A Case Report on Post-Operative Intussusception, Post Primary Volvulus Derotation and Decompression
Received: 16-Oct-2018 / Accepted Date: 19-Nov-2018 / Published Date: 29-Nov-2018 DOI: 10.4172/2161-069X.1000577
Abstract
Intussusception is process in which a segment of intestine enters into adjoining intestine lumen causing bowel obstruction. Intussusception is unusual in adults, and the diagnosis is commonly overlooked.
In this case report the patient was 40 years old and was admitted to the surgical ward after he had undergone laparotomy for the diagnosis of small bowel obstruction 2ry to primary volvulus .The presentation to emergency room at that time was colicky type of central abdominal pain, 2-3 episodes of vomiting of bilious matter of 3 days and abdominal distention.
The condition was smooth up to the 3rd postoperative day at which time he restarted to complain central abdominal pain associated with abdominal distention. He had also 2 episodes of vomiting of ingested matter.
On Physical Examination
Vital signs are Blood pressure-120/60; Pulse rate-82 beats/min; (Respiratory Rate) RR-24 beats/min; Temperature-36.7°C but on abdominal examination he had previous surgical scar, slightly distended abdomen which was hyper-tympanic to percussion. On per rectum examination, the rectum was empty. Abdominal X-ray showed multiple air fluid level and abdominal ultrasound which was done after a day showed small bowel obstruction 2ry to intussusception. Then after 2 L of ringer lactate was given over 30 min, catheter and nasogastric tube inserted and re-laparotomy done. The intraoperative finding was ileoileal intussusception with 2.5 cm one siteileal imminent perforation at the mid intussucipiens for which reduction and resection of the imminent perforation and ileoileal anastomosis done. This patient had smooth postoperative course and discharged after 7 days of hospital stay. Therefore to have early diagnosis and management of possible risk of intussusception post small bowel volvulus surgery especially as in this particular case, it is extremely important to take this case for the future care of intraoperative manipulations of bowel and to have future studies of similar cases in the area.
Keywords: Adult postoperative Intussusception; Intussusception; Gastrointestinal
Introduction
Intussusception is defined as the telescoping of one a segment of the gastrointestinal tract into an adjacent one [1]. It was reported initially by Barbette of Amsterdam in 1674 [2]. Sir Jonath Hutchinson was the first to successfully operate on intussusception patients in 1871 [3]. Post-operative intussusception is defined as defined as acute intussusception occurring within 30 days of index surgery, is a recognized and well-described, on the other hand, an extremely rare clinical entity [4,5]. Adult intussusception is rare cause of intestinal obstruction [6]. It is usually caused by existing pathology such as tumor and sometimes the cause is idiopathic [7,8]. Preoperative diagnosis of intussusception is infrequent in adult population, secondary to varying presentations [9].
Since clinical presentation is often nonspecific, imaging is a vital role in the preoperative diagnosis of intussusception [10,11]. So physicians often do not suspect the presence of acute intussusception if the condition occurs in early post-operative period [12]. Therefore as in my case postoperative intussusception especially the first operation done for small bowel obstruction is very uncommon cause of immediate post-operative morbidity and the topic discussed is very helpful in the surgical world.
Case Presentation
A 40 years old patient presented to the emergency room with colicky type of central abdominal pain of 3 days. He had also abdominal distention, failure to pass feces and flatus and 2-3 episode of vomiting of bilious matter. For this complaint diagnosed with small bowel obstruction 2ry to volvulus and resuscitated with after 3 L of crystalloid fluid resuscitation, NG tube and catheter inserted and taken to operation room and operate. The intraoperative finding was 360° counter clock wise rotated distended small bowel, around 100 mL of reactive fluid inside general peritoneum, for which derotation and retrograde decompression was done.
He was in smooth post-operative course until 3rd day with stable vital signs after which he restarted to have central colicky type of He was in smooth post-operative course until 3rd day with stable vital signs after which he restarted to have central colicky type of
Physical examination
• General appearance-acutely sick looking
• Blood pressure-120/60, Pulse rate-82, Respiratory rate-24, Temperature-36.7°C
• HEENT-He had pink conjunctiva and non-icteric sclera.
• Chest-He had clear and good, comparable air entry on bilateral lung field.
