A Rare Case of Anti-NMDA Receptor Encephalitis with Ovarian Teratoma in the Setting of VZV Encephalitis
Received: 13-Oct-2021 / Accepted Date: 27-Oct-2021 / Published Date: 03-Nov-2021
Abstract
Anti-N-methyl-D-aspartate receptor encephalitis (NMDA-RE) is rare autoimmune encephalitis, which classically has been associated with ovarian teratoma but rarely with concomitant viral encephalitis. Physicians need to be aware that patients may have NMDAR antibodies present in the CSF even if the serum test is negative. The patients would have never been correctly diagnosed if she had solely been tested for NMDAR antibodies in the serum.
Keywords: Autoimmune disorder; Encephalitis; Neurodegeneration; Ovarian Teratoma
Introduction
Anti-N-methyl-D-aspartate receptor encephalitis (NMDA-RE) is rare autoimmune encephalitis, which classically has been associated with ovarian teratoma but rarely with concomitant viral encephalitis [1]. We present the first reported case of NMDA-RE with a dual trigger of ovarian teratoma and Varicella Zoster Virus (VZV) encephalitis.
Case Presentation
A 33-year-old female with no known past medical history was admitted to an outside hospital (OSH) for rhythmical shaking and stiffening of upper and lower extremities, preceded by unconsciousness and foaming at the mouth for approximately 7 to 8 minutes. Her CT head did not show any potentially explanatory pathology. She was treated for seizures and discharged home.
She later started to have auditory and visual hallucinations. She was taken to the OSH again where an MRI brain was done, following which she was discharged. At home, she continued to have hallucinations progressing to agitation, verbal perseveration, and confusion. She had another seizure lasting 3 to 4 minutes for which she was brought to our hospital by her husband.
The patient was not alert or oriented to the surroundings and she was not following any simple or complex commands. The neurological examination was nonfocal except for her agitated behavior requiring four-point restraints and benzodiazepines. A lumbar puncture was done that showed elevated nucleated cells (31) with lymphocyte predominance (92%). MRI brain was unremarkable.
CSF analysis showed positive varicella zoster virus (VZV) PCR and N-methyl-D-aspartate receptor (NMDAR) antibody titers (1:20), although the serum NMDAR antibody level was negative. CT abdomen/pelvis showed a right ovarian teratoma.
The patient was treated with a 10-day course of acyclovir (10 mg/kg three times daily) for the VZV. For her anti-NMDAR encephalitis, she received a five-day course of intravenous immunoglobulin (IVIG) with a 2 g/kg total dose and high dose steroids, without significant improvement. Her right ovarian teratoma was resected. No evidence of involvement of the left ovary was appreciated on imaging or direct visualization. She was given a second course of IVIg (2 g/kg) during which her mentation improved.
An EEG done on admission was abnormal, showing potential of epileptogenicity in the left and right temporal regions independently, but no seizures were recorded. The repeat EEG done on her 14th hospital day showed frequent spikes in the left mid and posterior temporal regions, but no seizures.
A repeat LP was performed on hospital day 3, which showed a mild lymphocytic pleocytosis (10-78% lymphocytes) and negative VZV PCR. Her CSF NMDA titer had decreased to 1:1. Due to her improved mental status, she was discharged home 2 days later without further immunomodulating therapy. She followed up in the outpatient clinic with minimal residual neurologic deficits, primarily fatigue and mild memory deficits.
Discussion
In many ways, the patient’s presentation fit the characteristic illness script of anti-NMDAR encephalitis. Patients with anti-NMDAR encephalitis are predominantly female and of reproductive age, like the patient, and approximately half of female adults with anti- NMDAR encephalitis are found to have an ovarian teratoma at diagnosis [1]. The patient also presented with seizures and psychiatric manifestations (agitation, hallucinations, perseverative language), a combination not typically seen in a primary psychiatric illness. In addition, it would be very unusual for a disorder like schizophrenia to present at the age of 33 in an individual with no previous history of psychiatric symptoms or substance abuse. However, there have been only three case reports of an individual having anti-NMDAR encephalitis with concomitant detection of varicella zoster virus (VZV) in the CSF.
In 2014, a rare case of VZV brainstem encephalitis was hypothesized to have triggered anti-NMDAR encephalitis in a 76- year-old woman. The patient initially had symptoms corresponding to lesions in the left brainstem affecting multiple cranial nerves (left hypoglossal paresis, dysphonia, left hemihypesthesia). Later, she developed encephalopathy with hallucinations and cognitive distortions, which was attributed to NMDAR immunoreactivity. The first CSF sample taken upon admission had NMDAR antibodies and a positive PCR for VZV, so it is impossible to know which (if either) preceded the other. However, the patient did not have a tumor, and there was no other obvious trigger of the NMDAR antibody production. There have been multiple documented cases of herpes simplex virus triggering anti-NMDAR encephalitis [2], so it is plausible that a similar process could occur with VZV. As well, individuals over the age of 50 years are more prone to VZV reactivation due to age-related immunosenescence [3].
