Editorial Open Access
N3 Fatty Acids and Neurodegeneration: Is it Enough to Stop or to Shift?
Luigi Iuliano*, Giuseppina Palmaccio, Annagiulia Bottaccioli and Chiara Zerbinati
Department of Medico-Surgical Sciences and Biotechnology, Vascular Biology and Mass Spectrometry Laboratory, Sapienza University of Rome, Latina, Italy
- Corresponding Author:
- Luigi Iuliano
Department of Medico-Surgical Sciences and Biotechnology
Vascular Biology and Mass Spectrometry Laboratory
Sapienza University of Rome, Latina, Italy
Tel: +39-0773-3175-7231
Fax: +39-066-229-1089
E-mail: luigi.iuliano@uniroma1.it
Received date: August 13, 2012; Accepted date: August 14, 2012; Published date: August 16, 2012
Citation: Iuliano L, Palmaccio G, Bottaccioli A, Zerbinati C (2012) N3 Fatty Acids and Neurodegeneration: Is it Enough to Stop or to Shift? J Alzheimers Dis Parkinsonism 2:e119. doi:10.4172/2161-0460.1000e119
Copyright: © 2012 Iuliano L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
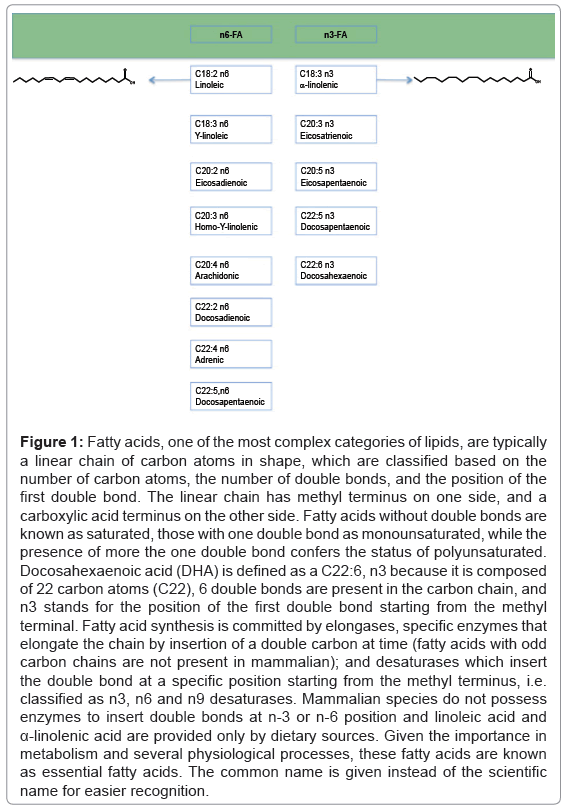
A recent large intervention study has showed no effect of dietary doses of n3 fatty acids (FA) on global cognitive decline in coronary heart disease patients [1]. N3-FA, which include α-linoleic acid, eicosapentaenoic acid (EPA) and docosapentaenoic acid (DHA) (Figure 1), have been subject of intense investigation in the recent years for expected benefits in delaying cognitive decline. Previous epidemiological and experimental animal studies suggested that deficiency in n3-FA, in particular DHA that is one of the most represented fatty acid in the brain, accelerates cognitive decline and increases the risk of developing AD [2-7]. With the Geleijnse’s trial, is it enough to suggest stopping investigation on n3-FA in the context of cognitive decline in man?
