Blood Exposure Accidents among Health Care Personnel at the Ngaoundere Regional Hospital in Northern Cameroon: Knowledge, Practical Attitudes, and Means of Prevention
Received: 03-Jun-2022 / Manuscript No. omha-22-66094 / Editor assigned: 06-Jun-2022 / PreQC No. omha-22-66094 (PQ) / Reviewed: 20-Jun-2022 / QC No. omha-22-66094 / Revised: 23-Jun-2022 / Manuscript No. omha-22-66094 (R) / Published Date: 30-Jun-2022
Abstract
Introduction: Blood exposure accidents (BEA) are a major public health problem, especially in developing countries such as Cameroon. Evaluating the knowledge and practices among healthcare workers (HCWs) of the Ngaoundere Regional Hospital (NRH), in relation to BEA, was a logical step towards addressing this concern in Cameroon.
Design: From 1 March to 30 April 2021, a descriptive cross-sectional study was conducted at the NRH in the Adamawa region of Cameroon. The study population consisted of the HCWs of the NRH. A total, 218 health care personnel were contacted to participate in the study and 172 (78.89%) HCWs agreed. Data were collected using an anonymous, self-administered questionnaire.
Results: A total of 172 HCWs were surveyed and the predominant gender was female (54.7%), the average age was 35.55±7.46 years, and the average longevity was 9.14±6.78 years. Approximately 62.80% of the respondents claimed to have had at least one BEA. The most common BEA was needle stick injury (87.5%), followed by infected blood splashed into the mouth and/or eyes (52.0%) and contact with a wound containing infected blood (48.7%).
Conclusions: This study revealed a poor knowledge of interventions after BEA, demonstrated in the practices of HCWs of the NRH, especially according to their professional category, with medical staff having a better knowledge of BEA than paramedical staff.
Keywords
Blood exposure accident; Health care workers; Risk factor; Ngaounde Regional Hospital
Introduction
The infection risk due to blood exposure accidents (BEA) among health care personnel or health care workers (HCWs) is a major public health problem, especially in developing countries with limited resources [1]. A BEA is defined as accidental contact with blood or a biological liquid contaminated by bacteria, viruses, parasites and fungi, followed a skin injury (sting, cut, scratch, bite) [1].
With the onset of the Human Immunodeficiency Virus (HIV), hepatitis C virus (HCV) and more recently, the epidemics of severe acute respiratory syndrome (SARS), the pandemics of H1N1 influenza, and Ebola virus infections, exposed HCWs are at high risk of infection, especially under difficult working conditions. This is the case reported by studies in the Democratic Republic of Congo and Liberia, showing exposure to Ebola, and reports from Germany, Italy, India, China, Brazil, South Africa, Nigeria and Cameroon, where a number of HCWs were exposed while working on patients with the SARS-CoV-2 [2,3].
Blood exposure accidents are now known to be the most frequent occupational accidents in the hospital environment, and the possibility of infection with HIV, HCV, or HBV poses a serious risk, especially in non-immune individuals, further endangering the lives of HCWs. A thorough evaluation of the frequency of BEA in the medical or paramedical population is made difficult by the under-reporting of these work-related accidents. The World Health Organization (WHO) estimates that more than two million needle-stick injuries are sustained by HCWs annually [4].
In Cameroon, a study conducted at the Bertoua Regional Hospital in 2010 revealed a BEA prevalence of 71.6% with needle recapping during care being considered as a primary risk factor (61.1%) [5], in 2015, a study conducted at the Yaoundé Central Hospital reported a 39.6% BEA prevalence in the HCWs over a 12-month period [6]. In 68.4% of these BEA cases, the serological status (HBV and HCV) of the source patient was unknown, and up to 73.7% of the BEA victims did not declare injury [6].
Knowledge of the epidemiological data on BEA allows health personnel to be aware of the circumstances of these accidents in order to put in place ad hoc prevention measures. The present study was conducted with the aim of improving compliance with standard precautions and protocols for the prevention of BEA and other biological fluid, by assessing the knowledge, attitudes and practices of HCWs at the Ngaoundere Regional Hospital (NRH) in relation to BEA, and to provide recommendations on intervention and prevention measures.
Methodology
Study design
This was a cross-sectional, descriptive study conducted at the Ngaoundere Regional Hospital (NRH) from 1st March to 30th April 2021. The NRH is a 2nd reference (3rd category) hospital in Cameroon’s national classification for health structures. The various missions of NRH are summarised in its consultations, therapeutic management of cases, surgical interventions, prevention, medical analyses, medical training, drug administration, and in the implementation of activities recommended by the Ministry of Public Health (MINSANTE).
Study population
The study population consisted of health care personnel, including specialist doctors (surgeon, dentist, ENT, paediatrician, gynaecologist, etc.), general practitioners, nurses, laboratory technicians, medical and health engineers, and nursing assistants.
Inclusion and exclusion criteria
Health care personnel working at the NRH, who gave their oral consent to participate in the study, were included while administrative personnel working at the NRH, trainees, personnel of the Pharmacy department of the NRH, and health personnel not working at the NRH were excluded.
Sampling
Non-probability convenience and consecutive exhaustive sampling was used.
Epidemiological data and statistical analysis
Data were collected using a survey form and inserted into the Sphinx Plus² - Lexica-V5 edition software for statistical analysis. Statistical processing included the descriptive analysis of socio-demographic and professional data, as well as data on knowledge and practices with regards to BEA. The comparison of variables was carried out using the χ2 test. A value of p < 0.05 were considered statistically significant.
