An Audit of the Knowledge and Practice of the Active Management of the Third Stage of Labor in a Resource Constrained Setting
Received: 04-Oct-2017 / Accepted Date: 18-Oct-2017 / Published Date: 25-Oct-2017 DOI: 10.4172/2471-9846.1000200
Abstract
Background: The high incidence of post-partum haemorrage (PPH) in South Africa draws into question the knowledge and practice of HCPs with regard to AMTSL. Hence we carried out this assessment of HCPs knowledge and practice of AMTSL in the Pietermaritzburg Metropolitan Area (PMB).
Aim: To evaluate HCP’s knowledge and practice of AMTSL in the Pietermaritzburg Metropolitan Area and to determine if AMTSL is being correctly implemented.
Method: A cross sectional questionnaire based survey of 280 HCPs involved in maternity services, at a tertiary, regional and district hospital and 3 clinics.
Results: 94% of questionnaires were completed by HCPs, 52.2% being midwives and 47.8% doctors. 71.2% of midwives and 71.1% of the doctors defined AMTSL according to the FIGO/WHO definition, with 93% of midwives and 91.9% of doctors practising AMTSL. Manual removal of the placenta was incorrectly listed as a part of AMTSL by 60.3% of midwives and 50.5% of the doctors. 64% of midwives and 42.3% of doctors incorrectly thought that the routine administration of a uterotonic agent was part of expectant management of the third stage of labour (EMTSL). Early cord clamping was practised by 69% of midwives and 73.8% of doctors, while 92% of midwives and 82.8% of doctors delivered the placenta by controlled cord traction. At caesarean delivery 65% of obstetric doctors and 87% of anaesthetic doctors use oxytocin (as a combination dose of intravenous bolus and infusion).
Conclusion: This study highlights that while there is a deficiency in the knowledge and practice of the HCPs with regard to AMTSL in our setting, the majority do practise AMTSL, with most of the recommended components being implemented.
Keywords: Attitude; HIV/AIDS; Perceived behavioral control; Subjective norm
Introduction
The active management of the third stage of labor (AMTSL) is effective in reducing the incidence of post-partum hemorrhage (PPH), the duration of the third stage of labor and the need for blood transfusion [1]. Failure of the uterus to contract (uterine atony) is the most common cause of primary PPH, occurring in 70-90% of cases and evidence suggests that correct implementation of AMTSL prevents at least 70% of PPH cases [2,3]. In South Africa, obstetric hemorrhage is a major cause of maternal morbidity and mortality and PPH is a major reversible component [4]. The fact that a high number of PPH cases can be prevented if AMTSL is correctly implemented [1] raises the question about the knowledge and practice of Health Care Professionals (HCPs) with respect to AMTSL; and whether the third stage of labor is managed appropriately.
A literature review revealed limited evidence regarding the practice of AMTSL. As far as we are aware, there are no studies regarding the knowledge and practice of AMTSL originating from Southern Africa. Hence we decided to explore the knowledge and practice of HCPs in the Pietermaritzburg (PMB) Metropolitan area of KwaZulu-Natal towards AMTSL.
Methods
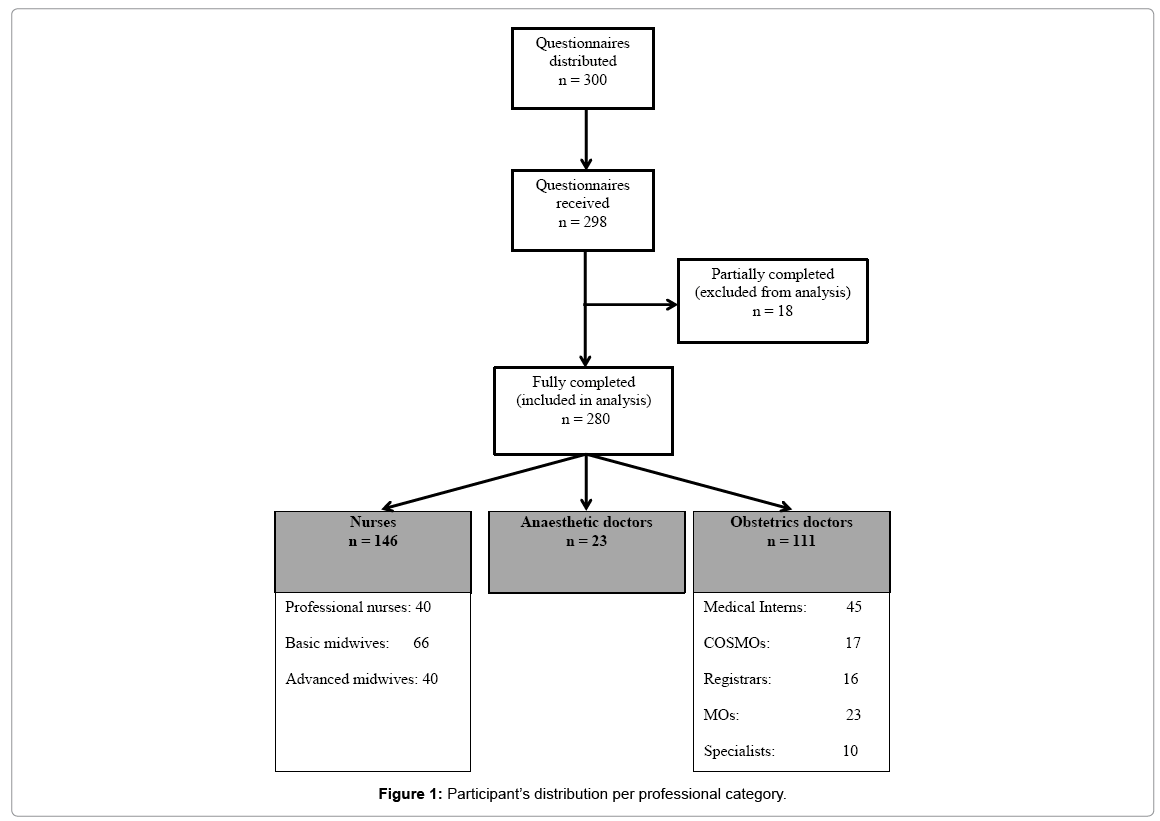
This was a questionnaire based cross sectional survey of HCPs involved in providing peripartum care. It included doctors (medical interns, medical officers, registrars and specialists), anesthetists, midwives and professional nurses in public health facilities consisting of a tertiary, regional, district hospitals and 3 primary health care clinics. The distribution and collection of questionnaire was done as per Figure 1.
