A Sessile Solitary Osteochondroma in an Unusual Location
Received: 20-Feb-2019 / Accepted Date: 18-Mar-2019 / Published Date: 25-Mar-2019 DOI: 10.4172/2472-016X.1000128
Abstract
Introduction: Osteochondroma usually presents as a solitary or multiple forms, former presents in cases of hereditary multiple exostosis. Solitary Osteochondroma is a benign tumor which occurs generally in children and adolescents. We present a solitary sessile Osteochondroma in an unusual location and size. Case Study: A 14 years old female adolescent noticed a painless swelling in her posterior upper aspect of left leg at the age of 10 years but did not consult any doctor for the same. She occasionally had discomfort in squatting, sitting cross leg and consulted an Orthopaedician after 4 years of occurrence of the swelling, where X-rays were taken. X-rays showed bony outgrowth from the posteromedial aspect of the proximal fibula. CT (Computed Tomography) scan showed irregular lobulated sessile based bony outgrowth from posteromedial aspect of proximal fibula. MRI (Magnetic Resonance Imaging) with contrast showed marrow edema within the tumor. En-block resection of tumor was done then histopathological examination confirmed the diagnosis as a benign exostosis. Postoperatively patient recovered uneventfully. Conclusion: Solitary occurrence of osteochondroma in an unusual location of bone and their early management is a debate, they can be resected once skeletal maturity is attained. It is not necessary that it needs urgent resection until and unless patient approaches with cosmetic deformity, discomfort and pressurising symptoms leading to neurovascular deficits.
Keywords: Osteochondroma; Exostosis; Bone tumor; Proximal fibula
Introduction
Osteochondromas (OCs) being benign tumors of bone is detected predominantly in the metaphysis of long bones with around 35% of the cases arising from the bones about the knee joint. These tumors of bone are mostly asymptomatic but can show symptoms of pain if a fracture occurs at the base of the tumor, nerve impingement syndromes [1]. OCs usually presents as solitary or multiple forms, the former is roughly six times more common than the multiple form, the latter presents generally in cases of hereditary multiple exostosis [2,3]. A solitary Osteochondroma generally occurs in children and adolescents [4,5]. The prevalence of primary bone tumors of fibula is 2.5%. Pedunculated solitary OCs is more common than the sessile OCs. Here we present a sessile solitary Osteochondroma arising from posteromedial aspect of proximal fibula in an adolescent in an unusual location.
Case Report
A 14-year-old female presented with swelling over the posterior and upper aspect of left leg. Initially, it was small in size and painless, which later progressed over a period of four years and grew to attain the present size. She occasionally had discomfort in squatting, sitting cross leg and consulted an Orthopaedician after 4 years of occurrence of the swelling, where X-rays were taken. There was no history of trauma, fever or any other constitutional symptoms. On clinical examination, a large swelling was seen over the posterior aspect of left proximal leg, which was approximately 8 x 6 cm. The swelling was irregular in shape, hard in consistency, non-tender, non-mobile and fixed to the underlying bone. The movement in the knee joint was not restricted, there were no neurovascular deficits in the affected limb.
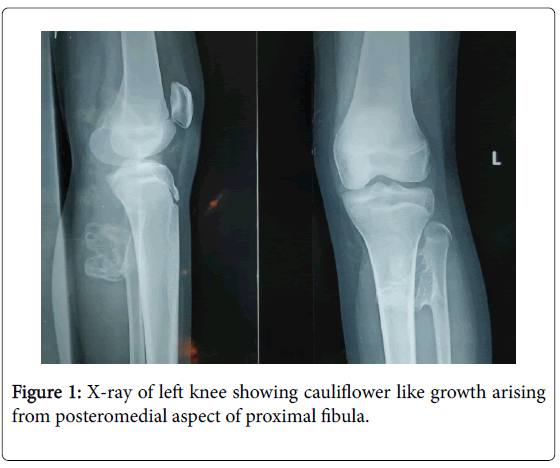
Plain radiographs (AP and lateral view) of left leg with knee were taken, which revealed a large cauliflower like growth arising from posteromedial aspect of proximal fibula (Figure 1).
Before the patient was posted to surgery, Magnetic Resonance Imaging (Figure 2a) and Computed Tomography (Figure 2b) of left leg revealed a solitary sessile exostosis measuring 5 x 2.5 x 4.1 cm arising from posteromedial aspect of left proximal fibula without any contact with neurovascular structures or without compression over them (Figure 2a). MRI showed 4 mm thickness of the surrounding cartilaginous cap with marrow edema. Other laboratory investigations were normal.