Ethical considerations
This study was authorised by the Institute of Health and Biomedical Sciences in Ngaoundere (N°028/005/DIR/21). The protocol for this study was reviewed and validated by the authorities of the Adamawa Regional Delegation for Public Health (N°234L/RA/DSP/BFP/NGE) and the ethics committee of the NRH (N°105/AR/RA/DRSP/HR/ NGD). Each questionnaire was completed anonymously and with the participant's approval. Any information obtained about the study participants was kept confidential.
Results
Socio-demographic and professional characteristics A total of 172 (78.89%) HCWs agreed to participate in the study, out of a total number of 218 NRH health care personnel. Of the 172 participants in this study, 94 were female (54.70% of the study population), with a male-female ratio of 0.82. The average age was 35.55±7.46 years, with the age group 30-35 years being the most represented. The details are shown in (Table 1).
The hospital units of the respondents were predominantly reception and emergency (14.00%), followed by medicine and paediatrics (11.00% and 10.00% respectively). Approximately 33.10% of HCWs, had an average longevity? of 9.14±6.78 years (range, 1 – 32 years)(Table 1).
| Characteristics | Study population (N=172) | Professional category | |||||
|---|---|---|---|---|---|---|---|
| PMS (n=147) | MS (n=25) | P value | |||||
| Gender M/F | N | % | n | % | n | % | |
| Male | 78 | 45.30% | 62 | 36.00% | 16 | 9.30% | p = 0.043 |
| Female | 94 | 54.70% | 85 | 49.40% | 9 | 5.20% | |
| Marital status | |||||||
| Single | 62 | 36.00% | 51 | 29.70% | 11 | 6.40% | |
| Married | 98 | 57.00% | 85 | 49.40% | 13 | 7.60% | |
| Cohabitation | 6 | 3.50% | 5 | 2.90% | 1 | 0.60% | p = 0.891 |
| Widowed | 1 | 0.60% | 1 | 0.60% | 0 | 0.00% | |
| Divorced | 1 | 0.60% | 1 | 0.60% | 0 | 0.00% | |
| Separated | 4 | 2.30% | 4 | 2.30% | 0 | 0.00% | |
| Age group | |||||||
| Less than 30 | 41 | 23.80% | 39 | 22.70% | 2 | 1.20% | |
| from 30 to 35 | 57 | 33.10% | 43 | 25.00% | 14 | 8.10% | |
| From 36 to 41 | 42 | 24.40% | 40 | 23.30% | 2 | 1.20% | |
| From 42 to 47 | 18 | 10.50% | 14 | 8.10% | 4 | 2.30% | p = 0.003 |
| From 48 to 53 | 10 | 5.80% | 8 | 4.70% | 2 | 1.20% | |
| From and above | 4 | 2.30% | 3 | 1.70% | 1 | 0.60% | |
| Hospital unit | |||||||
| Emergency | 24 | 14.00% | 19 | 11.00% | 5 | 2.90% | |
| Surgery / operating theatre | 16 | 9.30% | 15 | 8.70% | 1 | 0.60% | |
| Gynaecology | 10 | 5.80% | 8 | 4.70% | 2 | 1.20% | |
| Laboratory | 16 | 9.30% | 16 | 9.30% | 0 | 0.00% | |
| Medicine | 19 | 11.00% | 16 | 9.30% | 3 | 1.70% | |
| Paediatrics | 18 | 10.50% | 17 | 9.90% | 1 | 0.60% | p = <0.001 |
| Reanimation | 7 | 4.10% | 6 | 3.50% | 1 | 0.60% | |
| Blood bank | 10 | 5.80% | 10 | 5.80% | 0 | 0.00% | |
| Maternity | 16 | 9.30% | 15 | 8.70% | 1 | 0.60% | |
| Radiology and imaging medical | 4 | 2.30% | 3 | 1.70% | 1 | 0.60% | |
| Day hospital | 17 | 9.90% | 16 | 9.30% | 1 | 0.60% | |
| Dentistry | 9 | 5.20% | 2 | 1.20% | 7 | 4.10% | |
| ORL | 3 | 1.70% | 1 | 0.60% | 2 | 1.20% | |
| Ophthalmology | 1 | 0.60% | 1 | 0.60% | 0 | 0.00% | |
| Psychiatry | 2 | 1.20% | 2 | 1.20% | 0 | 0.00% | |
| Medical profession | |||||||
| Medical Specialist | 14 | 8.10% | 0 | 0.00% | 14 | 8.10% | |
| General Practitioner | 11 | 6.40% | 0 | 0.00% | 11 | 6.40% | |
| Nurse | 57 | 33.10% | 57 | 33.10% | 0 | 0.00% | |
| Midwife/ Birth attendant? | 5 | 2.90% | 5 | 2.90% | 0 | 0.00% | p = 0.001 |
| Laboratory technician | 24 | 14.00% | 24 | 14.00% | 0 | 0.00% | |
| Medico-Sanitary Engineer | 11 | 6.40% | 11 | 6.40% | 0 | 0.00% | |
| Health care assistant | 50 | 29.10% | 50 | 29.10% | 0 | 0.00% | |
| Professional experience | |||||||
| Less than 5 | 58 | 33.70% | 46 | 26.70% | 12 | 7.00% | |
| From 5 to 9 | 41 | 23.80% | 36 | 20.90% | 5 | 2.90% | |
| From 10 to 14 | 39 | 22.70% | 38 | 22.10% | 1 | 0.60% | |
| From 15 to 19 | 19 | 11.00% | 15 | 8.70% | 4 | 2.30% | p = 0.182 |
| From 20 to 24 | 11 | 6.40% | 9 | 5.20% | 2 | 1.20% | |
| 25 and above | 4 | 2.30% | 3 | 1.70% | 1 | 0.60% | |
| Description: Table showing socio-demographic and professional characteristics of study participants; PMS (Paramedical Staff); MS (Medical Staff) | |||||||
Table 1: Socio-demographic and occupational characteristics.
