A Mixed Method Study to Assess Women’s Knowledge on Cervical Cancer Screening and Associated Risk Factors in Gakenke District, Rwanda
Received: 06-Oct-2021 / Accepted Date: 20-Oct-2021 / Published Date: 27-Oct-2021
Abstract
Purpose: This study aimed to assess women’s knowledge on cervical cancer screening and associated factors in Gakenke district, Rwanda.
Materials and Methods: We conducted a community-based cross section study in rural areas of Gakenke district, north province of Rwanda from December 2020 to February 2021. Multistage and systematic random sampling techniques were used to select 423 women from households in selected villages and cells of each sector of Gakenke District. Level of knowledge was assessed by calculating the overall scores using SPSS score assessment tool. A bivariate and multivariate analysis was used to establish the factors associated with cervical cancer knowledge. By use of interview guide that was provided to the Key Informants (KIIs), we did thematic interpretation of the perceptions of the Key Informant Interviews (KIIs) towards cervical cancer screening by deductive content analysis to enable deeper understanding of the women’s experience of the disease and uptake of screening services.
Results: Most of the respondents (70.7%) were aged between 20-34 years, and almost all of them 396 (93.6%) had attained at least basic level of education. About 61.6% of the respondents were married, while 20.5% of them were either student or unemployed. Less than half (46.0%) of women demonstrated high level of knowledge towards cervical cancer screening. Regardless, women aged between 30 to 34, were notably less knowledgeable, as compared to those aged 45 years and above [AOR=0.316; 95% CI=0.113-0.885; p=0.028]. Students were 6.6 times more knowledgeable than famers [AOR=6.577; 95% CI=2.501-17.291; p=0.001]. The perceived reasons of lack of knowledge were emerged from three themes, namely lack of awareness, fear about outcome of the results, and the issues of affordability. For the perceived solutions, there were 12 codes, which could be grouped into two groups; which were increasing awareness and vaccination.
Conclusion: The overall level of knowledge towards cervical cancer screening was below average in this study. Age and being a student were the main predictors of good knowledge about cervical cancer cancer. Awareness campaigns, personalized encouragements, affordable and friendly health care with subsidized vaccination, and screening facilities are expected to increase awareness and acceptability and thus reduce burden of the disease.
Keywords: Cervical cancer, Screening, Knowledge, Rwand
Introduction
Globally, about 570, 000 women were diagnosed with cervical cancer in 2018, and about 311,000 of them died in the same period [1]. Consequently, cervical cancer new cases were 77,000 in developed countries and ranked tenth among female malignancies compared to 452,000 in female patients in developing countries where it was ranged second most among all the cancer types [2,3]. Therefore, greater than 85% mortality due to the cancer of cervix occurs in low income countries [4]. Whereas cases of cervical cancer are declining in the developed world, it shows an increasing trend in the developing world [1,5,6]. Ccervical cancer death rate has been estimated to be 18 times higher in low-income and middle-income countries than developed countries and is mainly due to lack of awareness differences [4]. Furthermore, studies in developed countries have shown that women of reproductive age are more aware about cervical cancer screening. For instance, in a retrospective study by Kerrebroeck and Maker in Belgium, the authors reported that over 60% of women were knowledgeable about cervical cancer screening. A study in China also found that over a half (56.4%) of the woman studied were aware of cervical cancer screening [2,7].