The data collection tool comprised a once-off questionnaire in which HCPs were asked to answer questions regarding AMTSL. Participants were recruited at academic meetings and during working hours. The questionnaire took about 10 min to complete and included demographic data with regard to their professional category and number of years of experience in obstetric care and the facility.
Regulatory permission including ethical and institutional permission (BE 029/14) was obtained.
The data was analyzed using SPSS version 21 and frequency tables and bar graphs were used to summarize data. Cross tabulations and Chi-square tests of association were used to investigate association between various variables. An α=0.05 was statistically significant.
Results
Of the 300 distributed questionnaires, 280 were complete and analysed.
Table 1 presents the distribution of the study participants according the level of healthcare facility, years of experience and professional category.
| N | % | |
|---|---|---|
| Proportion of participants per level of health care | ||
| Community Health center | 45 | 16.1 |
| District Hospital | 48 | 17.1 |
| Regional Hospital | 108 | 38.6 |
| Tertiary Hospital | 79 | 28.2 |
| Proportion of participants per level of experience | ||
| 0-3 years | 111 | 39.6 |
| 4-8 years | 80 | 28.6 |
| 9-12 years | 37 | 13.2 |
| >12 years | 52 | 18.6 |
| Proportion of participants per professional category | ||
| Professional nurses | 40 | 14.3 |
| Basic midwives | 66 | 23.6 |
| Advanced midwives | 40 | 14.3 |
| O&G Medical Interns | 45 | 16 |
| O&G COSMOs* | 17 | 6.1 |
| O&G Registrars | 16 | 5.7 |
| O&G MOs | 23 | 8.2 |
| Anesthetics doctors | 23 | 8.2 |
| Obstetricians | 10 | 3.6 |
*Community Service Medical Officer, O&G: Obstetrics and Gynaecology; MOs: Medical Officers
Table 1: Participants per level of care, professional experience and category.
The majority of the participants were basic midwives (23.6%), from the regional hospital (38.6%) and had only 0 to 3 years of experience (39.6%).
37% of professional nurses had 4 to 8 years of experience, while 40.9% of basic midwives and 37.5% of advanced midwives had 4 to 8 years and more than 12 years of experience, respectively. There was a statistically significant association between the number of years of experience and the professional nursing category (2=15.2; p=0.02).
Knowledge of HCPs
83.6% of nurses and 82.9% of doctors defined the third stage of labour (TSL) correctly. The findings pertaining to the knowledge of HCPs with regard to prolonged TSL, the definition and components of AMTSL and EMTSL, eligibility for AMTSL and early vs late cord clamping are summarized in Tables 2 and 3. There was a statistically significant association between doctors’ category and eligibility for AMTSL (χ2=13.6; p=0.03). Also between the nursing category and eligibility for AMTSL (χ2=6.3; p=0.04).
| Nurses | Doctors | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Professional nurses n (%) |
Basic midwives n (%) |
Advanced midwives n (%) |
Total n (%) |
Medical internes n (%) |
Cosmos n (%) |
Registrar n (%) |
MOs n (%) |
Specialist n (%) |
Total n (%) |
|
| How do you define the third stage of labor? | ||||||||||
| Full dilatation to baby’s birth | 2 (5.0) | 5 (7.6) | 3 (7.5) | 10 (6.8) | 4 (8.9) | 3 (17.6) | 0 (0.0) | 3 (13) | 0 (0.0) | 10 (9.0) |
| Full dilatation to placenta expulsion | 2 (5.0) | 4 (6.1) | 6 (15.0) | 12 (8.2) | 3 (6.7) | 4 (23.5) | 2 (12.5) | 0 (0.0) | 0 (0.0) | 9 (8.1) |
| Baby delivery to cord clamping | 2 (5.0) | 0 (0.0) | 0 (0.0) | 2 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Baby delivery to placenta expulsion | 34 (85.0) | 57 (86.4) | 31 (77.5) | 122 (83.6) | 38 (84.4) | 10 (58.8) | 14 (78.5) | 20 (87) | 10 (100) | 92 (82.9) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| How do you define prolonged third stage of labor? | ||||||||||
| >30 min with AMTSL | 23 (57.5) | 35 (53.0) | 14 (35.0) | 72 (49.3) | 30 (66.7) | 6 (35.3) | 8 (50) | 5 (21.8) | 5 (50.0) | 54 (48.6) |
| >60 min with AMTSL | 13 (32.5) | 12 (18.2) | 14 (35.0) | 39 (26.7) | 11 (24.4) | 6 (35.3) | 5 (3.2) | 7 (30.4) | 4 (40.0) | 33 (29.7) |
| >30 min with EMTSL | 3 (7.5) | 10 (15.2) | 2 (5.0) | 15 (10.3) | 2 (4.4) | 4 (23.5) | 2 (12.0) | 6 (26.0) | 1 (10.0) | 15 (13.5) |
| >60 min with EMTSL | 1 (2.5) | 9 (13.6) | 10 (25.0) | 20 (13.7) | 2 (4.4) | 1 (5.9) | 1 (6.2) | 5 (21.8) | 0 (0.0) | 9 (8.1) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What are the components of active management of third stage of labor? | ||||||||||
