Commentary Open Access
Full Thickness Local Excision of Large Rectal Tumour Using A Megawindows 36 Millimetres Circular Stapler
Pierpaolo Sileri*, Luana Franceschilli, Ilaria Capuano, Marilena Raniolo and Achille L Gaspari
Department of Experimental Medicine and Surgery, University of Rome Tor Vergata, Rome, Italy
- Corresponding Author:
- Pierpaolo Sileri
Cattedra Chirurgia Generale
Policlinico Tor Vergata
6B Viale Oxford 81, 00133, Rome, Italy
Tel: +393339137249
Fax: +390620902927
E-mail: piersileri@yahoo.com
Received Date: June 06, 2014; Accepted Date: July 29, 2014; Published Date: August 02, 2014
Citation: Sileri P, Franceschilli L, Capuano I, Raniolo M, Gaspari AL (2014) Full Thickness Local Excision of Large Rectal Tumour Using A Megawindows 36 Millimetres Circular Stapler. J Gastroint Dig Syst 4:201. doi:10.4172/2161-069X.1000201
Copyright: © 2014 Sileri P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Introduction
Colorectal adenomas are frequent in the western countries. The estimated lifetime risk is approximately 40% [1]. One third of these lesions will develop in the rectum and about 10% will become malignant [2]. Moreover, the widespread of colorectal cancer screening will necessarily lead to increased detection of adenomas and early rectal cancer. Therefore, more rectal lesions will probably undergo endoscopic or surgical management in the next years.
The presence or absence of malignant cells in a lesion can be diagnosed only after complete excision (total biopsy) and the incidence of unexpected invasive carcinoma after polyp removal can be as high as 20% [3].
Adenomatous rectal lesions not endoscopically removable (large, sessile or carpet-like polyps) need to be treated with surgical excision. Similarly, unexpected malignant polyps at endoscopy are referred to surgery to perform full thickness ‘total biopsy’.
Local excision is the treatment of choice and several techniques have been proposed. The excision of an intact tumour is mandatory to obtain lower recurrence rate and morbidity [4].
When a complete local excision is achieved with adequate superficial and deep margins, surgery is curative even in polyps containing carcinoma in situ (Tis) or initially invasive cancer with infiltration limited to the submucosal layer (T1).
Local excision of a rectal lesion can be a straight forward or, on the contrary, a demanding procedure due to the narrow space in which the surgeon must work, due to the difficulty of getting a satisfactory exposure and due to other factors, such as some characteristics of the polyp itself (size, morphology, nature, distance from the anal verge, longitudinal extension) or extrinsic factors like patient’s constitution and health, rectal mobility, surgeon’s experience [5,6].
The three approaches for local surgical excision are:
a) Kraske dorsal access or the Mason trans-sphincteric approaches or a combination of the two techniques. They offer a good exposure and are very effective from an oncological point of view, but they come with high complication rates, mainly infections and possible development of a faecal fistula [7,8].
b) Parks transanal approach (and its variations according to Francillon and Faivre) is the most common one for tumour located up to 12 cm from the anal verge. In expert hands, recurrence rate is low, approximately 10%, but can be as high as 36%, with major complications. The tumour is excised using a diathermy or harmonic scalpel [9].
Obviously, transanal approach has some limits: reduced space for surgical manipulation, difficult bleeding control (especially for posterior tumours) and incomplete field view (especially for higher tumours). Consequently, incomplete and imprecise resection may follow.
c) The Transanal Endoscopic Microsurgery (TEM) that allows a full thickness resection under an excellent view of the entire rectum (up to 18 cm from the anal verge). Limits are the device cost and learning curve [10].
Recently, the Transanal minimally invasive surgery (TAMIS) has been proposed with an immediate widespread worldwide. It is a technique developed as a low-cost alternative to TEM for local excision of carefully selected rectal neoplasms. It implies the use of ports for trans-anal access, pneumorectum, similarly to the standard TEM but with lower costs and comparable results [11].
Endoscopic linear stapler-cutter for trans-anal removal of rectal lesions has also been reported in literature. Indeed, staplers can offer the possibility of complete and safe excision with accurate haemostasis. Indications include rectal large lesions, polyps with dysplasia and in situ carcinoma. This procedure provides an easier access than TEM, decrease of bleeding, minimal operative time and shorter hospital stay. However, T1 rectal cancer has not been treated with this technique [12-15]. In fact, even with prolapsing rectal mucosa, a full thickness resection can be difficult to achieve. Differently, the use of a circular stapler similarly to a stapled transanal rectal resection for obstructed defaecation allows a full thickness resection despite, to date, this application has not been reported by others [16].
Local excision of a rectal lesion using a circular stapler allows a standardized and straight forward procedure, overcoming the limiting factors for a successful surgery previously described. The conclusions of our previous experience using this approach indicated that it can be reserved to the full thickness removal of intact flat lesions (sessile or carpet like polyps), T1 is the cancer with a diameter up to 2 cm and located within 12 centimetres from the anal verge. Some limits were the lack of vision during the rectal wall traction within the stapler, especially for higher lesions, as well as the little volume of resectable tissue due to the circular stapler head encase. Recently, the availability of a large volume stapler with an encase of a 36 mm might overcome these limits. The larger encase that may host up to 35 centimetres cubes of tissue, might allow full thickness removal of larger tumour. Furthermore, since the stapler has a fenestrated head encase with mega-windows for each quadrant, it allows a resection under direct vision.