• Cardiovascular system-S1 and S2 is well heard, there was no murmur or gallop.
• Abdomen-There was clean surgical scar
• Slightly distended abdomen, tympanic to percussion with shifting dullness.
• There was hyperactive bowel sound.
• Per-rectal examination-There was dried stool on examining finger, but no mass or bleeding per rectal examination.
• Genitourinary system-There was no costo-vertebral angle tenderness.
• Musculoskeletal system -There was no deformity or any edema.
• Integumentary system-There was no signs of palmar paler.
• Central nervous system -He was conscious and oriented.
• Assessment-SBO 2ry to Early post-operative adhesion R/O ileus
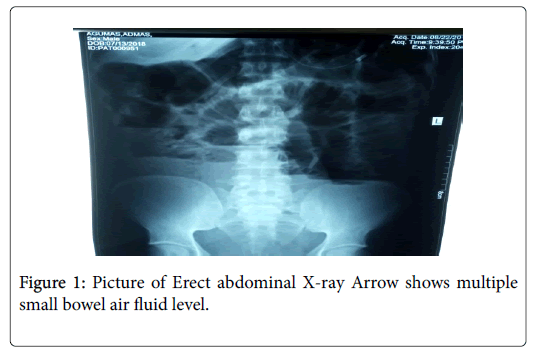
For the above assessment, NG tube inserted and the patient kept NPO and put on maintenance fluid and the following investigations were sent (Figure 1).
Investigation on the 3rd post operative day results
Complete blood count
• White blood cells-6000 cells/mm3,
• Hemoglobin-11 mg/dL,
• Neutrophil-79%
Serum electrolyte
• K+ 3.59 mmol/L,
• Na+ 145.3 mmol/L,
• Cl- 109.8 mmol/L,
• iCa++ 1.06 mmol/L,
• Serum Albumin-4 g/dL,
• Urea - 36.1 mg/dL,
• Creatinine-1.1 mg/dL
Plain abdominal X-ray showed centrally located numerous small bowel loops with multiple air level, paucity of gas in the lower abdomen.
On the 4th post op day the patient still didn't improve and abdominal ultrasound was done. The Abdominal ultrasound result was 4.7 by 8.7 cm whorled bowel and mesentery in the right para-umbilical region, free peritoneal fluid seen and other organs liver, spleen, pancreas were with normal findings (Table 1).
| Date | Time | BP (mmHg) | PR (bpm) | RR (bpm) | T°C | Uop L/D |
|---|---|---|---|---|---|---|
| 20-08-2018 | 8 am | 110/70 | 87 | 24 | 36.4 | 1.3 |
| 12 pm | 120/70 | 84 | 26 | 36.7 | 1.5 | |
| 4 pm | 100/70 | 86 | 28 | 37 | 1.3 | |
| 9 pm | 100/80 | 90 | 26 | 36.8 | 1.5 | |
| 1 am | 110/80 | 87 | 28 | 37 | 1.3 | |
| 21-08-2018 | 8 am | 118/60 | 86 | 26 | 36.7 | adequate |
| 12 pm | 110/70 | 82 | 30 | 37.1 | adequate | |
| 3 pm | 104/60 | 86 | 28 | 36.5 | adequate | |
| 9 pm | 110/70 | 88 | 26 | 37 | adequate | |
| 12 am | 120/70 | 92 | 28 | 36.8 | adequate | |
| 22-08-2018 | 8 am | 120/60 | 86 | 22 | 36.7 | adequate |
| 1 pm | 110/70 | 88 | 24 | 36.8 | adequate | |
| 5 pm | 100/70 | 84 | 28 | 36.9 | adequate | |
| 10 pm | 100/80 | 80 | 24 | 36.6 | adequate | |
| 3 am | 110/60 | 92 | 20 | 36.5 | adequate |
Table 1: Vital sign sheet in the wards for initial post-operative condition.
The Assessment confirmed to be small bowel obstruction 2ry to intussusception. After that the patient was resuscitated with 2 L of Ringer Lactate, Catheter and inserted then taken to the operation theatre and re-laparotomy was done.