| Oxytocin, early cord clamping and cutting and controlled cord traction | 16 (40.0) | 15 (22.7) | 11 (27.5) | 42 (28.8) | 12 (26.7) | 3 (17.6) | 7 (43.8) | 6 (26.0) | 4 (40.0) | 32 (28.8) |
| Oxytocin, controlled cord traction and uterine massage | 11 (27.5) | 35 (53.0) | 8 (20.0) | 54 (37.0) | 17 (37.8) | 6 (35.3) | 6 (37.5) | 8 (35.0) | 3 (30.0) | 40 (36.0) |
| Oxytocin, delayed cord clamping/cutting, controlled cord traction, and uterine massage | 13 (32.5) | 16 (24.2) | 21 (52.5) | 50 (34.2) | 16 (35.6) | 8 (47.1) | 3 (18.7) | 9 (39.0) | 3 (30.0) | 39 (35.1) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What are the components of expectant management of third stage of labor? | ||||||||||
| No routine oxytocin, no cord clamping till pulsations stop, placenta delivered by mother’s effort | 19 (47.5) | 42 (63.6) | 17 (42.5) | 78 (53.4) | 28 (62.2) | 10 (58.8) | 7 (43.7) | 12 (52.2) | 7 (70.0) | 64 (57.7) |
| Oxytocin, delayed cord clamping till pulse stops, placenta delivered by mother's effort | 21 (52.5) | 24 (36.4) | 23 (57.5) | 68 (46.6) | 17 (37.8) | 7 (41.2) | 9 (56.3) | 11 (47.8) | 3 (30.0) | 47 (42.3) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What types of patients are eligible for active management of third stage of labor? | ||||||||||
| All patients | 38 (95.0) | 63 (95.5) | 33 (82.5) | 134 (91.8) | 40 (88.9) | 14 (82.4) | 10 (62.5) | 13 (56.5) | 8 (80.0) | 85 (76.6) |
| Only patients at risk of PPH | 2 (5.0) | 3 (4.5) | 7 (17.5) | 12 (8.2) | 5 (11.1) | 3 (17.6) | 6 (37.5) | 10 (43.5) | 2 (20.0) | 26 (23.4) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
Table 2: Definition TSL, prolonged TSL, AMTSL, EMTSL, eligibility for AMTSL.
| Nurses | Doctors | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Professional Nurses n (%) |
Basic midwives n (%) |
Advanced midwives n (%) |
Total n (%) |
Medical internes n (%) |
Cosmos n (%) |
Registrar n (%) |
MOs n (%) |
Specialist n (%) |
Total n (%) |
|||
| How do you define early cord clamping? | ||||||||||||
| Within 20 s | 29 (72.5) | 53 (80.3) | 36 (90.0) | 118 (80.8) | 27 (60.0) | 11 (64.7) | 8 (50) | 15 (65.2) | 4 (40.0) | 65 (58.6) | ||
| Within 30 s | 7 (17.5) | 6 (9.1) | 0 (0.0) | 13 (8.9) | 13 (28.9) | 6 (35.3) | 3 (18.7) | 5 (21.8) | 4 (40.0) | 31 (27.9) | ||
| Within 1 min | 4 (10.0) | 7 (10.6) | 4 (10.0) | 15 (10.3) | 5 (11.1) | 0 (0.0) | 5 (31.3) | 3 (13) | 2 (20.0) | 15 (13.5) | ||
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) | ||
| How do you define late cord clamping? | ||||||||||||
| After 30 s | 12 (30.0) | 14 (21.2) | 8 (20.0) | 34 (23.3) | 9 (20.0) | 4 (23.5) | 3 (18.8) | 6 (26.1) | 3 (30.0) | 25 (22.5) | ||
| After 1 min | 6 (15.0) | 17 (25.8) | 6 (15.0) | 29 (19.9) | 17 (37.8) | 6 (35.3) | 5 (31.2) | 10 (43.5) | 1 (10.0) | 39 (35.1) | ||
| After 3 min | 13 (32.5) | 15 (22.7) | 18 (45.0) | 46 (31.5) | 10 (22.2) | 2 (11.8) | 3 (18.8) | 2 (8.7) | 2 (20.0) | 19 (17.1) | ||
| After cessation of pulsation | 9 (22.5) | 20 (30.3) | 8 (20.0) | 37 (25.3) | 9 (20.0) | 5 (29.4) | 5 (31.2) | 5 (21.7) | 4 (40.0) | 28 (25.2) | ||
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) | ||
| Is bimanual compression of the uterus a component of AMTSL? | ||||||||||||
| Yes | 25 (62.5) | 47 (71.2) | 26 (65.0) | 98 (67.1) | 16 (35.6) | 8 (47.1) | 8 (50) | 12 (52.2) | 2 (20.0) | 46 (41.4) | ||
| No | 15 (37.5) | 19 (28.8) | 14 (35.0) | 48 (32.9) | 29 (64.4) | 9 (52.9) | 8 (50) | 11 (47.8) | 8 (80.0) | 65 (58.6) | ||
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) | ||
| Is manual removal of placenta a component of AMTSL? | ||||||||||||
| Yes | 17 (42.5) | 37 (56.1) | 34 (85.0) | 88 (60.3) | 27 (60.0) | 10 (58.8) | 5 (31.3) | 9 (39.1) | 5 (50.0) | 56 (50.5) | ||
| No | 23 (57.5) | 29 (43.9) | 6 (15.0) | 58 (39.7) | 18 (40.0) | 7 (41.2) | 11 (68.7) | 14 (60.9) | 5 (50.0) | 55 (49.5) | ||
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) | ||
| Is blood transfusion a component of AMTSL? | ||||||||||||
| Yes | 7 (17.5) | 11 (16.7) | 1 (2.5) | 19 (13.0) | 5 (11.1) | 3 (17.6) | 0 (0.0) | 1 (4.3) | 0 (0.0) | 9 (8.1) | ||
| No | 33 (82.5) | 55 (83.3) | 39 (97.5) | 127 (87.0) | 40 (88.9) | 14 (82.4) | 16 (100) | 22 (95.7) | 10 (100) | 102 (91.9) | ||
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) | ||
Table 3: Definition of early and late cord clamping, components of AMTSL.