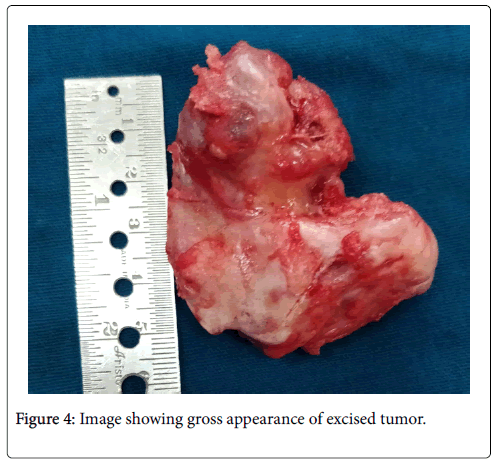
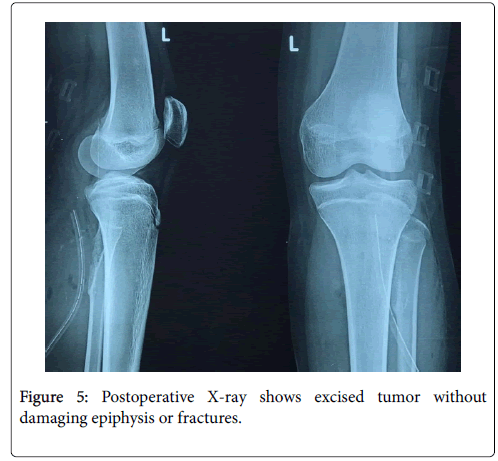
After doing a complete evaluation under combined spinal epidural anesthesia, en-block excision of tumor was performed (Figure 3). Patient was placed in prone position, A tourniquet was applied without exsanguination after venous backflow was achieved by limb elevation for 3-5 minutes. A lazy S-shaped incision extending from lateral aspect of calf region to midline posterior to fibula and tibia, superficial surgical dissection was done, common peroneal nerve was isolated. Muscle fibers were separated and fibula was exposed. En-block excision of tumor was performed (Figure 3a, 3b, 4). Bone wax was applied to the base of tumor after scooping out some part of marrow at the base of exostosis with drain in-situ wound was closed in layers. Intraoperative and postoperative periods were uneventful. A single dose of intravenous antibiotics was given pre-operatively and twice daily for five days, along with analgesics and anti-inflammatory drugs after surgery. Postoperative X-ray was taken which showed clear resection of tumor without any residues and without damaging epiphysis or fractures (Figure 5).
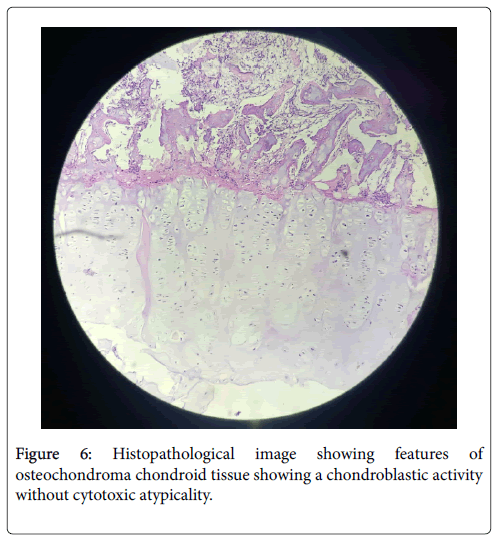
Histopathological examination of excised tumor confirmed the benign nature of osteochondroma chondroid tissue showing a chondroblastic activity without cytotoxic atypicality. Connective tissue composed from outside within a perichondrium with a chondrogenic cap and spongy bony substance (Figure 6) without any evidence of a malignant transformation. The patient’s recovery was uneventful, with no neurological functional impairment. She was subsequently followed up and showed no evidence of recurrence after 1 year of surgery.
Discussion
Sir Astley Cooper was the first person to describe an Osteochondroma (OC) in 1818. By the time an individual attains skeletal maturity the growth of an OC usually ceases, these tumors rarely regress spontaneously throughout the childhood and puberty. In 90% of the cases these tumors are solitary and may be sessile or pedunculated with cartilaginous cap covering the tumor usually of 1-3 mm in thickness composed of hyaline cartilage and without cellular atypia [6]. Tumor favours the meta-epiphyseal region of the long bones like proximal tibia/humerus, distal femur, in other words more commonly around the knee. The cartilaginous cap is the site of growth, which normally diminishes after skeletal maturity. The tumor is presented as a locally benign neoplasm, which favors the metaepiphyseal region of long bones like the distal femur, as well as the proximal tibia or humerus in the extremity [7-9]. The normal anatomical course of nerves and vessels may be distorted leading to vascular compression syndromes, a pseudoaneurysm or peroneal nerve paralysis by a proximal fibular osteochondroma [10-13]. In our case report, in-spite of the huge cauliflower like shape, chronic duration and location of the tumor, still there was no neurovascular compromise. A case report by Manoj Kumar et al. [6] had similar features of presentation of OC arising from the proximal fibula where fibulectomy was performed due to fungative growth of tumor. Life expectancy is not affected by these tumors but in cases of multiple OCs, the risk of malignant transformation should be considered [14].