Most Sub-Sahara countries are exposed to deferent predisposing factors of cervical cancer such as prolonged HPV infections, HIV infection, lower age at first sex intercourse, having sexual relations with different partners, tobacco smoking, use of family planning methods for longer periods, having many children and malnutrition among others, uptake of screening for cervical cancers still remains low, particularly in rural areas which are the most affected by the disease [8,9]. A study in Kenya revealed that only 6% of women interviewed had gone for cervical cancer screening [10], 16.8% was reported from Zimbabwe [11], 1.6% in Ethiopia and 20% in Congo, with much lower rate of uptake among rural women [12]. Whereas awareness and practices of screening and treatment program have successfully reduced cervical cancer incidences in the developed countries, it remains a major hindrance to cervical cancer diagnosis, treatment and management in many African countries, where the incidence has been estimated at 22.5% of all cancer cases among females [8,9]. Sadly, a big number of females who develop cancer of cervix live in rural areas [9]. Eastern Africa is one of the most seriously affected areas with the incidence of more than 30 cases per 100,000 women reported per year, For instance, in Rwanda, cancer of cervix was classified as the most frequent cancer in females, and the most common cancer among women aged between 15 and 44 years [13,14]. It is ranked the most leading cause of deaths among female cancer with an estimate of 1304 newly diagnosed cases and associated 921 deaths per year [8]. Consequently, the incidence of cervical cancer in Rwanda is estimated at 49 cases per 100,000 females per year, more than the estimated rates in Eastern Africa and worldwide estimated to be 34.5 and 16 new cases per 100,000 females, respectively [15]. The increased mortality rate due to cervical cancer in Rwanda may be attributed to lack of awareness of cancer screening and lack of screening uptake at earlier stage, hence delayed identification of the disease [15]. A study done in Butaro District in Rwanda showed that 97% of cervical cancer patients enrolled at the center from July 2012 to June 2015 had stage II disease or above [16]. Delayed diagnosis was found to be one major concern in cervical cancer prevention and treatment programs. Providentially, the disease can be prevented when detected early through screening strategies..
Even when cervical cancer screening program was introduced in Rwanda in 2010 targeting the entire country, cervical cancer screening rate among asymptomatic remains low at about 13.3%, and it uptake in rural areas is even much lower [17]. Moreover, most studies that have been carried out in Rwanda focused on determination of cervical cancer prevalence among particular groups of women such as those infected or uninfected with HIV/AIDS [14,18], rather than targeting the local population who might be less knowledgeable and are most at risk. There is therefore lack of information about knowledge of cervical cancer screening and the associated factors, particularly in women living in rural areas such as in Gakenke district. It is suspected that social-demographic, economic and health conditions females living may limit their knowledge on cervical cancer screening and hence may influence negative impact on their attitude and uptake of cervical cancer screening. It is with this regard that the current study sought to assess women’s knowledge on cervical cancer screening and associated risk factors in Gakenke District, Rwanda to aid in establishing the magnitude of the problem and guide decision makers in making informed choice for healthcare interventions that can help in the prevention and control of cervical cancer in Rwanda.
Materials and Methods
We conducted a community-based cross-sectional with 423 participants who were randomly selected through multi-stage cluster sampling in Gakenke District from December 2020 to February 2021. The respondents were selected at cell and village level, then to household level. In this mixed research, questionnaire-based interviews (quantitative method) and key Informants Interview guide (qualitative method) that was provided to the KIIs were used to assess the women’s knowledge towards cervical cancer screening, and associated factors in the district. Participants were women aged between 20 and 59 years living in all the 19 sectors of Gakenke District and the health care professionals who could possibly administer and implement cervical cancer screening practices to the women.
Quantitative data
Data collection was done using a structured questionnaire for collecting accurate information. The questionnaire was developed through extensive literature review in English language and was translated into Kinyarwanda the language used by people in Gakenke District. The questionnaire was structured to capture quantitative data about knowledge on cervical cancer screening and associated factors. The first section included questions on the participants’ demographic characteristics such as age, level of education attained, marital status, and area of residence, occupation, number of children and use of methods of contraception. The second section had questions that assessed the respondents’ specific knowledge about cervical cancer, symptoms, screening methods, sources of information, recommended age for cervical cancer vaccination, and the frequency of screening. Some questions required Yes/No or I do not know responses, while others required the participant to mention responses. The questionnaires were administered to 30 women in pilot study for acceptability and consistency of study instrument. Internal consistency was assessed by using Cornbrash’s alpha (α=0.7) and was found to be in acceptable ranges of 0.72-0.80.
Qualitative data
Qualitative data was collected by use of interview guide. It comprised with questions that allowed as capturing leachier and deeper information on cervical cancer screening implementation in all villages and households of data collection area. The participants were interviewed on their current needs to improve their Health-related quality of life. The discussions were recorded by using a voice recorder and the interviews took between 30-40 minutes.
Ethical clearance
During data collection procedure, ethical clearance was obtained from Mount Kenya University Rwanda Institutional Review Committee. The clearance was presented to the Director of Health and Mayor of Gakenke District to get authorization of conducting the study. All local leaders were contacted before conducting data collection.