Frequency of accidents with blood and/or other biological fluids in Ngaoundere regional hospital
Of the 172 participants, 62.80% (n = 108) claimed they had been a victim of BEA, 91 participants remembered being a victim of BEA at least once (range, 1 – 4). The relationship between being a victim of BEA and professional category was statistically significant (p = <0.1%), as seen in (Table 2). Nurses, who fall in the category of medical staff, were the most affected by BEA (80.70%).
| Characteristics | BEA Victim | Total | P value | ||||
|---|---|---|---|---|---|---|---|
| YES | NO | ||||||
| n | % | n | % | n | % | ||
| Professional category | 108 | 62.80% | 64 | 37.20% | 172 | 100.00% | |
| PMS | 100 | 68.00% | 47 | 32.00% | 147 | 100.00% | p = <0.1% |
| MS | 8 | 32.00% | 17 | 68.00% | 25 | 100.00% | |
| Profession | 108 | 62.80% | 64 | 37.20% | 172 | 100.00% | |
| Medical Specialist | 4 | 28.60% | 10 | 71.40% | 14 | 100.00% | |
| Medical Doctor | 4 | 36.40% | 7 | 63.60% | 11 | 100.00% | |
| Nurse | 46 | 80.70% | 11 | 19.30% | 57 | 100.00% | p = <0.1% |
| Midwife/ Birth attendant | 3 | 60.00% | 2 | 40.00% | 5 | 100.00% | |
| Laboratory technician | 11 | 45.80% | 13 | 54.20% | 24 | 100.00% | |
| Medical-Sanitary Engineer | 5 | 45.50% | 6 | 54.50% | 11 | 100.00% | |
| Health care assistant | 35 | 70.00% | 15 | 30.00% | 50 | 100.00% | |
| Description: Table showing the frequency of BEA by occupational category. PMS (Paramedical Staff); MS (Medical Staff) | |||||||
Table 2: Frequency of BEA by occupational category.
According to the data in (Table 3), BEA was most common in the treatment room (26.70%), followed by the reception and emergency departments (15.10%), the delivery room (14.00%), the patient's bed (12.80%), the laboratory (8.10%), the operating theatre (6.40%), and the intensive care unit (4.10%) shown in (Table 3).
| Mechanisms of occurrence of a BEA | Professional category | Total (N=172) | P value | ||||
|---|---|---|---|---|---|---|---|
| PMS (n=147) | MS(n=25) | ||||||
| n | % | n | % | n | % | ||
| Puncture | 167 | 97.10% | 142 | 96.60% | 25 | 100.00% | |
| Cutting | 142 | 82.60% | 117 | 79.60% | 25 | 100.00% | |
| Contact of a wound with blood | 136 | 79.10% | 113 | 76.90% | 23 | 92.00% | p = 0.031 |
| Blood splashes on mouth. eyes | 109 | 63.40% | 85 | 57.80% | 24 | 96.00% | |
| Cap with a needle after use | 106 | 61.60% | 83 | 56.50% | 23 | 92.00% | |
| Contact of healthy skin with blood | 51 | 29.70% | 50 | 34.00% | 1 | 4.00% | |
| Description: Table showing the knowledge on mechanisms of occurrence of a BEA by occupational category. PMS (Paramedical Staff); MS (Medical Staff) | |||||||
Table 3: Knowledge on mechanisms of occurrence of a BEA by occupational category.
Mechanisms of occurrence of BEA and risks involved
Mechanisms of occurrence of BEA
According to the participants, their perception of the most common mechanism of occurrence of a BEA was needle stick injury (97.10%), followed by cuts (82.60%) and wound contact with infected blood (79.10%). The relationship between individual perceptions on mechanisms of occurrence of a BEA and occupational category (Paramedical or Medical Staff) was statistically significant (p= 0.031).
Risk factors involved in a BEA
The viral infections HIV, HBV, and HCV were considered potential risks by HCWs, in the following proportions: 99.40%, 96.50% and 95.30% respectively. The relationship between perceived knowledge on the risk of infection with bacteria, viruses, and other microbes due to a BEA, and the professional category was statistically significant with p<0.1% (Table 4).
| Infectious diseases | Professional category | Total (N=172) | P value | ||||
|---|---|---|---|---|---|---|---|
| PMS (n=147) | MS (n=25) | ||||||
| n | % | n | % | n | % | ||
| HIV (AIDS) | 146 | 99.30% | 25 | 100.00% | 171 | 99.40% | |
| Hepatitis C | 141 | 95.90% | 25 | 100.00% | 166 | 96.50% | |
| Hepatitis B | 139 | 94.60% | 25 | 100.00% | 164 | 95.30% | |
| Syphilis | 74 | 50.30% | 20 | 80.00% | 94 | 54.70% | |
| Tetanus | 59 | 40.10% | 21 | 84.00% | 80 | 46.50% | p = <0.001 |
| Ebola | 51 | 34.70% | 20 | 80.00% | 71 | 41.30% | |
| Tuberculosis | 40 | 27.20% | 19 | 76.00% | 59 | 34.30% | |
| Covid-19 | 36 | 24.50% | 16 | 64.00% | 52 | 30.20% | |
| Malaria | 8 | 5.40% | 6 | 24.00% | 14 | 8.10% | |
| Cancer | 7 | 4.80% | 0 | 0.00% | 7 | 4.10% | |
| Description: Table showing the perceived knowledge of infectious risks involved in BEA, by occupational category. PMS (Paramedical Staff); MS (Medical Staff) | |||||||
Table 4: Perceived knowledge of Infectious risks involved in BEA, by occupational category.