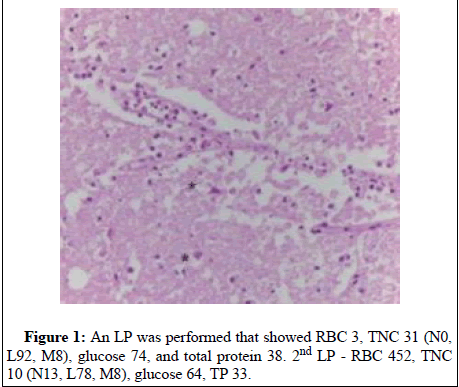
Two other cases were later reported, both of women with anti- NMDAR encephalitis whose CSF had a positive PCR for VZV during the course of their hospitalizations. In both of these cases, the patients had a potential trigger for the anti-NMDAR encephalitis. The first case involved a 29-year-old woman with a teratoma [4]. The other patient, a 50-year-old woman, was found to have a nonteratomatous cervicouterine cancer [5]. Tumors that originate in the endometrium or endocervix-even those that are not teratomas-have been connected to anti-NMDAR encephalitis [6]. Aside from the idea that VZV could directly trigger anti-NMDAR encephalitis, a number of hypotheses have arisen that aim to link the presence of VZV in the CSF to the production of NMDAR antibodies. One idea is that virus shedding or reactivation of VZV could occur as a result of inflammation caused by NMDAR antibodies [6]. It is possible that there is a bidirectional relationship between VZV and NMDAR antibodies, and that there is more than one mechanism for a patient to become ill with both NMDAR antibodies and VZV in the CSF (Figure 1).
In our case as well as two of the three previously described cases, VZV was detected in the CSF prior to the administration of immunosuppressive medications. Nevertheless, it is important to consider that there may be a risk of VZV reactivation with use of immunosuppressive therapies to treat anti-NMDAR encephalitis, and that this could affect the course of the disease. It is unclear how frequently patients with anti- NMDAR encephalitis are even tested for VZV in the CSF. Further research could help determine whether routine testing of CSF for VZV should be recommended for patients with anti-NMDAR encephalitis, or whether patients should receive treatment with acyclovir until both HSV and VZV tests are negative. This would be particularly relevant for patients who were born before 1995 (when the VZV vaccine was first introduced in the United States).
Conclusion
Although anti-NMDAR encephalitis is a rare disease, there needs to be increased awareness of its presenting symptoms and how they differ from those of psychiatric disorders like schizophrenia. One of the reasons that our patient was able to fully recover might have been that her anti-NMDAR encephalitis was identified relatively quickly once she presented at UNM Hospital. Early intervention is of upmost importance, as this disease, if missed, can have grave, persistent consequences for patients. Physicians also need to be aware that patients may have NMDAR antibodies present in the CSF even if the serum test is negative. Our patient would have never been correctly diagnosed if she had solely been tested for NMDAR antibodies in the serum.
References
- Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, et al. (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: An observational cohort study. Lancet Neurol 12: 157-165.
- Nosadini M, Mohammad SS, Corazza F, Ruga EM, Kothur K, et al. (2017) Herpes simplex virus-induced anti-N-methyl-d-aspartate receptor encephalitis: A systematic literature review with analysis of 43 cases. Dev Med Child Neurol 59: 796-805.
- Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, et al. (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82: 1341-1349.
- SolÃs N, Salazar L, Hasbun R (2016) Anti-NMDA Receptor antibody encephalitis with concomitant detection of Varicella zoster virus. J Clin Virol 83: 26-28.
- Prakash PA, Jin J, Matharu K, Garg T, Tsai WC, et al. (2019) Anti-NMDAR encephalitis with concomitant varicella zoster virus detection and nonteratomatous malignancy. Neurol Neuroimmunol Neuroinflamm 6: e537.
- Hara M, Morita A, Kamei S, Yamaguchi M, Homma T, et al. (2011) Anti-N-methyl-D-aspartate receptor encephalitis associated with carcinosarcoma with neuroendocrine differentiation of the uterus. J Neurol 258: 1351-1353.
Citation: Thomas et al. (2021) A Rare Case of Anti-NMDA Receptor Encephalitis with Ovarian Teratoma in the Setting of VZV Encephalitis.J Alzheimers Dis Parkinsonism 11: S7: 029.
Copyright: © 2021 Thomas M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credite
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2556
- [From(publication date): 0-2021 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 1959
- PDF downloads: 597