Data analysis
The collected data were entered and cleaned in Excel version 3.1 and exported to SPSS version 21 for descriptive and logistic regression analysis of quantitative data. Descriptive data analysis was used to describe the knowledge on cervical cancer screening. Frequency tables, graphs and descriptive summaries were used to describe the variables. To obtain a binary outcome of knowledge, the mean knowledge score was determined and women who scored above the mean were considered to be more knowledgeable while those who scored below were considered to have less knowledge. Questions were delivered to study participants in “Yes” or “No” responses. Each correct response was given a score of 1 and a wrong answer was given a score of 0. The maximum calculated score for a respondent is 17 and the minimum is 4. Respondents with score 8 and below were classified as having low level of knowledge, whereas those with 9 score and above were classified as having high level of knowledge.
Binary logistic regression was used to separately assess the associations of the adequacy of knowledge towards cervical cancer screening with socio-demographic characteristics.
Multivariate logistic regression analysis was applied to identify the variables independently associated with knowledge levels of cervical cancer screening. Variables considered in the analysis including: Respondent’s characteristics such as age group, education, marital status, occupation, and monthly income increase knowledge of the cervical cancer screening. Upon fitting these factors using binary logistic regression and by specifying ‘backward conditional’ method with removal at p<0.05, three factors remained in full model of analysis and two in a reduced model. Odds ratio at 95% CI was calculated to show the strength of the association between the outcome and the explanatory variables. All variables which showed statistically significant results with knowledge on cervical cancer screening in bivariate logistic regression were entered to multivariate logistic regression to identify the independent contribution of each explanatory variable and p-value<0.05 was used to decide statistically significant association between the independent and dependent variables.
Qualitative data from key informants were thematically analyzed to complement quantitative data from questions related to study objectives. Interviews were transcribed verbatim and coded. Codes were identified based on data collected during the interviews and were grouped under major themes, which provided the framework for analyzing responses among selected respondents. The quotations indicated the views of selected key informants on knowledge of screening of cervical cancer. They provided additional information to understand more key findings showed throughout the study.
Results
Socio-demographic characteristics of respondents
Out of the 423 females recruited from the 19 sectors, 396 participated in the study, translating to 93.6% response rate. Age group of the respondents ranged from 20 to 49 years, with a mean age of 30.39 (SD=7.99 years). About 271 (68.4%) were married, of which 130 (32.8%) had not given birth, 157 (39.6%) had at least 1-3 children, 105 (26.5%) had 4-6 children, while five (1.0%) had more or equal to seven children. More than a half of respondents 165 (41.7%) had primary school education. The majority of respondents 300 (75.8%) were farmers. Out of respondents, 280 (70.7%) were aged between 20- 34 years, 266 (67.2%) had at least one child (67.2%) while 244 (61.6%) have been ever married. Furthermore, 39 had no level of education i.e., illiterate (9.8%) and 81 (20.5%) were either student or unemployed (Table 1).
| Variable | N (%) |
|---|---|
| Age group in years | |
| 20-24 | 109 (27.5) |
| 25-29 | 101 (25.5) |
| 30-34 | 70 (17.7) |
| 35-39 | 52 (13.1) |
| 40-44 | 35 (8.8) |
| ≥ 45 | 29 (7.3) |
| Education level | |
| Primary | 165 (41.7) |
| Secondary | 185 (46.7) |
| Tertiary | 7 (1.8) |
| Never attended school | 39 (9.8) |
| Employment status | |
| Farmer | 300 (75.8) |
| Employed | 15 (3.8) |
| Unemployed | 81 (20.5) |
| Marital status | |
| Single | 106 (26.8) |
| Married | 271 (68.4) |
| Widowed | 19 (4.8) |
| Number of children | |
| No child | 130 (32.8) |
| 1-3 | 157 (39.6) |
| 4-6 | 105 (26.5) |
| ≥ 7 | 4 (1.0) |
Table 1: Socio-demographic characteristics of respondents.