Factors involved in the severity of BEA
Infection in the source patient was only known by 92.4% of HCWs (n=159), as a risk factor in increasing BEA severity. The depth of the wound in the source patient was perceived in 85.5% of HCWs (n=147), as another factor that could increase the severity of a BEA. The type of source instrument causing injury was the third risk factor, identified by 81.4% of HCWs (n=140). Approximately 87.2% of the HCWs (n=150) claimed that the vaccination status of the exposed person was not a potential factor in affecting BEA severity. Responses were identical in both PMS and MS groups (p=0.87).
Intervention after a BEA
First aid measures
According to the results shown in (Table 5) on knowledge of first aid in the event of a BEA according to professional category, the most appropriate interventions after a BEA were thought to be; washing the affected area with soap and water (76.20%), disinfection with 70% alcohol or Betadine (62.80%), and disinfection with 1/10 diluted bleach (59.90%). Approximately 40.10% of PMS recommended squeezing the wound to make it bleed and 15.16% recommended disinfecting with pure bleach. The relationship between knowledge of first aid and professional category was statistically significant with p = 0.002.
| First aid measures | Professional category | ||||||
| PMS (n=147) | MS (n=25) | Total (N=172) | P value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | N | % | ||
| Wash with soap and water | 108 | 73.50% | 23 | 92.00% | 131 | 76.20% | |
| Disinfect the wound with 70° alcohol or Betadine | 85 | 57.80% | 23 | 92.00% | 108 | 62.80% | |
| Disinfect with bleach diluted 1:10 | 80 | 54.40% | 23 | 92.00% | 103 | 59.90% | |
| Wash with water only | 59 | 40.10% | 16 | 64.00% | 75 | 43.60% | |
| Squeezing the wound to make it bleed | 59 | 40.10% | 1 | 4.00% | 60 | 34.90% | p = 0.002 |
| Disinfect with pure bleach | 23 | 15.60% | 0 | 0.00% | 23 | 13.40% | |
| Description: this table showing HCWs’ knowledge of first aid in the event of a BEA. PMS (Paramedical Staff); MS (Medical Staff) | |||||||
Table 5: knowledge of first aid in the event of a BEA
Declaration of BEA
Reporting a BEA was perceived as an important response by 76.70% of HCWs, with the lowest perception rates observed among nurses and orderlies, as shown in (Table 6). There was a statistically significant relationship between reporting a BEA and professional category (p < 0.001). Approximately 85.50% of HCWs showed a lack of knowledge for reporting procedures, while 59.9% stated that reporting procedures were complicated.
| Mandatory reporting of BEA | P value | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| n | % | n | % | ||
| Professional category | 132 | 76.70% | 40 | 23.30% | p = 0.003 |
| PMS | 107 | 72.80% | 40 | 27.20% | |
| MS | 25 | 100.00% | 0 | 0.00% | |
| Profession | 132 | 76.70% | 40 | 23.30% | p = 0.018 |
| Medical Specialist | 15 | 100.00% | 0 | 0.00% | |
| Medical Doctor | 10 | 100.00% | 0 | 0.00% | |
| Nurse | 39 | 68.40% | 18 | 31.60% | |
| Midwife/ Birth attendant | 4 | 80.00% | 1 | 20.00% | |
| Laboratory technician | 19 | 79.20% | 5 | 20.80% | |
| Medico-Sanitary Engineer | 11 | 100.00% | 0 | 0.00% | |
| Health care assistant | 34 | 68.00% | 16 | 32.00% | |
| Description: table VI represents the reporting rate of blood exposure accidents by occupational category. All MS affirmed Mandatory reporting of BEA | |||||
Table 6: Distribution of reporting rate of blood exposure accidents by occupational category.
| Universal precautionary measures | Professional category | P value | |
|---|---|---|---|
| %PMS (n=147) | %MS (n=25) | ||
| Wear gloves if there is a risk of contact with blood. biological fluids or soiled equipment | 91.80% | 96.00% | p = 0.013 |
| Place sharps in safety containers immediately after use | 87.80% | 88.00% | |
| Wash your hands before and after each treatment | 83.70% | 80.00% | |
| Do not recap the needles | 74.10% | 96.00% | |
| Do not work on duty if you have skin lesions on your hand | 51.00% | 56.00% | |
| Decontaminate soiled surfaces or objects with water only | 51.00% | 12.00% | |
| Detach the needles by hand after use | 37.40% | 4.00% | |
| Description: this table represented the different universal precautions proposed to the HCWs to choose. About this, the awareness rates varied from 4.00% to 96.00% | |||
Table 7: Knowledge of the different universal precautionary measures by occupational category.