There was a statistically significant association between the definition of prolonged TSL and nursing category (χ2=16; p=0.01), also between doctors’ category and definition of prolonged TSL (χ2=31.6; p=0.03).
Healthcare professional’s practice
91.8% of doctors and 92.2% of nurses manage the TSL actively and the majority of HCPs practiced early cord clamping (69.8% of midwives and 73.8% of doctors). Other practices with regard to AMTSL, EMTSL, clamping of the cord, placental delivery and the type and timing of administration of prophylactic uterotonic agents are presented in Table 4.
| Nurses | Doctors | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Professional Nurses n (%) |
Basic midwives n (%) |
Advanced midwives n (%) |
Total n (%) |
Medical internes n (%) |
Cosmos n (%) |
Registrar n (%) |
MOs n (%) |
Specialist n (%) |
Total n (%) |
|
| How often do you practice AMTSL? | ||||||||||
| Always | 33 (82.5) | 49 (74.2) | 26 (65.0) | 108 (74.0) | 25 (55.6) | 9 (52.9) | 10 (62.5) | 13 (65.5) | 8 (80.0) | 65 (58.6) |
| Usually | 4 (10.0) | 11 (16.7) | 13 (32.5) | 28 (19.2) | 17 (37.8) | 7 (41.2) | 3 (18,75) | 8 (34.8) | 2 (20.0) | 37 (33.3) |
| Sometimes | 2 (5.0) | 3 (4.5) | 1 (2.5) | 6 (4.1) | 3 (6.7) | 1 (5.9) | 3 (18.75) | 2 (8.7) | 0 (0.0) | 9 (8.1) |
| Rarely | 1 (2.5) | 3 (4.5) | 0 (0.0) | 4 (2.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Never | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| How often do you practice EMTSL? | ||||||||||
| Always | 9 (22.5) | 30 (45.5) | 17 (42.5) | 56 (38.4) | 2 (4.4) | 1 (5.9) | 1 (6.2) | 2 (8.7) | 1 (10.0) | 7 (6.3) |
| Usually | 2 (5.0) | 3 (4.5) | 1 (2.5) | 6 (4.1) | 5 (11.1) | 3 (17.6) | 4 (25) | 2 (8.7) | 0 (0.0) | 14 (12.6) |
| Sometimes | 9 (22.5) | 6 (9.1) | 3 (7.5) | 18 (12.3) | 4 (8.9) | 3 (17.6) | 3 (18.8) | 9 (39.1) | 1 (10.0) | 20 (18.0) |
| Rarely | 9 (22.5) | 11 (16.7) | 6 (15.0) | 26 (17.8) | 18 (40.0) | 4 (23.5) | 1 (6.2) | 5 (21.7) | 2 (20.0) | 30 (27.0) |
| Never | 11 (27.5) | 16 (24.2) | 13 (32.5) | 40 (27.4) | 16 (35.6) | 6 (35.3) | 7 (43.8) | 5 (21.7) | 6 (60.0) | 40 (36.0) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| When do you clamp the cord after the delivery of the baby? | ||||||||||
| Within 20 s | 19 (47.5) | 35 (53.0) | 11 (27.5) | 65 (44.5) | 20 (44.4) | 6 (35.3) | 3 (18.8) | 9 (39.1) | 1 (10.0) | 39 (35.1) |
| 20 to 60 s | 12 (30.0) | 14 (21.2) | 11 (27.5) | 37 (25.3) | 19 (42.2) | 4 (23.5) | 6 (37.5) | 9 (39.1) | 5 (50.0) | 43 (38.7) |
| 1-3 min | 5 (12.5) | 10 (15.2) | 8 (20.0) | 23 (15.8) | 3 (6.7) | 1 (5.9) | 2 (12.5) | 2 (8.7) | 2 (20.0) | 10 (9.0) |
| After pulsations cessation | 4 (10.0) | 7 (10.6) | 10 (25.0) | 21 (14.4) | 3 (6.7) | 5 (29.4) | 5 (31.2) | 3 (13) | 2 (20.0) | 18 (16.2) |
| Others | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (5.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.9) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| How often do you deliver the placenta by controlled cord traction? | ||||||||||
| Always | 36 (90.0) | 53 (80.3) | 33 (82.5) | 122 (83.6) | 27 (60.0) | 14 (82.4) | 11 (68.8) | 11 (47.8) | 6 (60.0) | 69 (62.2) |
| Usually | 2 (5.0) | 10 (15.2) | 1 (2.5) | 13 (8.9) | 18 (40.0) | 3 (17.6) | 4 (25) | 6 (26.1) | 3 (30.0) | 34 (30.6) |
| Sometimes | 1 (2.5) | 3 (4.5) | 6 (15.0) | 10 (6.8) | 0 (0.0) | 0 (0.0) | 1 (6.2) | 5 (21.8) | 1 (10.0) | 7 (6.3) |
| Never | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 0 | 1 (4.3) | 0 (0.0) | 1 (0.9) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What utero-tonic drugs do you use for AMTSL? | ||||||||||
| Oxytocin IV | 12 (30.0) | 12 (18.2) | 14 (35.0) | 38 (26.0) | 13 (28.9) | 11 (64.7) | 2 (12.5) | 8 (34.8) | 3 (30.0) | 37 (33.3) |
| Oxytocin IM | 19 (47.5) | 37 (56.1) | 21 (52.5) | 77 (52.7) | 23 (51.1) | 3 (17.6) | 11 (68.75) | 10 (43.5) | 6 (60.0) | 53 (47.7) |
| Syntometrine IM | 5 (12.5) | 9 (13.6) | 3 (7.5) | 17 (11.6) | 7 (15.6) | 0 (0.0) | 0 (0.0) | 2 (8.7) | 1 (10.0) | 10 (9.0) |
| Misoprostol | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (0.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 0 (0.0) | 1 (0.9) |