Women’s knowledge of cervical cancer screening
The majority of the study participants 341 (86.1%) knew the age recommended for girls to be vaccinated against cervical cancer. Likewise, the same majority 341 (86.1%) knew the number of times a female should go for screening of cervical cancer. However, a limited number of respondents 4 (1.0%) knew the test used during cervical cancer screening. Not only 171 (43.2%) of respondents new that the HPV was the causative agent of cervical cancer, and 341 (86.1%) knew age recommended for girls to be vaccinated against cervical cancer, but also 77 (19.4%) knew the age a woman should start screening of cervical cancer. In terms of groups of individuals prone to cervical cancer 333 (84.1%) agreed that all women of childbearing age are prone to cervical cancer while other do not. Furthermore, 329 (83.1%) agreed that sexually active women only are prone to cervical cancer. On sources of cervical cancer, almost all (99.2%) mentioned having many children and early engagement in sexual relationship as main sources of cervical cancer cells. 393 (99.2%) agreed that having many children and 392 (99.0%) starting sexual relations earlier 17 years are main sources of cancer of cervical cells. Furthermore, 388 (98.0%) agreed that having history of STI are sources of cancer of cervical cells. In the context of knowledge of cervical cancer symptoms/signs, 210 (53.0%) agreed that pain during sex is a cervical cancer symptom while other do not. Furthermore, 137 (34.6%) agreed that abnormal vaginal blood loss is a cervical cancer sign. In terms of knowledge of methods to prevent cervical cancer, 351 (88.6%) agreed that immunization is a method to prevent cervical cancer while other did not. Furthermore, 158 (39.9%) agreed that sexual abstinence is a method to prevent cervical cancer. When it comes to places where to get news on cervical cancer, 294 (74.2%) agreed that medical practitioner is the one source of news on cervical cancer while other did not. Furthermore, 143 (36.1%) agreed that newspaper is a good place where to get news on cervical cancer (Table 2).
| Variables | Yes | No |
|---|---|---|
| N (%) | N (%) | |
| HPV is the causative agent of cervical cancer | 171 (43.2) | 225 (56.8) |
| Cervical cancer is curable | 147 (37.1) | 249 (62.9) |
| Know tests used during screening | 4 (1.0) | 392 (99.0) |
| Know age recommended for vaccination | 341 (86.1) | 55 (13.9) |
| Know age to start screening for cervical cancer | 77 (19.4) | 319 (80.6) |
| Know number of times to go for screening of | 341 (86.1) | 55 (13.9) |
| Know groups of individuals at risk | ||
| All women of child bearing age | 333 (84.1) | 63 (15.9) |
| Women with gynecological problems only | 0 (0.0) | 396 (100.0) |
| Pregnant women only | 0 (0.0) | 396 (100.0) |
| Sexually active women only | 329 (83.1) | 67 (16.9) |
| Know predisposing factors | ||
| Many sexual companions | 191 (48.2) | 205 (51.8) |
| Having many children | 393 (99.2) | 3 (0.8) |
| Starting sexual relations earlier than 17 years | 392 (99.0) | 4 (1.0) |
| Being immune-depressed | 376 (94.9) | 20 (5.1) |
| Having history of STI | 388 (98.0) | 8 (2.0) |
| Use of oral contraceptive pills | 0 (0.0) | 396 (100.0) |
| Infection with human papilloma virus | 257 (64.9) | 139 (35.1) |
| Not using condom during sex | 75 (18.9) | 321 (81.1) |
| Parental transmission | 0 (0.0) | 396 (100.0) |
| Know signs and symptoms | ||
| Persistent pelvic pain | 56 (14.1) | 340 (85.9) |
| Abnormal vaginal blood loss | 137 (34.6) | 259 (65.4) |
| Abnormal vaginal discharge | 27 (6.8) | 369 (93.2) |
| Pain during sex | 210 (53.0) | 186 (47.0) |
| Know if cancer of cervix is preventable | 66 (16.7) | 330 (83.3) |
| Know methods of prevention | ||
| Sexual abstinence | 158 (39.9) | 238 (60.1) |
| Being faithful to partner | 0 (0.0) | 396 (100.0) |
| Condom use | 88 (22.2) | 308 (77.8) |
| Immunization | 351 (88.6) | 45 (11.4) |
| Screening | 25 (6.3) | 371 (93.7) |
| Other methods | 15 (3.8) | 381 (96.2) |
| Source of information | ||
| Newspaper | 143 (36.1) | 253 (63.9) |
| TV | 0 (0.0) | 396 (100.0) |
| Friends and relatives | 82 (20.7) | 314 (79.3) |
| Medical practitioner | 294 (74.2) | 102 (25.8) |
Table 2: Distribution of knowledge on cervical cancer screening.