Surgical Technique
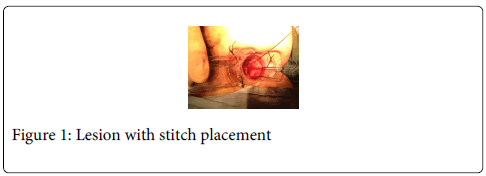
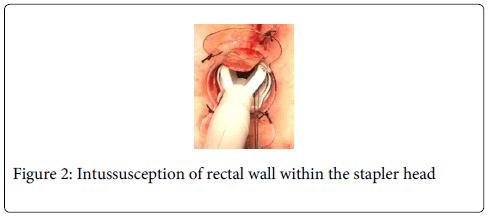
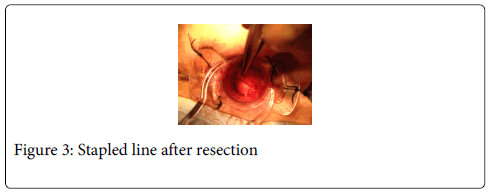
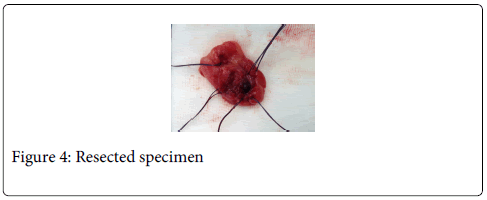
Disposable circular anal dilator and a purse-string suture anoscope are used (TST-plus, Touchstone Ltd, China). Anal verge is gently lubricated and digitally dilated for 1 minute with two fingers. The lubricated obturator is then inserted and left in situ for 1-2 minutes. At this point radial 4 stitches (0 silk) are used to expose the anal verge and to fix to the perianal skin the anal dilator. Absorbable 2-0 sutures are positioned at least 1 cm all around the rectal lesion on macroscopically free margins. Stitches should include mucosa, submucosa, and rectal muscle wall. A total of 6 to 8 sutures are positioned in a parachute manner (Figure 1). A 36 mm circular stapler is then opened and the head inserted above the lesion and the upper suture. All the sutures are inserted into the stapler through the stapler windows and pulled down. This way, the rectal wall including the lesion should create an intussusception within the stapler head (Figure 2). The stapler is then closed, hold for 30 seconds and fired. Occasionally a minimal mucosal bridge with a staple connecting the two edges may occur and is easily cut using heavy scissors. If bleeding occurs the suture line can be reinforced using interrupted vicryl 000. (Figure 3) The retrieved specimen is then oriented, pinned on a cork pad, properly labelled, and sent for pathology evaluation (Figure 4).
In our experience this technique overcomes some of the limits of incomplete surgical field exposure and difficult manipulation.
References
- Leslie A, Carey FA, Pratt NR, Steele RJ (2002) The colorectal adenoma-carcinoma sequence. Br J Surg 89: 845-860.
- Giuliani A, Caporale A, Corona M, Ricciardulli T, Di Bari M, et al. (2006) Large size, villous content and distal location are associated with severe dysplasia in colorectal adenomas. Anticancer Res 26: 3717-3722.
- Ramirez JM, Aguilella V, Gracia JA, Ortego J, Escudero P, et al. (2009) Local full-thickness excision as first line treatment for sessile rectal adenomas: long-term results. Ann Surg 249: 225-228.
- Fucini C, Segre D, Trompetto M (2004) Local excision of rectal polyp: indications and techniques. Tech Coloproctol 8 Suppl 2: s300-304.
- Stamos MJ, Murrell Z (2007) Management of early rectal T1 and T2 cancers. Clin Cancer Res 13: 6885s-9s.
- Chorost MI, Petrelli NJ, McKenna M, Kraybill WG, Rodriguez-Bigas MA (2001) Local excision of rectal carcinoma. Am Surg 67: 774-779.
- Gilbertas A, Meyer P (1973) [Kraske's posterior approach in the treatment of villous tumors of the rectum]. Chirurgie 99: 337-342.
- Mason AY (1977) Transsphincteric approach to rectal lesions. SurgAnnu 9: 171-194.
- Parks AG (1968) A technique for excising extensive villous papillomatous change in the lower rectum. Proc R Soc Med 61: 441-442.
- Buess G, Kipfmüller K, Ibald R, Heintz A, Hack D, et al. (1988) Clinical results of transanal endoscopic microsurgery. SurgEndosc 2: 245-250.
- Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW (2013). Transanal minimally invasive surgery (TAMIS) for locale excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum 56: 301-307.
- Allison SI, Adedeji A, Varma JS (2001) Per anal excision of large rectal adenomas using an endoscopic stapler. J R CollSurgEdinb 46: 290-291.
- De Gennaro VA, Lescher TC (1995) Transanal excision of rectal tumors using a laparoscopic stapler. Dis Colon Rectum 38: 327-328.
- Miskowiak J, Lindenberg S (1986) Excision of rectal villous adenoma using a TA or GIA stapler. Br J Surg 73: 630.
- Monalto G, Polinari U, Ausania F, Pende V, Coppola R, et al. (2008) Role of the endo-GIA stapler in transanal excision of rectal tumours. Can J Surg 51: E42-43.
- Sileri P, Stolfi VM, Palmieri G, Benavoli D, D' Ugo S, et al. (2010) Modified stapled transanal rectal resection (Starr) for full thickness excision of rectal tumour. J GastrointestSurg 14: 739-742.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14456
- [From(publication date):
August-2014 - Sep 19, 2024] - Breakdown by view type
- HTML page views : 10037
- PDF downloads : 4419