| Other or a combination | 3 (7.5) | 8 (12.1) | 2 (5.0) | 13 (8.9) | 2 (4.4) | 3 (17.6) | 3 (18.75) | 2 (8.7) | 0 (0.0) | 10 (9.0) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| When do you administer utero-tonic drugs | ||||||||||
| With delivery of anterior shoulder | 10 (25.0) | 22 (33.3) | 16 (40.0) | 48 (32.9) | 11 (24.4) | 5 (29.4) | 7 (43.8) | 8 (34.8) | 7 (70.0) | 38 (34.2) |
| With delivery of the baby | 4 (10.0) | 4 (6.1) | 8 (20.0) | 16 (11.0) | 3 (6.7) | 1 (5.9) | 2 (12.5) | 1 (4.3) | 2 (20.0) | 9 (8.1) |
| After delivery of the baby before cord clamping | 5 (12.5) | 9 (13.6) | 7 (17.5) | 21 (14.4) | 4 (8.9) | 1 (5.9) | 1 (6,2) | 4 (17.4) | 0 (0.0) | 10 (9.0) |
| After delivery of the baby and cord clamping | 21 (52.5) | 31 (47.0) | 9 (22.5) | 61 (41.8) | 27 (60.0) | 10 (58.8) | 6 (37.5) | 10 (43.5) | 1 (10.0) | 54 (48.6) |
| Total | 40 (100) | 66 (100) | 40 (100) | 146 (100) | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
Table 4: HCPs practice of AMTSL, EMTSL, cord clamping, placental delivery and the use of utertonics.
The association between the frequency of delivering the placenta by controlled cord traction and the nursing category was statistically significant (2=13.8; p=0.03).
Also, a statistically significant association between doctors category and the timing of administration of utero-tonic drugs (χ2=30.3; p=0.04) and a statistically significant association between timing of cord clamping during caesarean section and doctors’ category (χ2=30.8; p=0.03) was found.
The association between the mode of administration of utero-tonic drugs and doctors’ category was statistically significant as well (χ2=22.9; p=0.03).
Doctor’s practice during caesarean delivery
93.6% of doctors deliver the placenta by controlled cord traction and 56.8% of them clamp the cord within 20 s of the delivery of the baby. 65% use oxytocin as a combination dose of an intravenous bolus and infusion. A bolus dose of 2-3IU after delivery of baby and cord clamping and infusion dose of 17-20IU is usually used. 49.5% of obstetric doctors and 60.9% of anaesthetic doctors administered prophylactic uterotonic drugs after delivery of the baby and cord clamping (Table 5).
| Medical internes n (%) |
Cosmos n (%) |
Registrars n (%) |
MOs n (%) |
Specialists n (%) |
Total n (%) |
|
|---|---|---|---|---|---|---|
| Which methods do you deliver the placenta during caesarean section? | ||||||
| Controlled Cord Traction | 39 (88.9) | 17 (100) | 16 (100) | 22 (95.7) | 9 (90.0) | 103 (93.6) |
| Manual Removal | 5 (11.1) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 1 (10.0) | 7 (6.4) |
| Total* | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 110 (100) |
| When do you clamp the cord during caesarean section? | ||||||
| Within 20 s | 28 (62.2) | 14 (82.4) | 5 (31.2) | 12 (52.2) | 4 (40.0) | 63 (56.8) |
| 20 to 60 s | 14 (31.1) | 3 (17.6) | 8 (50) | 6 (26.1) | 5 (50.0) | 36 (32.4) |
| 1-3 min | 0 (0.0) | 0 (0.0) | 00 (0.0) | 2 (8.7) | 1 (10.0) | 3 (2.7) |
| After pulsations cessation | 3 (6.7) | 0 (0.0) | 3 (18.8) | 3 (13) | 0 (0.0) | 9 (8.1) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| When do you administer prophylactic uterotonic drugs during caesarean section? | ||||||
| With delivery of anterior shoulder | 7 (15.6) | 4 (23.5) | 3 (18.8) | 6 (26.1) | 4 (40.0) | 24 (21.6) |
| With delivery of the baby | 7 (15.6) | 3 (17.6) | 2 (12.5) | 5 (21.8) | 4 (40.0) | 21 (18.9) |
| After delivery of the baby but before cord clamping | 5 (11.1) | 1 (5.9) | 2 (12.5) | 3 (13) | 0 (0.0) | 11 (9.9) |
| After delivery of the baby and cord clamping | 26 (57.8) | 9 (52.9) | 9 (56.2) | 9 (39.1) | 2 (20.0) | 55 (49.5) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| Which uterotonic drugs do you use during caesarean section? | ||||||
| Oxytocin IV | 41 (91.1) | 17 (100) | 15 (93.8) | 16 (69.6) | 9 (90.0) | 98 (88.3) |
| Syntometrine IM | 3 (6.7) | 0 (0.0) | 0 (0.0) | 2 (8.7) | 1 (10.0) | 6 (5.4) |
| Ergometrine | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 0 (0.0) | 1 (0.9) |
| Misoprostol | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 0 (0.0) | 1 (0.9) |