Level of knowledge of cervical cancer screening
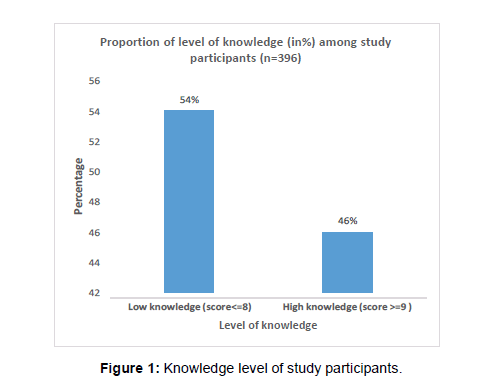
The overall score of knowledge levels about screening of cervical cancer among respondents was determined by using a score of responses. Questions were delivered to study participants in “Yes” or “No” responses. Each correct response was given a score of 1 and a wrong answer was given a score of 0. The maximum calculated score for a respondent is 17 and the minimum was four (4). Respondents with score 8 and below were classified as having low level of knowledge, whereas those with 9 score and above were classified as having high level of knowledge. Out of 396 respondents, 214 (54.0%) attained 8 scores and below and were subsequently had 8 scores and below (214) and subsequently classified as having low level of knowledge, whereas 46.0% of them scored 9 and above and were classified as were classified as having high low level of knowledge. A low level of knowledge was much more observed among respondents age 30-34 that represented 48 (68.6%), while a high level of knowledge was observed among respondents with age group 35-39 years that represented 27 (51.9%), even though observed differences was not statistically significant (p-value=0.673) (Figure 1).
Factors associated with women’s knowledge of cervical cancer screening
We carried out analysis to establish the association between demographic characteristics and level of knowledge cervical cancer screening. A low level of knowledge was observed among full time employees, while high level of knowledge was more provident among part time employees. Moreover, low level of knowledge was observed among respondents who never attended school. Similarly, low level of knowledge prominent among widowed as compared to single. In contrast, low level of knowledge was much more observed among women with 4-6 children than those without (Table 3).
| Variables | Low knowledge | High knowledge | Chi square | P-value | ||
|---|---|---|---|---|---|---|
| n | % | N | % | |||
| Age group | 7.747 | 0.673 | ||||
| 20-24 | 55 | 50.5 | 54 | 49.5 | ||
| 25-29 | 53 | 52.5 | 48 | 47.5 | ||
| 30-34 | 48 | 68.6 | 22 | 31.4 | ||
| 35-39 | 25 | 48.1 | 27 | 51.9 | ||
| 40-44 | 19 | 54.3 | 16 | 45.7 | ||
| ≥ 45 | 14 | 48.3 | 15 | 51.7 | ||
| Occupation | 45.205 | <0.001 | ||||
| Unemployed | 7 | 16.3 | 36 | 83.7 | ||
| Student | 15 | 39.5 | 23 | 60.5 | ||
| Part time employee | 0 | 0 | 7 | 100 | ||
| Full time employee | 4 | 50 | 4 | 50 | ||
| Farmer | 188 | 62.7 | 112 | 37.3 | ||
| Education | 39.909 | <0.001 | ||||
| Low primary | 16 | 57.1 | 12 | 42.9 | ||
| Primary (P4-P6) | 92 | 67.2 | 45 | 32.8 | ||
| Vocational training | 12 | 60 | 8 | 40 | ||
| Secondary (S1-S3) | 48 | 48.5 | 51 | 51.5 | ||
| Secondary (S4-S6) | 19 | 28.8 | 47 | 71.2 | ||
| Diploma (A1) | 0 | 0 | 3 | 100 | ||
| Bachelor’s and above | 0 | 0 | 4 | 100 | ||
| Never attended school | 27 | 69.2 | 12 | 30.8 | ||
| Marital Status | 6.541 | 0.035 | ||||
| Single | 51 | 48.1 | 55 | 51.9 | ||
| Married | 132 | 54.1 | 112 | 45.9 | ||
| Co-habitant | 16 | 59.3 | 11 | 40.7 | ||
| Widowed | 15 | 78.9 | 4 | 21.1 | ||
| Number of children | 10.61 | 0.002 | ||||
| No child | 59 | 45.4 | 71 | 54.6 | ||
| 01-Mar | 85 | 54.1 | 72 | 45.9 | ||
| 04-Jun | 66 | 62.9 | 39 | 37.1 | ||
| ≥ 7 | 4 | 100 | 0 | 0 | ||
Table 3: Association between demographic characteristics and women’s knowledge level of screening of cervical cancer.