The disappointing results of the work of Geleijnse et al. [1] come after other clinical trials of EPA-DHA intake and cognitive function. Terano et al. [8] showed that 720 mg/d of DHA reduced the rate of cognitive decline over 3 and 6 months, but not over one year of follow up in 20 Japanese elderly patients who suffered a thrombotic stroke. In a 6-month trial, in 174 Alzheimer’s disease patients, no effect of EPA– DHA (2300 mg/d) on cognitive performance was found, except in a small subgroup with mild cognitive impairment [9]. Rogers et al. [10] found no effect of EPA–DHA (1500 mg/d) on cognitive function in 190 depressed U.K. adults after 12 weeks of treatment. In a 6-month trial, in 302 healthy Dutch subjects aged 65 years, EPA–DHA doses of either 400 mg/d or 1800 mg/d did not affect any of the cognitive domains studied [11]. Dangour et al. [12] assigned 867 subjects aged 70 to 79 years and without cognitive impairment to 700 mg of EPA-DHA (ratio of 2:5) or olive oil for 2 years. A large number of cognitive tests were applied, none of which was significantly influenced by treatment [12]. A recent well-conducted trial, enrolling 402 patients and designed to determine if treatment with DHA improved the symptoms and course of patients with mild to moderate Alzheimer disease, did not find treatment group differences on any of the primary or secondary outcomes despite elevations of plasma phospholipids and cerebrospinal fluid DHA [13]. It has also to consider that no relationship between serum n3-PUFA and AD or other forms of dementia was found in the Canadian Study of Aging and Dementia [14].
Figure 1: Fatty acids, one of the most complex categories of lipids, are typically a linear chain of carbon atoms in shape, which are classified based on the number of carbon atoms, the number of double bonds, and the position of the first double bond. The linear chain has methyl terminus on one side, and a carboxylic acid terminus on the other side. Fatty acids without double bonds are known as saturated, those with one double bond as monounsaturated, while the presence of more the one double bond confers the status of polyunsaturated. Docosahexaenoic acid (DHA) is defined as a C22:6, n3 because it is composed of 22 carbon atoms (C22), 6 double bonds are present in the carbon chain, and n3 stands for the position of the first double bond starting from the methyl terminal. Fatty acid synthesis is committed by elongases, specific enzymes that elongate the chain by insertion of a double carbon at time (fatty acids with odd carbon chains are not present in mammalian); and desaturases which insert the double bond at a specific position starting from the methyl terminus, i.e. classified as n3, n6 and n9 desaturases. Mammalian species do not possess enzymes to insert double bonds at n-3 or n-6 position and linoleic acid and α-linolenic acid are provided only by dietary sources. Given the importance in metabolism and several physiological processes, these fatty acids are known as essential fatty acids. The common name is given instead of the scientific name for easier recognition
Taken together, these data should restrain the emphasis on beneficial effects of n3 fatty acids and help to shift towards little studied fatty acids.
The intense investigation conducted with n3-FA contrasts with the paucity of studies concerning the effects of other FA in neurodegeneration and ageing, including the essential fatty acid linoleic acid (LA), which belongs to the n6 class of FA (Figure 1). The interest in n3-FA can be found in the seminal studies on anti-inflammatory actions opposed to n6-FA, which are thought of in a negative context because n6-FA are putative delivers of bioactive inflammatory eicosanoids, leading to a hugely popular theory of balance between proinflammatory n6-PUFA and anti-inflammatory n3-FA. In this context, the potential harmful effects of n3-FA associated with their sheer oxidizability, leading to the formation of bioactive docosanoids and neuroketals [15,16], has not usually been a matter of concern.
n spite of the popular, yet unproven, theory of “nonbeneficial” n6-FA, a recent clinical trial of linoleic acid supplementation in man showed that high-dose n6-FA intake did not cause any sign of inflammation or oxidative stress [17]. It is worthy to mention that linoleic acid has several beneficial effects - including lowering of blood pressure and blood cholesterol, and inhibition of platelet aggregation - implicated in the reduced risk of lacunar infarction and protection against ischemic stroke [18]. A neuroprotective effect of n6-FA [19] and a linear, inverse, association between the risk of Alzheimer disease and intake of n6-FA have been reported [20]. Interestingly, a recent study reported that linoleic acid, dose dependently, acts as anticonvulsant in a seizure rat model [21].