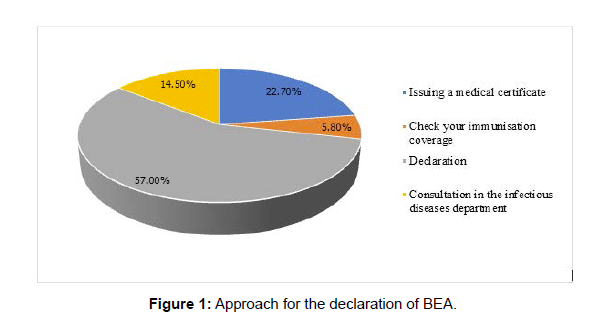
Approximately 57.00% of HCWs stated that a report should be made after BEA, while 22.70% recommended drawing up a medical certificate, as shown in (Figure 1). The 48-hour reporting time limit was known by 18.60% of the HCWs.
Medical follow-up after BEA
The need for medical follow-up after BEA was known by 88.40% (n=152) of the HCWs. According to the professional category, 20/147 PMS were unaware of this (p=0.05). Of the 172 HWs, 88.4% (n=152) were aware of the need to investigate the source patient's HIV status and only 16/147 PMS were unaware of this (p=0.093). The need for post-exposure prophylaxis after a BEA in the presence of an HIVpositive patient or a patient of unknown serology, was known by 86.60% (n=149) of the HCWs. By professional category, only 23/147 PMS (15.60%) were unaware of the need for post-exposure prophylaxis under the conditions described above (p= 0.034).
Prevention of BEA
Training on BEA
The majority of respondents 117/172 (68.0%) stated that they had never received training on BEA.
Protection during care
According to the results obtained, 134/172 (77.9%) of HCWs protected themselves at all times while performing their duties, and 8/172 (4.7%) claimed to protect themselves sometimes, while on duty.
Approximately 84.9% (146/172) of these HCWs confirmed the existence of tools for the prevention of BEA (gloves, nose coverings, gowns) within their department.
Universal precautions
Universal precautions are a standard set of guidelines to prevent the transmission of blood borne pathogens from exposure to blood and other potentially infectious materials (OPIM). Universal precautions were introduced by the Centres for Disease Control (CDC) in 1985, mostly in response to the human immunodeficiency virus (HIV) epidemic. This activity reviews universal precautions and highlights the role of the interprofessional team in their application. The existence of universal precautions in relation to BEA was known by only 57.60% of the healthcare personnel (n=99).
Universal precautionary measures
The Knowledge of the different universal precautionary measures by occupational category
Hepatitis B vaccination
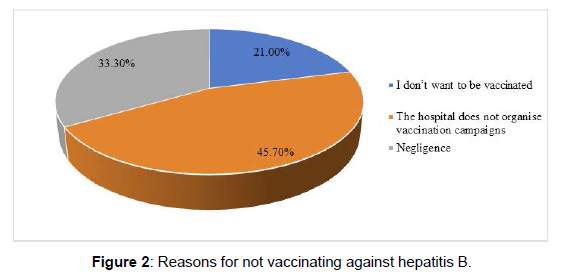
According to the results obtained, 52.90% of the respondents stated that they had been vaccinated against hepatitis B. For those who were not vaccinated, their reasons are shown in (Figure 2) below.
Key points for prevention of BEA
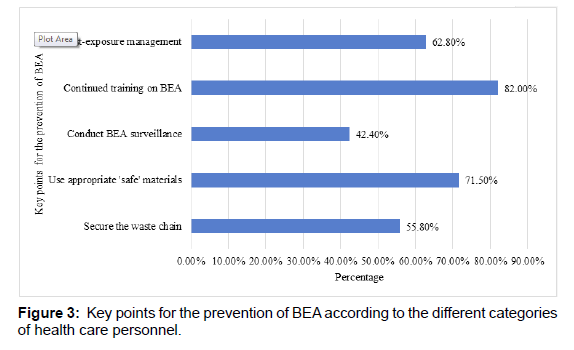
According to the data presented in (Figure 3), most of the HCWs (82.00%) recommended continuing the education on BEA as one of the keys for BEA prevention.
Discussion
Blood exposure accidents are a major concern for HCWs, especially in developing countries. Assessing the knowledge, attitudes and practices of HCWs in the NRH with regards to BEA, was a necessary approach. Out of the 218 health care personnel in the NRH, 172 (78.89%) fully participated in this study. This percentage is comparable to that in most studies dealing with the same subject matter. For example, studies conducted in: Congo Brazzaville (69.9%), Morocco (52.81%), Togo (65,7%), and Ivory Coast (75,5%) [7, 8, 9, 10]. This percentage of HCWs from NRH is the highest yet, and shows the interest of the staff of this hospital in the subject matter. It demonstrates the concern and the need to equip the staff of the NRH on BEA, in order to contribute to the improvement of their working conditions.
The study population was relatively young with an average age of 35.55±7.46 years, predominantly represented by those under 35 years of age (56.90%). Similar data have been reported in the literature [7, 9]. This young demographic could be due to the recruitment of younger HCWs by the MINSANTE in recent years.
The average working experience of the respondents was 9.14±6.78 years, lower than that reported by Ebatetou et al., of 13.7±6.5 years [7] and Younes et al., of 15 years [11]. This further proves that a younger population of healthcare personnel have been recruited by MINSANTE in the last ten years because of the ageing population of HCWs.