| Other or a combination | 1 (2.2) | 0 (0.0) | 1 (6.2) | 3 (13) | 0 (0.0) | 5 (4.5) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What mode of administration do you use for oxytocin during caesarean section? | ||||||
| Bolus | 11 (24.4) | 1 (5.9) | 0 (0.0) | 2 (8.7) | 2 (20.0) | 16 (14.4) |
| Infusion | 15 (33.3) | 1 (5.9) | 1 (6.2) | 4 (17.4) | 1 (10.0) | 22 (19.8) |
| Combination | 19 (42.2) | 15 88.2) | 15 (93.8) | 17 (73.9) | 7 (70.0) | 73 (65.8) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What bolus dose of oxytocin do you administer during caesarean section? | ||||||
| 2-3 IU | 25 (55.6) | 11 (64.7) | 10 (62.5) | 9 (39.1) | 3 (30.0) | 58 (52.3) |
| 5-8 IU | 0 (0.0) | 2 (11.8) | 4 (25) | 5 (21.8) | 4 (40.0) | 15 (13.5) |
| 10 IU | 5 (11.1) | 2 (11.8) | 0 (0.0) | 4 (17.4) | 1 (10.0) | 12 (10.8) |
| 20 IU | 2 (4.4) | 0 (0.0) | 0 (0.0) | 1 (4.3) | 0 (0.0) | 3 (2.7) |
| Not applicable | 13 (28.9) | 2 (11.8) | 2 (12.5) | 4 (17.4) | 2 (20.0) | 23 (20.7) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| What infusion dose of oxytocin do you administer during caesarean section? | ||||||
| 8-12 IU | 3 (6.7) | 3 (17.6) | 0 (0.0) | 3 (13) | 1 (10.0) | 10 (9.0) |
| 17-20 IU | 32 (71.1) | 13 (76.5) | 15 (93.8) | 17 (74) | 7 (70.0) | 84 (75.7) |
| Not applicable | 10 (22.2) | 1 (5.9) | 1 (6.2) | 3 (13) | 2 (20.0) | 17 (15.3) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
| Do you use a secondary Intravenous administration giving set for oxytocin? | ||||||
| Yes | 15 (33.3) | 3 (17.6) | 6 (37.5) | 9 (39.1) | 5 (50.0) | 38 (34.2) |
| No | 17 (37.8) | 11 (64.7) | 7 (43.8) | 10 (43.5) | 3 (30.0) | 48 (43.2) |
| Sometimes | 1 (2.2) | 2 (11.8) | 2 (12.5) | 2 (8.7) | 0 (0.0) | 7 (6.3) |
| Not applicable | 12 (26.7) | 1 (5.9) | 1 (6.2) | 2 (8.7) | 2 (20.0) | 18 (16.2) |
| Total | 45 (100) | 17 (100) | 16 (100) | 23 (100) | 10 (100) | 111 (100) |
Table 5: Obstetric doctors practice at caesarean section.
23 doctors working in the anaesthetics department were enrolled in the study. The number of years of experience varied widely, with 60.9% having 0 to 3 years of experience, 13% had 4 to 8 years of experience, 13% had 9 to 12 years of experience and 13% had more than 12 years of experience.
87% reported administering a combination of a bolus and an infusion dose of utero-tonic drugs. Only13% reported using a bolus dose alone. Of those doctors who combine a bolus and an infusion dose of oxytocin, 45% always used a secondary IV line for the administration of oxytocin, while 35% never used a secondary IV line. The remaining 20% use a secondary line sometimes. Table 6 gives details of the oxytocin dose administered by the anaesthetics doctors.
| N | % | |
|---|---|---|
| What bolus dose of oxytocin do you administer during caesarean sections? | ||
| Bolus of 2-2.5 IU | 22 | 95.7 |
| Bolus of 5 IU | 1 | 4.3 |
| Total | 23 | 100 |
| What infusion dose of oxytocin do you administer during caesarean sections? | ||
| Infusion of 8 IU | 1 | 4.3 |
| Infusion of 17-20 IU | 19 | 82.6 |
| Infusion of 40 IU | 1 | 4.3 |
| Not indicated | 2 | 8.7 |
| Total | 23 | 100 |
| When do you administer oxytocin during caesarean section? | ||
| With delivery of anterior shoulder | 1 | 4.3 |
| After delivery of the baby but before cord clamping | 8 | 34.8 |
| After delivery of the baby and cord clamping | 14 | 60.9 |
| Total | 23 | 100 |
Table 6: Administration of prophylactic oxytocin by anaesthetic doctors during caesarean section.
Discussion
The international federation of gynaecologists and obstetricians (FIGO), the international confederation of midwives (ICM) and world health organization (WHO) recommend the routine use of AMTSL for all vaginal births in health facilities [5,6]. Our study revealed that the majority of HCPs practice AMTSL and believe that the intervention is indicated for all patients, not only those who are at risk of having PPH. These findings are similar to that of other studies: Farrar et al. [7] in 2010 found that 93% of obstetricians and 73% of midwives report “always or usually” using AMTSL, while Bombastic et al. [8] in 2010 found that 78% of obstetricians “always or usually” use AMTSL.
