic pancreatitis. In pancreatic duct leaks, stenting of the pancreatic duct across the area of the leak may be performed, and is successful in approximately 60% of patients [51]. Pseudocysts, caused by chronic pancreatitis, have the potential to cause pain, gastric outlet obstruction, CBD obstruction, hemorrhage, and infection. While often challenging to treat, they may be endoscopically drained if they are symptomatic, infected, or progressively enlarging [51]. They are best handled by a multidisciplinary team including surgeons, gastroenterologists, and interventional radiologists [51].
Pancreatic duct strictures
ERCP can be used as a therapeutic modality in patients with pancreatic duct strictures for drainage of the main pancreatic duct. Firstly, in patients with a pancreatic duct stricture, malignancy must be considered and excluded. In the presence of pancreatic cancer obstructing the CBD, stenting is useful and cost-effective in the pre-operative period [51]. However, long-term drainage of the CBD with surgical reconstruction is necessary [51]. For patients with pancreatic strictures secondary to chronic pancreatitis, multiple endoscopic stenting has been shown to be feasible and safe, with excellent long-term results. Costamagna et al. followed 19 patients with severe chronic pancreatitis after stent removal and only 10.5% experienced symptomatic stricture recurrence [52].
Pancreatic duct stones
Unfortunately, compared to pancreatic strictures, the results are not as promising for patients with pancreatic duct stones. A randomized trial by Dite et al. found that surgery had higher rates of complete pain relief at 5 years (37% vs. 14% for ERCP), and that patients in the surgical group had better weight gain post-procedurally. However, exocrine function, as measured by the development of diabetes was equivalent in both groups [53]. Nonetheless, ERCP has been shown to provide good long term benefits for patients with pancreatic duct stones and it avoids the significant mortality and morbidity associated with pancreatic surgery [54].
Conclusions
ERCP continues to play an ongoing, important role in the diagnosis and management of biliary and pancreatic diseases. ERCP still remains the diagnostic gold-standard for the evaluation of morphological changes in the pancreas. In many cases, such as in common bile duct stones and pancreatic strictures, ERCP is the preferred modality for treatment. In other cases, ERCP can act as an alternative to surgery for high-risk surgical candidates. At tertiary centres, with high volumes of ERCPs, more ERCPs are being performed for patients with greater co-morbidities and advanced disease. There remain questions regarding the ideal use of ERCP in patients with hilar cholangiocarcinoma, and severe acute gallstone pancreatitis. Larger studies are expected in the future to help address these ongoing clinical debates.
References
- McCune WS, Shorb PE, Moscovitz H (1968) Endoscopic cannulation of the ampulla of vater: a preliminary report.Ann Surg 167: 752-756.
- Brody F, Vaziri K, Ponsky TA, Dunkin BJ (2010) The first endoscopic retrograde pancreatogram.SurgEndosc 24: 1055-1059.
- Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y (1974) Endoscopic sphincterotomy of the ampulla of Vater.GastrointestEndosc 20: 148-151.
- Kapoor H (2011) Anaesthesia for endoscopic retrograde cholangiopancreatography.ActaAnaesthesiolScand 55: 918-926.
- Verma D, Gostout CJ, Petersen BT, Levy MJ, Baron TH, et al. (2007) Establishing a true assessment of endoscopic competence in ERCP during training and beyond: a single-operator learning curve for deep biliary cannulation in patients with native papillary anatomy. GastrointestEndosc 65: 394-400.
- Colton JB, Curran CC (2009) Quality indicators, including complications, of ERCP in a community setting: a prospective study.GastrointestEndosc 70: 457-467.
- Lim BS, Leung JW, Lee J, Yen D, Beckett L, et al. (2011) Effect of ERCP mechanical simulator (EMS) practice on trainees' ERCP performance in the early learning period: US multicenter randomized controlled trial.Am J Gastroenterol 106: 300-306.
- Freeman ML, Guda NM (2005) ERCP cannulation: a review of reported techniques.GastrointestEndosc 61: 112-125.
- Cheung J, Tsoi KK, Quan W, Lau JYW, Sung JJY (2009) Guidewire versus conventional contrast cannulation of the common bile duct for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. GastrointestEndosc 70: 1211-1219.
- Zhou W, Li Y, Zhang Q, Li X, Meng W, et al. (2011) Risk Facotrs for Postendoscopic Retrograde Cholangiopancreatography Pancreatitis: A Retrospective Analysis of 7,168 Cases. Pancreatology 11: 399-405
- Testoni PA, Testoni S, Giussani A (2011) Difficult biliary cannulation during ERCP: how to facilitate biliary access and minimize the risk of post-ERCP pancreatitis.Dig Liver Dis 43: 596-603.