Women were predominant in this setting and represented 54.7% of the study population (sex ratio = 0.72). This has equally been observed in other studies including: 54.70% in another study from Cameroon, 57, 50% in Congo Brazzaville, and 72, 50% in Morocco [5, 7, 11]. This high percentage of women is probably because they represent the majority of Cameroon’s population and are implicated in education and science, more now than in the past.
The predominant hospital units of the respondents were the reception and emergency departments (14.00%) followed by the medical department (11.00%). In their study, Ebatetou et al. found a predominance of the emergency and intensive care units (28.3%) followed by the medical unit (27.3%) and the medical-surgical unit (26%) [7]. Bagny et al. in Togo reported a predominance of the medical sector (65.2%) followed by the laboratory (17.7%) [12], Vikkey et al. in Benin found a predominance of surgery (27.2%) and laboratory (17.7%) [13]. In Morocco, Moussa et al. found a predominance of the surgical pole (48.7%) [8], during the course of their work, 62.80% of the HCWs claimed to have been victims of at least one BEA. Similar frequencies have been reported by several authors in sub-Saharan Africa [1, 9, 11, 14]. According to occupational category, BEA were more frequent among paramedical staff than among medical staff (p <0.1%). A study by Younes et al. also reported that paramedical staff was the most exposed to BEA [11].
The staffs of the NRH appears to have a good knowledge of the main mechanisms of occurrence of BEA, namely: needle stick injury (97.10%), skin cut with a sharp object (82.60%) and contact of a wound with infected blood (79.10%). Ebatetou et al. had similar results: needle stick with blood or blood-contaminated biological fluid (85.8%), contact of a wound with infected blood (70.7%) and skin cut with a sharp object (62.20%) [7]. However, these findings differ from those reported by Bagny et al., where needle stick injuries represented 100% of all BEAs in their setting [12]. Nevertheless, needle stick injuries remain the main risk factor in the occurrence of BEA reported frequently in the literature [11, 12, 15].
The type of infection in the source patient from which a BEA originated, the depth of an infected wound brought in contact with a HCW, and the type of equipment causing injury were the three main factors known by most HCWs (> 81.40%), to be involved in the severity of a BEA. Based on professional category, the responses were identical for both paramedical and medical staff (p=0.87).
The three main infectious agents (HIV, HBV, and HCV) were perceived as risk factors by 99.40%, 96.50% and 95.30% of HCWs respectively. These results were similar to those reported by Laraqui et al. and Ebatetou et al. [1, 7], but differ from those of Ndiaye et al. which were 36.40% for HIV, 29.6% for HBV and 23.3% for HCV [16], and Younes et al. who reported rates of 0.3%, 3% and 30% for HIV, HCV and HBV respectively [11]. Based on professional category, medical staff was more aware of the risk of contracting infection, than paramedical staff. The diversity of knowledge acquired during the different basic training courses, between the paramedical and medical staff would explain the difference in perception. The need for initial and on-going training on BEA is essential for all health care personnel in order to aid in the proper management of infectious waste.
First aid after a BEA
In case of a BEA such as a prick or blood spill on injured skin, the first emergency care consists of, immediately cleaning the wound with running water and soap, disinfecting with a chlorinated derivative (Dakin's solution or Bleach (usually 5.25% or 6.00%–6.15% sodium hypochlorite depending upon manufacturer) is usually diluted in water at 1:10) or, cleaning with 70% alcohol or iodised polyvidone in dermal solution (ensuring a contact time of at least 5 minutes). In case of a blood spill on a mucous membrane, such as the conjunctiva, rinsing thoroughly, preferably with physiological serum or with water for at least 5 minutes is sufficient. In case of percutaneous exposure, the HCW should not cause the wound to bleed. A risk assessment should be carried out immediately after the BEA, by a referring physician. In this study, 76.20% of participants recommended washing with soap and water after an accident which is similar to 68.80% found in the Koné et al. study and 50% in the Saint-Laurent et al. study [17, 18]. With regards to disinfection, 61.35% recommended it, while 21%, 39.3%, and 96% recommended disinfection in the study conducted by Koné et al., Ebatetou et al., and, Saint-Laurent et al. respectively [7,17,18]. This low percentage in the knowledge of standard protocols in the event of a BEA can be explained by the fact that there is a lack of ongoing training on BEA, as only 32.00% of the HCWs stated that they had received training on BEA.
As concerns intervening after a BEA, the practice of inducing a bleed was found in 34.90% of the participants in the study. According to the professional category, this rate represents 59/147 of paramedical staff and 1/25 of medical staff. This is much higher than the rate reported by Gondo et al. which was 3.33% of respondents [14]. This common attitude of bleeding superficial wounds has no scientific basis and could be considered risky as it turns a superficial wound into a deep wound [14]. It would be important to raise awareness on what to do in case of a BEA.
Post-exposure prophylaxis
Post-exposure prophylaxis (PEP) is currently the only way to reduce the risk of HIV infection when in contact with an HIV-infected patient or contaminated objects. The importance of using PEP in the presence of an HIV-positive patient or a patient of unknown serology was confirmed by 86.60% of HCWs. In Congo Brazzaville, Ebatetou et al. found 79.20% while in Côte d'Ivoire, Eholie et al. found 42.5% in favour of PEP [7, 10]. The difference in knowledge on the need to prescribe PEP after a BEA is related to the professional category. Only 15.60% of paramedical staff were unaware of the need for PEP (p= 0.034). This is logical from the point of view of the different functions and educational levels between medical and paramedical personnel. On the other hand, the difference noted between the two categories, by Eholie et al. was not statistically significant [10].