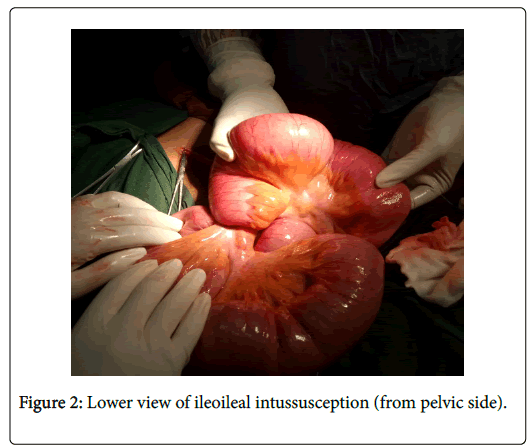
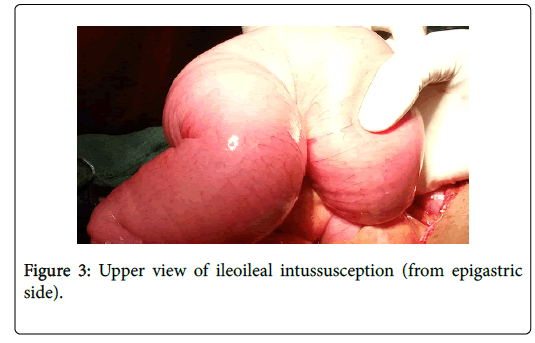
The intraoperative finding was around 150 mL of serous fluid inside the peritoneum, ileoileal intussusception around 80 cm proximal to ileocecal valve with proximal distended bowel, around 2.5 cm imminent perforation at the mesenteric side of intussucipiens due to hugely distended intussuceptum (Figures 2 and 3).
Discussion and Conclusion
What we did intra-operatively was evacuation of peritoneal fluid, reduction of the intussusception, resection of the imminent perforation part of the ileum and end to end ileoileal anastomosis. There was no mass inside the remaining or resected ileum. The patient had smooth post-operative course and was discharged after 7 days of hospital stay.
Acknowledgement
I would like to thank the department of surgery who did a lot in the management of this patient. My kind gratitude goes to the OR nurses and anesthetist above all my assistant Surgeon Dr. Etsub Abebaw for their good did and active participation.
Conflicts of Interest
The authors have no conflicts of interest.
References
- Walker WA, Mieli-Vergani G, Shneider BL, Sherman PM, Kleinman RE, et al. (2004) Pediatric Gastrointestinal Disease: Pathophysiology, Diagnosis, Management, 4th, BC Decker, Ontario: 604.
- Park SB, Ha HK, Kim AY, Lee SS, Kim HJ (2007) The diagnostic role of abdominal CT imaging findings in adult’s intussusception: Focused on the vascular compromise. Eur J Radiol 62: 406-415.
- Barbette P (2017) OuevresChirurgiques at Anatomiques. Geneva: Francois Miege, 1674.
- Zubaidi A, Al-Saif F, Silverman R (2006) Adult intussusceptions: A retrospective review. Dis ColonRectum 49: 1546-1551.
- Kim YW (2016) A case of postoperative spontaneous intussusception after laparoscopic low anterior resection for rectal cancer. Mil Med Res 3:19.
- Eke N, Adotey JM (2000) Postoperative intussusception, causal or casual relationships? Int Surg 85: 303–308.
- Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, et al. (2006) Clinical spectrum and surgical approach of adult intussusceptions: A multicentric study. Int J Colorectal Dis 21: 834–839.
- Chiang JM, Lin YS ( 2008) Tumor spectrum of adult intussusception. J Surg Oncol 98: 444–447.
- Iko BO, Teal JS, Siram SM, Chinwuba CE, Roux VJ, et al. (1984) Computed tomography of adult colonic intussusception: Clinical and experimental studies. AJR Am J Roentgenol 143: 769-772.
- Weiwei J, Weibing T, Qiming G, Xiaoqun Xu (2012) Postoperative intussusception in infants and children: A report of seven cases. J Biomed Res 2: 66–68.
Citation: Minale Y (2018) A Case Report on Post-Operative Intussusception, Post Primary Volvulus Derotation and Decompression . J Gastrointest Dig Syst 8: 577. DOI: 10.4172/2161-069X.1000577
Copyright: © 2018 Minale Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4820
- [From(publication date): 0-2018 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 3938
- PDF downloads: 882