Multivariate analysis for significant variables with women’s knowledge levels of cervical cancer screening
Respondents aged 30 to 34 years were roughly 68% less likely to have high knowledge on cervical cancer screening compared to those aged 45 years and above (AOR=0.316; 95%CI=0.113-0.885; p=0.028). High level of knowledge of the cervical cancer screening was 19.8 times more likely among respondents that were unemployed than those who were farmers (AOR=19.765; 95%CI=7.510-52.015; p=0.001). Furthermore, high level of knowledge of the cervical cancer screening was 6.6 times more likely among respondents who were students compared to those who were famers (AOR=6.577; 95%CI=2.501-17.291; p=0.001) (Table 4).
| Variables | AOR | 95% CI | P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Full model | ||||
| Age group | ||||
| 30-34 | 0.129 | 0.03 | 0.555 | 0.006 |
| ≥ 45 | Ref | |||
| Marital status | ||||
| Single | 1.687 | 0.262 | 10.866 | 0.582 |
| Married | 3.712 | 0.784 | 17.57 | 0.098 |
| Widowed | Ref | |||
| Occupation | ||||
| Unemployed | 11.175 | 2.769 | 45.102 | <0.001 |
| Student | 5.384 | 1.471 | 19.711 | <0.011 |
| Farmer | Ref | |||
| Reduced model | ||||
| Age group | ||||
| 30-34 | 0.316 | 0.113 | 0.885 | 0.028 |
| ≥ 45 | Ref | |||
| Occupation | ||||
| Unemployed | 19.765 | 7.51 | 52.015 | <0.001 |
| Student | 6.577 | 2.501 | 17.291 | <0.001 |
| Farmer | Ref | |||
Source: Primary data
Table 4: Multivariate analysis for factors associated with high knowledge.
Qualitative data
Responses from key informants: Results are presented with regard to the interview guide.
Qualitative data was analyzed to provide additional information in support of the quantitative data to aid in deeper understanding women’s knowledge on cervical cancer screening in order to find solutions to help improve on cervical cancer screening uptake.
When asked on whether she has ever heard about screening program for cervical cancer in Rwandan the a KII respondent explained that the Ministry of Health launched the cervical cancer-screening program in 2010;
She said, “It starts by the immunization campaign for cervical cancer as launched by the first lady targeting the females in the reproductive age 15-49, few years back.”-KII-6
When considering overview of interviewees, they did not have any ideas about future prospects for this programme in the context of accessibility to services. One of the interviewees mentioned, “There are no future prospects that are planned for the targeted group to have access to information on cervical cancer screening and treatment for those who already have been diagnosed with cervical cancer”- KII-2.
However, when reference is made to some achievements of the programme, one study participant said, “Observed achievements include among other the fact that students in high school have got information on cervical cancer signs and symptoms”-KII-5
The head of the health centre who participated in the interview highlighted another big achievement, which is sustainable. She said, “Furthermore, other big achievement observed is that the immunization against cervical cancer is part of the young child immunization agenda like others.”-KII-3
The medical doctor as a KIIs stipulated for future prospects to improve attitudes towards cervical cancer screening. “For future interventions, the MoH would utilize peer educators, mHealth interventions, and strategies that will act on multiple constructs from the IBM like education and environmental constraints simultaneously.” Furthermore, he stipulated, “Innovative approaches to cervical cancer screening service delivery, including community-based HPV self-sampling, should demonstrate promising changes to uptake in screening.”-KII-8
Discussion
The level of good knowledge of cervical cancer screening of women participated in the study was 46.0%. These results are in line with the study conducted in Addis Ababa Ethiopia, which showed that about 44.2% of the respondents had good knowledge of cervical cancer screening [19]. Similar findings were also observed in the study done in in Kathmandu, Nepal by Shrestha found that about 42.9% of women had good knowledge about screening of the cancer of cervix [20]. In contradiction to the findings of this study, much lower knowledge on cervical cancer have been reported in Gabon and Tanzania at 13.6% and 19.2%, respectively [21,22]. This could be due to the variation in study settings and study period. In contrast, studies in developed countries have shown that women are more aware about cervical cancer screening.