Declaration of blood exposure accidents
As far as the medico-legal approach is concerned, the declaration of the accident at work must be made 24-48 hours after the accident to the occupational physician or the referring physician, who provides information on the risks incurred, analyses the circumstances in which the accident occurred, assesses the need for serological follow-up, and draws up the initial descriptive medical certificate in order to guarantee the rights of the injured [1]. There is a misconception with regards to the legal time limit for reporting a BEA to occupational medicine and the need to contact the referring doctor for medical follow-up. Usually, a maximum period of 48 hours is required for reporting a BEA by public sector employees, while reporting to a medical doctor for follow-up has to be an immediate action.
During the study, 76.70% of the respondents in all occupational categories thought all BEA should be reported. This result is similar to those obtained by Eholie et al. (84.60%) and Ebatetou et al. (89, 20%) [7, 10]. The reasons for non-reporting of BEA were mainly due to personal negligence (85.50%), followed by lack of knowledge on reporting procedures (59.9%), and complicated procedures to follow after BEA (16.9%). It is important to report BEA for better management in case of exposure, and to ensure better surveillance of BEA within the hospital.
Investigation of the patient's serological status after a BEA
In our survey, the majority (90.60%) of respondents thought that the patient's serological status should be investigated after a BEA. This result ties closely with those by Ebatetou et al (86.3%) and Bagny et al. (87.80%) [7,12]. knowledge of a patient's serological status makes it possible to determine the next steps to take in the event of exposure. Approximately 88.40% of the participants in the study thought medical follow-up was necessary after a BEA. These results are similar to those obtained by Ebatetou et al. (87.00%) [7].
Knowledge and attitudes/practices
Training on BEA
Approximately 32.0% of the caregivers claimed to have never received training on BEA. This rate is close to the one reported by Moussa et al. of 28.70% [8]. To prevent BEA, the need for initial and continuing training on BEAs remains essential for its health care personnel.
Protection during care
About 77.9% of HCWs claimed to protect themselves during care. This result is higher than that reported by Gondo et al. 31.3% [14]. The availability of a means of prevention against BEA within the services and the routine supply of personal protective equipment (goggles or visor, single-use gown, single-use mask, single-use gloves, hydro alcoholic solution) in the different areas of activity would greatly contribute to observing safety measures and preventing BEA.
Universal precautionary measures
The existence of universal measures for the prevention of BEA was only known by 57.60% of the health care personnel. This result is similar to certain studies found in the literature: in Congo Brazzaville (55.7%), in Ivory Coast (68.7%), in Senegal (68%), in The Democratic Republic of Congo (80%), and higher than those found in Benin (45.5%): [7, 10, 16, 19]. Generally, knowledge on universal precautionary measures, varied from 4.0% to 96.0%. It is necessary to know the universal precautions to apply during care, for any patient whatever is his/her infection status.
Hepatitis B vaccination
Hepatitis B virus is a major public health problem, and Cameroon, with a high prevalence of 9.2% in the general population and 8.7% among health workers, is among the most affected countries in the world and in Africa [20]. The management of HVB is still very problematic as it is very costly despite the public health measures already put in place by the government, the best way to prevent the disease remains vaccination.
Approximately 52.90% of respondents claimed to have been vaccinated against hepatitis B. Comparing the vaccinated and unvaccinated participants, versus the BEA and non-BEA groups, a significant variation was observed with regards to BEA (p=0.03). Vaccinated participants were mostly found in the non-BEA group. In the study by Gondo et al. the reported rate of vaccination against hepatitis B was 66.94% and only 28.9% of respondents reported having been vaccinated against hepatitis [14]. In the absence of vaccination,the risk of contamination by the hepatitis B virus from a patient carrying HBsAg by health personnel is four times higher than that of the general adult population not working in a hospital environment. The most frequently mentioned reason for non-vaccination was the absence of a vaccination campaign organised by the hospital (45.70%). Hospitals should organise free screening and vaccination campaigns for their staff because effective vaccination remains the best means of prevention against this hepatitis B viral infection.
Suggestion from staff interviewed on improving working conditions
Most respondents called for training (82.0%) on BEA as one of the key points of BEA prevention, followed by the use of appropriate 'safe' equipment (71.50%). This would be due to the absence of initial and continuous training on BEA, which should normally be organised by MINSANTE through programmes and courses, but by the hospital management through the occupational medicine department, the infectious diseases and hospital hygiene departments.
Conclusions
This study highlighted the knowledge, and practices of healthcare personnel at the NRH, in relation to BEA. A high frequency (62.80%) of BEA was reported by the staff of the NRH. The implementation of a surveillance system for occupational contamination among HCWs is imperative. More than half of the staff (68.0%) had never received training on BEA. Hence, the need for education on BEA for NRH health staff remains essential. It was noted that a significant number of the participants in this study (77.90%) took precautions to avoid BEA. The average knowledge of the respondents about the risks of infection and the main infectious agents that can be transmitted during a BEA is no guarantee. Given the low rate of vaccination against hepatitis B, initiatives should be taken to encourage healthcare personnel to be vaccinated against hepatitis B in order to protect themselves, their family members and patients.