Thickness of the cartilagenous cap is appropriately measured by imaging studies like Ultrasound, CT and MRI. The thickness of cartilaginous cap exceeding 2 cm signifies possibilities of malignant transformation of an Osteochondroma mostly in adults who have attained complete skeletal maturity [15]. In our study thickness of the cartilaginous cap was 4 mm confirmed by MRI. X-rays showed bony outgrowth from the posteromedial aspect of proximal fibula. CT scan showed irregular lobulated sessile based bony outgrowth from posteromedial aspect of proximal fibula. MRI with contrast showed marrow edema within the tumor. En-block resection of tumor was done and then histopathological examination confirmed the diagnosis as a benign exostosis. Postoperatively patient recovered uneventfully. Histopathological study confirms the diagnosis in almost all cases [16].
Incomplete resection of the sessile type of an OC might lead to recurrence and repeated surgical plan of action. There might also be ensuing disturbed growth and function following resection of entire tumor caused due to massive osseous defect [17].
Conclusion
Solitary occurrence of osteochondroma in an unusual location of bone and their early management is a debate, they can be resected once skeletal maturity is attained. It is not necessary that it needs urgent resection until and unless patient approaches with cosmetic deformity, discomfort and pressurising symptoms leading to neurovascular deficits.
Conflict of Interest
None.
References
- Manoharan A, Suresh SS, Sankaranarayanan L (2013) Proximal Fibular Osteochondroma Producing Common Peroneal Nerve Palsy in a Post-Cesarean Section Patient. Oman Medical Journal 28.
- Mulder JD, Schutte HE, Kroon HM, Taconis WK (1993) Radiologic Atlas of Bone Tumors. (2nd Edtn) Elsevier, Amsterdam.
- Bovee JVMG, Hogendroon PCW (2002) Multiple osteochondromas. In World Health Organization Classificationof tumors. Pathology and Genetics of Tumors of Soft Tissue and Bone. Â IARC Press, Lyon
- Languepin A, Peyrou PL, Houcke M (1980) Exostosant Disease and Solitary Osteogenic Exostoses. Medical and Surgical Encyclopedia, Paris, Elsevier.
- Dahlin DC, Unna KK (1986) General Aspects and Data on 8522 Cases. Bone Tumors. (4th Édtn) Springfield, 227-257.
- Kumar M, Malgonde M, Jain P (2014) Osteochondroma Arising from the Proximal Fibula. J Clin Diagn Res 8: LD01-LD03.
- He XH (1990) Analysis of 1355 cases of tumors and tumor-like lesions in the bone. Zhonghua Zhong Liu Za Zhi 12: 66–68.
- Saglik Y, Altay M, Unal VS, Basarir K, Yildiz Y (2006) Manifestations and management of osteochondromas: a retrospective analysis of 382 patients. Acta Orthop Belg 72: 748–755.
- Baena-Ocampo LDC, Ramirez-Perez E, Linares-Gonzalez LM, Delgado-Chavez R (2009) Epidemiology of bone tumors in Mexico City: retrospective clinicopathologic study of 566 patients at a referral institution. Ann Diagn Pathol 13: 16–21.
- Mnif H, Koubaa M, Zrig M, Zammel N, Abid A (2009) Peroneal nerve palsy resulting from fibular head osteochondroma. Orthopedics 32: 528.
- Cardelia JM, Dormans JP, Drummond DS, Davidson RS, Duhaime C, et al. (1995) Proximal fibular osteochondroma with associated peroneal nerve palsy: a review of six cases. J Pediatr Orthop 15: 574-577.
- Andrikopoulos V, Skourtis G, Papacharalambous G, Antoniou I, Tsolias K, et al. (2003)  Arterial Compromise Caused by Lower Limb osteochondroma. Vasc Endovascular Surg 37: 185-190.
- Holzapfel BM, Seppel G, Wagner R, Kenn W, Meffert R (2011) Popliteal Entrapment Syndrome Caused by Fibular Osteochondroma. Ann Vasc Surg 25: 982-e5.
- Tong K, Liu H, Wang X, Zhong Z, Cao S et al. (2017) Osteochondroma: Review of 431 patients from one medical institution in South China. J Bone Oncol 8: 23–29.
- Bennani L, Amine B, Alaoui H, Hassouni N (2006) Solitary Exostosis of Humerus Associated with a Retractile Capsulitis of the Ipsilateral Shoulder. Revue du Rhumatisme 73, 1206.
- Gogoua RD, Traoré M, Kouamé M, D’Horpock F, Anoumou M (2017) A Recurrent Solitary Exostosis of the Distal End of the Right Radius: A Case Report with a 17-Year Follow-Up. Open J Orthop 7: 140-145.
- Haque MA, Haque ME, Islam MS, Chowdhury MR (2012) A gaint solitary exostosis of the lower ulna in a child. Â Community Based Medical Journal 1: 30-32.
Citation: Ravinath TM, Kulambi V, Shetty S, Prathik R, Vijaykumar K, et al. (2019) A Sessile Solitary Osteochondroma in an Unusual Location. J Orthop Oncol 5: 128. DOI: 10.4172/2472-016X.1000128
Copyright: © 2019 Ravinath TM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4605
- [From(publication date): 0-2019 - Oct 03, 2025]
- Breakdown by view type
- HTML page views: 3742
- PDF downloads: 863