The findings of this study are also in contrast with the study done in Belgium by Kerrebroeck and Maker reported that over 60% of women were aware about cervical cancer screening [7]. Another study in China showed that 56.4% of the women studied were aware of cervical cancer screening which is higher than the results from this study [2]. The difference observed might be attributed to lack of adequate cervical cancer screening programs in developing countries compared to developed countries. Other reasons could be related to differences in education, poverty and accessibility to health care services. Some of the reasons have been indicated by KIIs in this study. One key informant stated “There are no future prospects that are planned for the targeted group to have access to information on cervical cancer screening and treatment” KII-2. The KIIs also, mentioned lack of capacity as big challenge. They said” there is lack of trained staff, only midwifes at hospital level have been trained on cervical cancer screening and only one nurse is trained at health centre. Community Health care workers are not Trained on Cervical Cancer screening and enough information on cervical cancer is not available at this level, regular cervical cancer prevention program is not accessible to all women in due lack of knowledge” KII-6 of the total respondents, 45.7% had good knowledge about risk factors for cervical cancer, which was lower than the 57.8% found in a Saudi Arabia study that was conducted among reproductive-age women [23]. This difference may be due to cultural and socio-economic differences between these populations.
Respondents in age group 30-34 were roughly 68% less likely to have high knowledge on cervical cancer screening. These findings were in line with the findings from a hospital-based cross-sectional study done in India [24]. These may be because women of childbearing age are more likely to visit health care setting and get more information from health care providers. Women who had a secondary level of education were 4.4 times more knowledgeable about cervical cancer screening compared with those who did not attend formal education. These findings are in line with previous study carried out in Dessie referral hospital and Dessie health center in northeast Ethiopia, which demonstrated that women with a degree were more aware of cervical cancer screening [25]. This may be because women who are educated are expected to have more information on disease prevention measures.
Conclusion
Findings from this study have shown that less than half of the respondents were knowledgeable of cervical cancer screening.Moreover, increase in age and being a student were found to be the main predictors of good knowledge about cervical cancer screening. Awareness campaigns, personalized encouragements, affordable and friendly health care, vaccination, and access to screening facilities are expected to increase awareness and acceptability and thus reduce burden of the disease.
Moreover, educational interventions, especially those utilizing peer or community health educators and use of mobile clinics or mHealth implementation strategies may further increase the level of knowledge of women living in rural areas such as in Gakenke District. Innovative service delivery, including community-based self-sampling, acting on environmental constraints, striving to make services more available, accessible, and appropriate to women, would be most effective.
Policy makers are encouraged to institute campaigns, personalized encouragements, and provide affordable and friendly health care services, along with screening facilities that are expected to increase awareness and acceptability and thus maintain on the improvement that has so far been achieved.
Declaration of Respondents Consent
The authors obtained informed consents from all the respondents. The respondents were made to understand that their names and initials would be anonymous.s.
References
- Bray F, Ferlay J, Soerjomataram I, Isabelle S, Rebecca LS, et al. (2018) Global cancer statistics, GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68: 394-424.
- Zhang S, Xu, H, Zhang L, Qiao Y (2020) Cervical cancer: Epidemiology, risk factors and screening. Chin J Cancer Res 32: 720-728.
- Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin D, et al. (2015) Cancer incidence and mortalité worldwide: Sources, methods and major patterns. Int J Cancer 136: 359-386.
- Prabhu M, Eckert LO (2016) Development of world health organization recommendations for appropriate clinical trial endpoints for next generation human papillomavirus vaccines. PapillomavirusRes 2: 185-189.
- Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, et al. (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: A Systematic analysis. Lancet 378: 1461-1484.
- Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, et al. (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: A Systematic analysis. Lancet 378: 1461-1484.
- Torre LA, Islami F, Siegel RL, Ward EM, Jemal A (2017) Global cancer in women: Burden and trends. Cancer Epidemiol Biomarkers Prev 26: 444-457.