With regard to HCP’s knowledge
Our study highlighted a deficiency in the basic knowledge of the majority of HCPs with regard to TSL, AMTSL and EMTSL. Approximately one sixth of doctors and midwives incorrectly defined the TSL. Furthermore interventions such as bimanual compression of the uterus and manual removal of the placenta were incorrectly considered as a part of AMTSL. These findings are similar to a Nigerian survey of HCP’s knowledge with regard to AMTSL, which showed bimanual compression of the uterus (37.7%) and manual removal of the placenta (24.7%) to be incorrectly considered as components of AMTSL [9].
The definition and the components of AMTSL are varied despite its well documented beneficial effects, this was evident in the participant’s responses, where most HCPs followed the FIGO/ICM protocol: (administration of prophylactic uterotonics within 1 min after the baby’s birth, controlled cord traction for placental delivery and uterine massage after placental delivery - where no comment on cord clamping is advised) [5] and WHO protocol: (where late cord clamping at least 1-3 min is added to the recommended components by ICM/FIGO to accommodate the growing evidence suggesting beneficial effects of delayed cord clamping to the baby) [6]. A small proportion of HCPs followed the Cochrane/NICE guidelines which suggests early cord clamping [1,10]. The evidence also suggests no difference between early and late cord clamping on maternal outcomes [11]. With regard to the definition of early and late cord clamping: WHO defined early cord clamping as clamping within 1 min of delivery, while late cord clamping is defined as clamping the cord after 1 to 3 min. Our study showed that most of the midwives and doctors were able to define early cord clamping (58.6% for doctors and 80.8% of midwives define early cord clamping as clamping the cord within 20 s of delivery), but the definition of late cord clamping varied widely. These findings are similar to that of Bombastic et al. [8] but differ from that of Farrar et al. [7] who showed that most midwives and obstetricians define early cord clamping as occurring within 10 s and late cord clamping after cessation of cord pulsation.
When assessing the practice of AMTSL
Our study found that the majority of HCPs always or usually manage the TSL actively; this is in keeping with other studies that assessed the practice of AMTSL [7,8].
This study showed that uterotonic agents are utilised by a large proportion of HCPs, including 46.6% of midwives and 42.3% of doctors, who incorrectly thought that the routine administration of uterotonic agent is a part of EMTSL.
Oxytocin was the uterotonic agent of choice for most HCPs and is mainly given after the delivery of the baby and cord clamping, this was in keeping with the findings of Bombastic et al. [8] and differ from Farrar et al. [7] who found in their study in 2010 that IM syntometrine was the most commonly administered uterotonic agent after the delivery of anterior shoulder. However, the preferred route of administration in our study was the IM route, as compared to the IV route in the study of Bombastic et al. [8]
It is well known that administration of the uterotonics is the most important component of AMTSL, it reduces PPH by about 50% if used alone [12]. It is possible that the shortcoming of our HCPs practice of AMTSL is either the dose (which was not assessed in our study), or the timing, or the route of oxytocin administration (recent data favours early versus slow IV) [13]. In South African health facilities oxytocin is the recommended uterotonic agent for the prevention of PPH (10 IU, IMI) after delivery of the baby [14,15]. Most low risk pregnancies are delivered in clinics and many labouring women may not have intravenous lines. This may contribute to the findings that most nurses used IMI oxytocin. Furthermore medical staff shortage and presence of only one attendant during the delivery might contribute to the late oxytocin administration (after the delivery of the baby and cord clamping).
Our study showed that the majority of HCPs practice early cord clamping (within 1 min), the majority of midwives do so within 20 s, while the majority of doctors do so between 20 to 60 s. These finding are similar to those of Farrar et al. [7] and Bombastic et al. [8].
Our study highlighted a discrepancy between the knowledge and practice of AMTSL by our HCPs, where most of them followed the WHO definition of AMTSL (where delayed cord clamping is advised unless immediate resuscitation is needed), but they practice early cord clamping (as recommended by Cochrane/NICE guidelines). While this might not be beneficial to the new born, clamping the cord early theoretically reduces maternal blood loss and this may be the reason for our HCPs practice of early clamping.
The majority of our HCPs deliver the placenta by controlled cord traction, which is similar to the finding of Farrar et al. [7] but contrary to the findings of Bombastic et al. [8].
Recent evidence suggests little effect of controlled cord traction on the incidence of sever PPH, need for therapeutic uterotonics or blood transfusion [16], postpartum blood loss and duration of TSL when utertonic agents are used [17].
At caesarean delivery (CD)
Our study found that 56.8% of doctors clamp the cord within 20 s of delivery and 98.6% deliver the placenta by controlled cord traction. Most doctors assess the placental bed and the uterine cavity for bleeding after placental delivery. All doctors ensure haemodynamic stability in the operating theatre and recovery room; they check for vaginal bleeding and uterine contractility intra- or post operatively. All of the above mentioned steps are critical to prevent PPH at or post CD.
While the uterotonic agents at the time of CD are predominantly administered by the anaesthetist, we found that the surgeon’s knowledge regarding the type, route and dosage of drug administration are actually similar to what the anaesthetists practise. These findings were similar to Farrar et al. [7] in 2010 who showed that the obstetricians and anaesthetists use of oxytocin at CD was similar.
Oxytocin is the most commonly used prophylactic uterotonic agent at CD by the majority of doctors and is mainly used as combination dose (65.8% obstetric doctors and 87% of anaesthetic doctors). The bolus dose used was mainly 2 to 3 international units (IU) by surgeons and 2 to 2.5 IU by the anaesthetists, while the combination dose was mainly 17 to 20 IU by both. It is usual practice to administer the prophylactic uterotonic drug after delivery of the baby and cord clamping.