Recommendations
Ministry of Public Health
- The establishment BEA reporting and information systems, awareness and health education on BEA in all health facilities;
- Creation of an occupational health service;
- Provide health coverage for its employees;
To the administration of the Ngaoundere Regional Hospital
• Implement a policy of routine HIV, HBV, HCV screening for all hospital workers;
• Ensure continuous training of health workers on BEA (declaration, management and prevention);
• Always provide staff with personal protective equipment (gloves, nose coverings, gowns, safety glasses or a face mask, single-use waterproof apron);
To the health staff of the NRH
• Participate in various workshops and ongoing training on BEA;
• Consider any source of biological fluid as potentially infectious;
• Report all cases of BEA;
• Rigorously observe universal protective measures;
• Vaccinate against certain infections (Hepatitis B)
Competing Interests
The authors declare no competing interests.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Authors' Contributions
All authors contributed to this work. They all read and approved the final version of the manuscript.
Acknowledgments
The authors wish to thank all the health professionals and the administration of the NRH for their participation in this study.
References
- https://hi.art1lib.com/book/17097786/c53d97
- https://www.hrw.org/fr/news/2018/06/06/lepidemie-debola-en-rd-congo
- https://cdn.who.int/media/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/20-who-nepal-sitrep-covid-19-v5.pdf?sfvrsn=d7c7c5ba_2
- https://www.who.int/occupational_health/topics/needinjuries/en/
- https://www.memoireonline.com/05/11/4531/Analyse-des-connaissances-sur-les-accidents-dexposition-au-sang--cas-de-lhopital-regional-de-B.html
- Eock CM (2015) Accidents d’exposition au sang à l’Hôpital Central de Yaoundé : Connaissances, attitudes et pratiques du personnel paramédical. Health Sci Dis 19: 12-15.
- Ataboho EE, Makele C, Ngatali SCF, Boumba ALM, Moukassa D (2018) Accidents d ’ Exposition au Sang : Connaissances et Impact de la Catégorie Professionnelle dans un Hôpital du Congo Brazzaville hospital of Congo Brazzaville. Health Sci Dis 19:10-15.
- Moussa B, Boujemaa EM, Aziz N, Karima ER (2017) Connaissances, attitudes et pratiques vis-à-vis des précautions standard chez les soignants du Centre hospitalier universitaire Hassan II de Fès (Maroc). EMHJ23:1.
- Kara-Pékéti K, Magnang H, Bony JS, Robin H, Frimat P (2011) Prévalence des accidents professionnels d’exposition au sang chez le personnel soignant au Togo (Afrique). Arch des Mal Prof et de l'Environnement 72: 363-369.
- EholieSP, Ehui E, Yebouet-Kouame BY, Simo TA, Tanon A, et al. (2002) Analyse des pratiques et connaissances du personnel soignant sur les accidents d’exposition au sang à Abidjan (Côte d’Ivoire). Med Mal Infect 32: 359-368.
- Azzouzi Y, Bakkali M, Khadmaoui A, Ahami AOT, Hamama S, et al. (2014) Les accidents avec exposition au sang chez les soignants : connaissances, attitudes, pratiques et prévention dans la région de Gharb au MarocInternational. Int J Innov Sci 7: 557-570.
- Bagny A (2014) Connaissances, attitudes et pratiques du personnel soignant sur le risque de transmission des hépatitis virales B et C en milieu hospitalier au Togo. Med sante trop 23:300-303.
- Hinson AV, Lawin H, Gounongbe F, Aguêmon B, Sossa CJ, et al. (2016) Epidemiological Aspects of Blood Exposure Accidents With the Healthcare Workers Staff of a Peripheral Hospital in Benin. J Biol Sci 2: 48-63.
- Gondo D, Effoh D, Adjoby R, Konan J, Koffi S (2016) Connaissances, attitudes et pratiques (CAP) du personnel soignant sur les accidents d’exposition au sang (AES) dans 4 maternités d’Abidjan. Revue Africaine d’Anesthésiologie et de Médecine d’Urgence 21:16-20.
- Bouzgarrou L, Kacem I, Henchi MA, Kraim A, Kammoun S (2021) Les accidents d’exposition au sang dans le Centre Hospitalo Universitaire de Mahdia : Etude sur sept ans. Revue Tunisienne de Pathologie Professionnelle et de l’Environnement 2:44–48.
- Ndiaye CBD (2011) Les accidents avec exposition au sang (AES) au CHNU de Fann, Dakar, Sénégal. Cah Méd Inter Prof(CAMIF).
- Koné MC, Mallé KK (2015) Les accidents d’exposition au sang : connaissances et pratiques des personnels de santé d’un hôpital du Mali. Bulletin de la Société de pathologie exotique 108:369–372.
- Saint-Laurent P, Sarrazin D, Pik JJ, Kadi Z (2005) Evaluation des connaissances et pratiques des infirmières vis-à-vis du risque d’accident d’exposition au sang : résultats d’une enquête multicentrique en Picardie. Hygiènes 13:3.
- N. M. Bambenongama and J. L. Likwela (2013) Connaissances, attitudes et pratiques des professionnels de santé face aux précautions standards en milieu hospitalier. Sante Publique 25:663–673.
- https://www.scidev.net/afrique-sub-saharienne/news/personnel-sante-hepatite-b-cameroun/
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Karyom DAN, Bong-Akee S, Honore ER, Gael OM, Collins BN, et al. (2022) Blood Exposure Accidents among Health Care Personnel at the Ngaoundere Regional Hospital in Northern Cameroon: Knowledge, Practical Attitudes, and Means of Prevention. Occup Med Health 10: 412.
Copyright: © 2022 Karyom DAN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3014
- [From(publication date): 0-2022 - Dec 04, 2025]
- Breakdown by view type
- HTML page views: 2506
- PDF downloads: 508