- Kerrebroeck VH, Makar A (2016) Cervical cancer screening in Belgium and over screening of adolescents. Eur J Cancer Prev 25: 142-1097.
- Bruni L, Albero G, Serrano B, Mena M, Gómez D, et al. (2019) Human papillomavirus and related diseases in Rwanda. ICO/IARC information center on HPV and related diseases report 2-58
- Ntekim A (2021) Cervical cancer in sub-Sahara Africa, topics on cervical cancer with an advocacy for prevention. InTech 52-62.
- Sudenga SL, Rositch AF, Otieno WA, Smith J (2013) Knowledge, attitudes, practices and perceived risk of cervical cancer among Kenyan women. Int J Gynecol Cancer 23: 895-899.
- Mutambara J, Mutandwa P, Mahapa M, Chirasha V, Nkiwane S, et al. (2017) Knowledge, attitudes and practices of cervical cancer screening among women who attend traditional churches in Zimbabwe. J Cancer Res Pract 4: 53-58.
- Lim J, Ojo AA (2016) Barriers to utilization of cervical cancer screening in sub-Sahara Africa: A systemic review. Eur J Cancer Care 26: e12444.
- Jemal A, Bray F, Melisa M, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69-90.
- Singh DK, Kathryn A, Donald RH, Robert DB, Qiuhu S, et al. (2009) Human papillomavirus infection and cervical cytology in HIV-infected and HIV-uninfected Rwandan women. J Infect Dis 199: 51-61.
- de Sanjosé S, Serrano B, Castellsagué X, Brotons M, Muñoz J, et al. (2012) HPV and related cancers in the GAVI Countries. WHO/ICO HPV information center report. Vaccine 30: 1-83.
- Park PH, Davey S, Fehr AE, Butonzi J, Shyirambere, et al. (2018) Patient characteristics and early outcomes of cervical cancer patients at Butaro district Hospital Rwanda. J Glob Oncol 4: 28.
- Ruzigana G, Matabele LB, Rulisa S, Martin AN, Ghebre RG (2017) Cervical cancer screening at a tertiary care center in Rwanda. Gynecol Oncol Rep 21: 13-16.
- Makuza JD, Nsanzimana S, Muhimpundu MA, Pace LE, Ntaganira J, et al. (2015) Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. Pan Afr Med J 22: 1-4.
- Getachew S, Getachew E, Gizaw M, Ayele W, Addissie A, et al. (2019) Cervical cancer screening knowledge and barriers among women in Addis Ababa, Ethiopia. PLoS ONE 14: e0216522.
- Shrestha J, Saha R, Tripathi N (2013) Knowledge, attitude and practice regarding cervical cancer screening amongst women visiting tertiary centre in Kathmandu, Nepal. Nepal Med Sci J 2: 85-90.
- Lyimo FS, Beran TN (2012) Demographic knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health 12: 12-22.
- Assoumou SZ, Mabika BM, Mbiguino AN, Mouallif M, Khattabi A, et al. (2015) Awareness and knowledge regarding of cervical cancer, pap smear screening and human papillomavirus infection in Gabonese women. BMC Women’s Health 15: 1186-1290.
- Bansal AB, Pakhare AP, Kapoor N, Mehrotra R, Kokane AM (2015) Knowledge, attitude and practices related to cervical cancer among adult women: A hospital based cross-sectional study. J Nat Sci Biol Med 6: 324.
- Al-Darwish AA, Al-Naim AF, Al-Mulhim KS, Al-Otaibi NK, Morsi MS, et al. (2014) Knowledge about cervical cancer early warning signs and symptoms, risk factors and vaccination among students at a medical school in al-ahsa, Kingdom of Saudi Arabia. Asian Pac J Cancer Prev15: 2529-2532.
Citation: Izuwayo G, Habtu M, Marete O, Mochama M, Rutayisire E, et al. (2021) A Mixed Method Study to Assess Women’s Knowledge on Cervical Cancer Screening and Associated Factors in Gakenke District, Rwanda. J Oncol Res Treat S5: 004.
Copyright: © 2021 Izuwayo G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 3172
- [From(publication date): 0-2021 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 2312
- PDF downloads: 860