- Lohr JM, Aabaken L, Arnelo U, Gronroos J, Halttunen J, et al. (2012) How to cannulate? A survey of the Scandinavian Association for Digestive Endoscopy (SADE) in 141 endoscopists. Scandinavian Journal of Gastroenterology 47: 861-869.
- Vihervaara H, Grönroos JM (2012) Feasibility of the novel 3-step protocol for biliary cannulation--a prospective analysis.SurgLaparoscEndoscPercutan Tech 22: 161-164.
- Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, et al. (2008) Pancreatic guidewire placement for achieving selective biliary cannulation during endoscopic retrograde cholangio-pancreatography.World J Gastroenterol 14: 5595-5600.
- Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Espinel J, et al. (2009) Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial.GastrointestEndosc 70: 700-709.
- Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, et al. (2010) Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation? A prospective randomized controlled trial. J Gastroenterol 45: 1183-1191.
- Lim JU, Joo KR, Cha JM, Shin HP, Lee JI, et al. (2012) Early use of needle-knife fistulotomy is safe in situations where difficult biliary cannulation is expected.Dig Dis Sci 57: 1384-1390.
- Bailey AA, Bourke MJ, Kaffes AJ, Byth K, Lee EY, et al. (2010) Needle-knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis (with video).GastrointestEndosc 71: 266-271.
- Mavrogiannis C, Liatsos C, Romanos A, Petoumenos C, Nakos A, et al. (1999) Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones.GastrointestEndosc 50: 334-339.
- Halttunen J, Keränen I, Udd M, Kylänpää L (2009) Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation.SurgEndosc 23: 745-749.
- Chen CC (2012) The efficacy of endoscopic ultrasound for the diagnosis of common bile duct stones as compared to CT, MRCP, and ERCP.J Chin Med Assoc 75: 301-302.
- Lai EC, Mok FP, Tan ES, Lo CM, Fan ST, et al. (1992) Endoscopic biliary drainage for severe acute cholangitis.N Engl J Med 326: 1582-1586.
- Boender J, Nix GA, de Ridder MA, Dees J, Schütte HE, et al. (1995) Endoscopic sphincterotomy and biliary drainage in patients with cholangitis due to common bile duct stones.Am J Gastroenterol 90: 233-238.
- Chak A, Cooper GS, Lloyd LE, Hammar PJ, Issa K, et al. (2000) Effectiveness of ERCP in cholangitis: a community-based study.GastrointestEndosc 52: 484-489.
- Khashab MA, Tariq A, Tariq U, Kim K, Ponor L, et al. (2012) Delayed and Unsuccessful Endoscopic Retrograde Cholangiopancreatography Are Associated With Worse Outcomes in Patients With Acute Cholangitis. Clinical Gastroenterology and Hepatology 10: 1157-1161.
- Kinney TP (2007) Management of ascending cholangitis.GastrointestEndoscClin N Am 17: 289-306, vi.
- Obana T, Fujita N, Noda Y, Kobayashi G, Ito K, et al. (2010) Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients.Intern Med 49: 1935-1941.
- Pereira-Lima JC, Jakobs R, Winter UH, Benz C, Martin WR, et al. (1998) Long-term results (7 to 10 years) of endoscopic papillotomy for choeldocholithiasis. Multivariate analysis of prognostic factors for recurrence of biliary symptoms. GastrointestEndosc 48: 457-464.
- Carr-Locke DL (2002) Therapeutic role of ERCP in the management of suspected common bile duct stones.GastrointestEndosc 56: S170-174.
- Chan CH, Telford JJ (2012) Endoscopic management of benign biliary strictures.GastrointestEndoscClin N Am 22: 511-537.
- Dumonceau JM (2012) Sampling at ERCP for cyto- and histopathologicical examination.GastrointestEndoscClin N Am 22: 461-477.
- Kassab C, Prat F, Liguory C, Meduri B, Ducot B, et al. (2006) Endoscopic management of post-laparoscopic cholecystectomy biliary strictures. Long-term outcome in a multicenter study.GastroenterolClinBiol 30: 124-129.
- Bergman JJ, Burgemeister L, Bruno MJ, Rauws EA, Gouma DJ, et al. (2001) Long-term follow-up after biliary stent placement for postoperative bile duct stenosis.GastrointestEndosc 54: 154-161.