Studies focusing on dietary supplementation with arachidonic acid, a downstream product of linoleic acid, showed improvement of membrane fluidity, synaptic plasticity, and spatial cognition in aged rats [2,22,23]. Arachidonic acid was also reported to be a survival molecule for glial cells [24], and to be decreased in postmortem brain tissue from Alzheimer disease and schizophrenic patients [25-28]. Studies in other clinical settings further support a potential useful role of n6-FA. A diet high in vegetable n6-FA decreased abdominal fat and ameliorated insulin resistance compared to saturated fat [29]. In addition, linoleic acid has been inversely related to alanine aminotransferases in blood [30].
Nutritional strategies may be relevant tools to counteract cognitive decline, for which there is no substantial treatment to date, and among them lipids are striking candidates. However, theory needs experimental support to effectively translate into medicine. There is enough data to redirect research on fatty acids and cognitive decline by shifting towards a little explored class of fatty acids, the n6-FA.
References
- Geleijnse JM, Giltay EJ, Kromhout D (2012) Effects of n-3 fatty acids on cognitive decline: A randomized, double-blind, placebo-controlled trial in stable myocardial infarction patients. Alzheimers Dement 8: 278-287.
- Kotani S, Nakazawa H, Tokimasa T, Akimoto K, Kawashima H, et al. (2003) Synaptic plasticity preserved with arachidonic acid diet in aged rats. Neurosci Res 46: 453-461.
- Larrieu S, Letenneur L, Berr C, Dartigues JF, Ritchie K, et al. (2004) Sociodemographic differences in dietary habits in a population-based sample of elderly subjects: the 3C study. J Nutr Health Aging 8: 497-502.
- Conquer JA, Tierney MC, Zecevic J, Bettger WJ, Fisher RH (2000) Fatty acid analysis of blood plasma of patients with Alzheimer's disease, other types of dementia, and cognitive impairment. Lipids 35: 1305-1312.
- Barberger-Gateau P, Letenneur L, Deschamps V, Pérès K, Dartigues JF, et al. (2002) Fish, meat, and risk of dementia: cohort study. BMJ 325: 932-933.
- Tully AM, Roche HM, Doyle R, Fallon C, Bruce I, et al. (2003) Low serum cholesteryl ester-docosahexaenoic acid levels in Alzheimer's disease: a case-control study. Br J Nutr 89: 483-489.
- Cunnane SC, Plourde M, Pifferi F, Bégin M, Féart C, et al. (2009) Fish, docosahexaenoic acid and Alzheimer's disease. Prog Lipid Res 48: 239-256.
- Terano T, Fujishiro S, Ban T, Yamamoto K, Tanaka T, et al. (1999) Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids 34: S345-S346.
- Freund-Levi Y, Eriksdotter-Jönhagen M, Cederholm T, Basun H, Faxén-Irving G, et al. (2006) Omega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: a randomized double-blind trial. Arch Neurol 63: 1402-1408.
- Rogers PJ, Appleton KM, Kessler D, Peters TJ, Gunnell D, et al. (2008) No effect of n-3 long-chain polyunsaturated fatty acid (EPA and DHA) supplementation on depressed mood and cognitive function: a randomised controlled trial. Br J Nutr 99: 421-431.
- van de Rest O, Geleijnse JM, Kok FJ, van Staveren WA, Dullemeijer C, et al. (2008) Effect of fish oil on cognitive performance in older subjects: a randomized, controlled trial. Neurology 71: 430-438.
- Dangour AD, Allen E, Elbourne D, Fasey N, Fletcher AE, et al. (2010) Effect of 2-y n-3 long-chain polyunsaturated fatty acid supplementation on cognitive function in older people: a randomized, double blind, controlled trial. Am J Clin Nutr 91: 1725-1732.
- Quinn JF, Raman R, Thomas RG, Yurko-Mauro K, Nelson EB, et al. (2010) Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. JAMA 304: 1903-1911.