Our study found that the bolus oxytocin dose used during CD by the majority of the doctors is half the minimum dose recommended by NICE [18] and practised across most of Europe and Australia [19] and by most obstetricians and anaesthists in UK [20]; where 5-10 IU oxytocin as a slow IV bolus is used. This use of smaller oxytocin bolus dose by our HCPs might be because of the fear of the haemodynamic side effects of oxytocin, such as hypotension, tachycardia, flushing and chest pain. The practice of using a smaller oxytocin bolus dose might be a possible reason for increased bleeding during CD as a result of poor uterine tone, but there is no documented evidence of this. It must however be noted, that the systematic review of oxytocin dosing at caesarean delivery supports slow boluses of 0.3 to 1 IU at elective CD and 3 IU at emergency CD; and both followed by a 5 to 10 IU/h oxytocin infusion, to reduce the risk of PPH while minimizing the adverse effects of oxytocin [21]. Our study also showed that most of HCPs do not use separate intravenous lines for oxytocin infusion at the time of CD.
A possible area that might be deficient and may explain the reason for high incidence of PPH at CD is the dose and timing of oxytocin prophylaxis, (low prophylactic oxytocic drug, late administration of oxytocin, no separate line for oxytocin infusion) and the fact that intravenous infusions are often stopped during transfer of patients out from the operating theatre.
Conclusion
Although there is a deficiency in the knowledge of the HCPs in study sites with regard to AMTSL, the intervention is implemented, with most of the recommended steps used by the majority of HCPs. The most important component of the intervention (administration of uterotonics) is used by a large proportion of HCPs. The only deficient area in knowledge might be the dose or timing (late) of uterotonic administration both after vaginal delivery and in the operating theatre during CD.
References
- Prendiville WJP, Elbourne D, McDonald SJ (2000) Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev 3:CD000007.
- Anderson J, Etches D, Smith D (2001) Postpartum haemorrhage. In: Damos JR, Eisinger SH (eds.) Advanced life support in obstetrics (ALSO) provider course manual. Leawood, Kansas: Am Acad Fam Phys, pp: 1-15.
- Rajaram P, Agarwal A,Swain S (1995) Determinants of maternal mortality: A hospital based study from South India. Indian J Matern Child Health 6: 7-10.
- Saving Mothers Report 2008-2010, the 5th triennial report of the national committee on confidential enquiries into maternal deaths in South Africa (2012) NDOH.
- Management of the third stage of labour to prevent post-partum haemorrhage (joint statement) (2003) The Hague and London: International confederation of midwives and international federation of gynaecology and obstetrics.
- Managing complications of pregnancy and childbirth: A guide for midwives and doctors (2003) Geneva: World Health Organization, United Nations Population Fund, United Nations Children’s Fund and The World Bank.
- Farrar D, Tuffnell D, Airey R, Duley L (2010) Care during the third stage of labour: A postal survey of UK midwives and obstetricians. BMC Preg Childbirth 10: 23.
- Bimbashi A, Ndoni E, Dokle A, Duley L (2010) Care during the third stage of labour: Obstetricians views and practice in an Albanian maternity hospital. BMC Pregn Childbirth 10: 4.
- Oladapo OT, Fawole AO, Loto OM, Adegbola O, Akinola OI, et al. (2009) Active management of third stage of labour: A survey of providers’ knowledge in southwest Nigeria. Arch Gynecol Obstet 280: 945-952
- National collaborating centre for women's and children's health: Intrapartum care: Care of healthy women and their babies during childbirth (2007) London: RCOG Press, pp: 32-33.
- McDonald SJ, Middleton P, Dowswell T, Morris PS (2013) Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database of Systematic Rev.
- Cotter A, Ness A, Tolosa J (2013) Prophylactic oxytocin for the third stage of labour. Cochrane Database of Syst Rev 10: CD001808.
- Emire OO, Berna D, Sezin EA, Sibel A, Salim E, et al. (2014) Prospective randomized trial of oxytocin administration for active management of the third stage of labor. Int J Gynaecol Obstet 127: 175-179.
- Guidelines for maternity care in South Africa: A manual for clinics, community health centers and district hospitals (2007) Community health services.
- Matsitse TB, Helberg E, Meyer JC, Godman B, et al. (2017) Compliance with the primary health care treatment guidelines and the essential medicines list in the management of sexually transmitted infections in correctional centres in South Africa: Findings and implications. Expert Rev Anti Infect Ther 15: 963-972.
- Moore JE, Uka S, Vogel JP, Timmings C, Rashid S, et al. (2016) Navigating barriers: Two year follow up on recommendations to improve the use of maternal health guidelines in Kosovo. BMC Public Health 16: 987.
- Yongming DU, Man YE, Feiyun Z (2014) Active management of the third stage of labor with and without controlled cord traction: A systematic review and meta-analysis of randomized controlled trials. Acta Obstet Gynecol Scand 93: 626-633.
- National collaborating centre for women's and children's health (2012) Caesarean section clinical guideline. RCOG Press.
- Mockler JC, Murphy DJ, Wallace EM (2010) An Australian and New Zealand survey of practice of the use of oxytocin at elective caesarean section. Aust N Z J Obstet Gynaecol 50: 30-35.
- Wedisinghe L, Macleod M, Murphy DJ (2008) Use of oxytocin to prevent haemorrhage at caesarean section - A survey of practice in the United Kingdom. Eur J Obstet Gynecol Reprod Biol 137: 27-30.
- Stephens LC, Bruessel T (2012) Systematic review of oxytocin dosing at caesarean section. Anaesth Intensive Care 40: 247-252.
Citation: Daef G, Naidoo TD, Moodley J (2017) An Audit of the Knowledge and Practice of the Active Management of the Third Stage of Labor in a Resource Constrained Setting. J Comm Pub Health Nursing 3:200. DOI: 10.4172/2471-9846.1000200
Copyright: © 2017 Daef G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7311
- [From(publication date): 0-2017 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 6279
- PDF downloads: 1032