- Draganov P, Hoffman B, Marsh W, Cotton P, Cunningham J (2002) Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents.GastrointestEndosc 55: 680-686.
- Sikora SS, Pottakkat B, Srikanth G, Kumar A, Saxena R, et al. (2006) Postcholecystectomy benign biliary strictures - long-term results.Dig Surg 23: 304-312.
- Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, et al. (2010) Diagnosis and management of primary sclerosing cholangitis.Hepatology 51: 660-678.
- Chapman MH, Webster GJ, Bannoo S, Johnson GJ, Wittmann J, et al. (2012) Cholangiocarcinoma and dominant strictures in patients with primary sclerosing cholangitis: a 25-year single-centre experience.Eur J GastroenterolHepatol 24: 1051-1058.
- Singh S, Talwalkar JA (2013) Primary sclerosing cholangitis: diagnosis, prognosis, and management.ClinGastroenterolHepatol 11: 898-907.
- Coelho-Prabhu N, Baron TH (2010) Endoscopic retrograde cholangiopancreatography in the diagnosis and management of cholangiocarcinoma.Clin Liver Dis 14: 333-348.
- Yasuda I, Mukai T, Moriwaki H (2013) Unilateral versus bilateral endoscopic biliary stenting for malignant hilar biliary strictures.Dig Endosc 25 Suppl 2: 81-85.
- Parodi A, Fisher D, Giovannini M, Baron T, Conio M (2012) Endoscopic management of hilarcholangiocarcinoma.Nat Rev GastroenterolHepatol 9: 105-112.
- El-Hanafy E (2010) Pre-operative biliary drainage in hilarcholangiocarcinoma, benefits and risks, single center experience.Hepatogastroenterology 57: 414-419.
- Shah OJ, Zargar SA, Robbani I (2006) Biliary ascariasis: a review.World J Surg 30: 1500-1506.
- Sandouk F1, Haffar S, Zada MM, Graham DY, Anand BS (1997) Pancreatic-biliary ascariasis: experience of 300 cases.Am J Gastroenterol 92: 2264-2267.
- El Hajj II, Coté GA (2013) Endoscopic diagnosis and management of ampullary lesions.GastrointestEndoscClin N Am 23: 95-109.
- van Geenen EJ, van Santvoort HC, Besselink MG, van der Peet DL, van Erpecum KJ, et al. (2013) Lack of consensus on the role of endoscopic retrograde cholangiography in acute biliary pancreatitis in published meta-analyses and guidelines: a systematic review.Pancreas 42: 774-780.
- Sharma VK, Howden CW (1999) Metaanalysis of Randomized Controlled Trials of Endoscopic Retrograde Cholangiography and Endoscopic Sphincterotomy for the Treatment of Acute Biliary Pancreatitis. Am Coll of Gastoenterology 94: 3211-3214.
- Tse F, Yuan Y (2012) Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis (Review). Cochrane Database Syst Rev CD009779.
- Van Geenen EM, Mulder CJJ, Van Der Peet DL, Fockens P, Bruno MJ (2010) Endoscopic treatment of acute biliary pancreatitis: A national survey among Dutch gastroenterologists. Scandinavian Journal of Gastroenterology 45: 1116-1120.
- Bignell M, Dearing M, Hindmarsh A, Rhodes M (2011) ERCP and Endoscopic Sphincterotomy (ES): A Safe and Definitive Management of Gallstone Pancreatitis with the Gallbladder Left In Situ. J GastrointestSurg 15: 2205-2210.
- Christodoulou DK, Tsianos EV (2010) Role of endoscopic retrograde cholangiopancreatography in pancreatic diseases.World J Gastroenterol 16: 4755-4761.
- Costamagna G, Bulajic M, Tringali A, Pandolfi M, Gabbrielli A, et al. (2006) Multiple stenting of refractory pancreatic duct strictures in severe chronic pancreatitis: long-term results.Endoscopy 38: 254-259.
- Díte P, Ruzicka M, Zboril V, Novotný I (2003) A prospective, randomized trial comparing endoscopic and surgical therapy for chronic pancreatitis.Endoscopy 35: 553-558.
- Delhaye M, Arvanitakis M, Verset G, Cremer M, Deviere J (2004) Long-term Clinical Outcome After Endoscopic Pancreatic Ductal Drainage for Patients With Painful Chronic Pancreatitis. Clinical Gastroenterology and Hepatology 2: 1096-1106.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 18701
- [From(publication date):
August-2014 - Sep 26, 2024] - Breakdown by view type
- HTML page views : 13835
- PDF downloads : 4866