- Kröger E, Verreault R, Carmichael PH, Lindsay J, Julien P, et al. (2009) Omega-3 fatty acids and risk of dementia: the Canadian Study of Health and Aging. Am J Clin Nutr 90: 184-192.
- Bernoud-Hubac N, Davies SS, Boutaud O, Montine TJ, Roberts LJ 2nd (2001) Formation of highly reactive gamma-ketoaldehydes (neuroketals) as products of the neuroprostane pathway. J Biol Chem 276: 30964-30970.
- Fam SS, Murphey LJ, Terry ES, Zackert WE, Chen Y, et al. (2002) Formation of highly reactive A-ring and J-ring isoprostane-like compounds (A4/J4-neuroprostanes) in vivo from docosahexaenoic acid. J Biol Chem 277: 36076-36084.
- Bjermo H, Iggman D, Kullberg J, Dahlman I, Johansson L, et al. (2012) Effects of n-6 PUFAs compared with SFAs on liver fat, lipoproteins, and inflammation in abdominal obesity: a randomized controlled trial. Am J Clin Nutr 95: 1003-1012.
- . Iso H, Sato S, Umemura U, Kudo M, Koike K, et al. (2002) Linoleic acid, other fatty acids, and the risk of stroke. Stroke 33: 2086-2093.
- Wang ZJ, Liang CL, Li GM, Yu CY, Yin M (2006) Neuroprotective effects of arachidonic acid against oxidative stress on rat hippocampal slices. Chem Biol Interact 163: 207-217.
- Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, et al. (2003) Dietary fats and the risk of incident Alzheimer disease. Arch Neurol 60: 194-200.
- Taha AY, Filo E, Ma DW, McIntyre Burnham W (2009) Dose-dependent anticonvulsant effects of linoleic and alpha-linolenic polyunsaturated fatty acids on pentylenetetrazol induced seizures in rats. Epilepsia 50: 72-82.
- Okaichi Y, Ishikura Y, Akimoto K, Kawashima H, Toyoda-Ono Y, et al. (2005) Arachidonic acid improves aged rats' spatial cognition. Physiol Behav 84: 617-623.
- Fukaya T, Gondaira T, Kashiyae Y, Kotani S, Ishikura Y, et al. (2007) Arachidonic acid preserves hippocampal neuron membrane fluidity in senescent rats. Neurobiol Aging 28: 1179-1186.
- Palomba L, Cerioni L, Cantoni O (2009) Arachidonic acid: a key molecule for astrocyte survival to peroxynitrite. Glia 57: 1672-1679.
- Horrobin DF, Manku MS, Hillman H, Iain A, Glen M (1991) Fatty acid levels in the brains of schizophrenics and normal controls. Biol Psychiatry 30: 795-805.
- Soderberg M, Edlund C, Kristensson K, Dallner G (1991) Fatty acid composition of brain phospholipids in aging and in Alzheimer's disease. Lipids 26: 421-425.
- McGahon B, Clements MP, Lynch MA (1997) The ability of aged rats to sustain long-term potentiation is restored when the age-related decrease in membrane arachidonic acid concentration is reversed. Neuroscience 81: 9-16.
- Murray CA, Lynch MA (1998) Evidence that increased hippocampal expression of the cytokine interleukin-1 beta is a common trigger for age- and stress-induced impairments in long-term potentiation. J Neurosci 18: 2974-2981.
- Summers LK, Fielding BA, Bradshaw HA, Ilic V, Beysen C, et al. (2002) Substituting 171 dietary saturated fat with polyunsaturated fat changes abdominal fat distribution and improves insulin sensitivity. Diabetologia 45: 369-377.
- Petersson H, Arnlöv J, Zethelius B, Risérus U (2010) Serum fatty acid composition and insulin resistance are independently associated with liver fat markers in elderly men. Diabetes Res Clin Pract 87: 379-384.
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 15119
- [From(publication date):
August-2012 - Nov 11, 2025] - Breakdown by view type
- HTML page views : 10372
- PDF downloads : 4747