Case of a 38 Year Old Male with Pulmonary Crohn's Disease
Received: 03-Apr-2018 / Accepted Date: 18-Apr-2018 / Published Date: 25-Apr-2018 DOI: 10.4172/2161-069X.1000563
Abstract
We present the case of a 38 year old male who presented with several weeks of respiratory complaints found to be the result of Crohn's Disease (CD) with Pulmonary Manifestations. His past medical history was significant for long standing CD and he was on immunosuppressive therapy with vedolizumab. Initial findings were concerning for Bronchopneumonia or a possible Metastatic Disease. Subsequent work-up eliminated infectious and cancerous etiologies. This included blood cultures, HIV, Quantiferon Gold Assay, PPD, and bronchial biopsy results. Furthermore, GMS, AFB, and Truant special stains were negative for fungal elements and mycobacteria.
Eventually, the patient underwent a VATS (video-assisted thoracoscopic surgery) biopsy, which revealed noncaseating granulomas with prominent neutrophilic microabscesses. This finding led to the differential diagnosis of either a vasculitis, or a pulmonary CD. The lack of cavitation, fibrinoid necrotizing epithelioid and eosinophilic granulomas, necrotizing granulomatous vasculitis, glomerulonephritic symptoms, and a negative ANCA essentially ruled out the diagnosis of eosinophilic granulomatosis with polyangiitis. Biopsy of the lung also did not reveal the characteristic geographic necrosis and acute and chronic inflammation changes which are typical of granulomatosis with polyangiitis. These findings ultimately led to the diagnosis of Pulmonary CD with pulmonary necrobiotic nodules. This is an extremely rare manifestation of the Inflammatory Bowel Syndrome and one that clinicians should have within their differential upon treating patients with long-standing CD and pulmonary complications.
Keywords: Internal medicine; Gastroenterology; Inflammatory bowel disease
Introduction
Crohn’s disease (CD) is a type of inflammatory bowel disease that has been universally recognized as a chronic illness which can have profound emotional and social impacts on an individual. It typically encompasses a granulomatous inflammation which can involve any part of the GI tract, usually with terminal ileum and/or colonic involvement. This inflammation is best described as transmural with bowel wall thickening, linear ulcerations, and submucosal thickening that eventually leads to characteristic endoscopic findings of mucosal cobblestoning and “skip lesions.”
Patients with CD typically present with fever, abdominal pain, diarrhea (often without blood), fatigue, and weight loss. Growth retardation may be seen in children. Oftentimes perianal disease, such as an anorectal fissure, fistula, or abscess may be the presenting complaint. Over time, chronic inflammation can result in complications, such as intestinal obstruction due to edema and fibrosis, toxic megacolon, intestinal perforation, and fistulas to the bowel, bladder, vagina, skin, and soft tissue.
Bile salt malabsorption can also occur leading to cholesterol gallstones and/or oxalate kidney stones. There is also an increased risk of intestinal malignancy and amyloidosis. CD can also be characterized by the various extraintestinal manifestations which can evolve in up to 25% of patients [1]. Of these extraintestinal manifestations, arthritis, erythema nodosum, pyoderma gangrenosum, and primary sclerosing cholangitis are the most common.
Traditionally, the lungs have not classically thought to be affected. Recently however, there has been growing evidence for pulmonary involvement directly caused by extraintestinal CD which can involve the tracheobronchial tree, the lung parenchyma and the pleura [2]. Recent data suggests that the overall prevalence of concomitant bronchopulmonary manifestations is only 0.4% but subclinical alterations from CD are believed to involve at least half of adults regardless of sex [3]. Pulmonary involvement in CD is rare; however, it is increasingly becoming a more recognized clinically significant entity that clinicians need to be able to distinguish from vasculitis or infectious causes [4].
Case Report
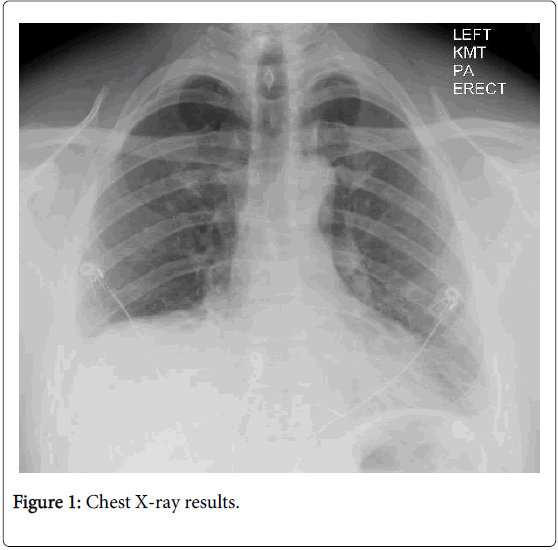
A 38 year old Caucasian man presented with worsening shortness of breath and a productive cough for the last 1-2 weeks. His symptoms were associated with fever, pleuritic chest pain, chills, night sweats, generalized weakness, fatigue, and joint pain. His past medical history was significant for ileocolonic CD, which was previously being treated with adalimumab but had recently been switched to vedolizumab several months earlier. He denied any recent changes in weight, sick contacts, recent travel, hematochezia, melena, and recent diarrhea or constipation. He was also a non-smoker and used only chewing tobacco and occasional alcohol. Of note, the patient stated that prior to these developments he had never had similar symptoms. Initial chest X-ray was remarkable only for bilateral pleural effusions with lower lobe airspace opacities (Figure 1).
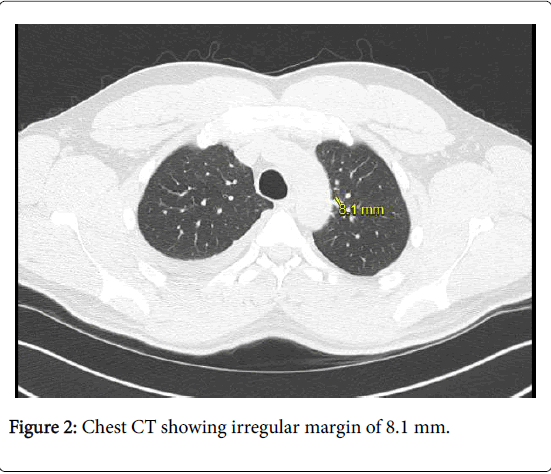
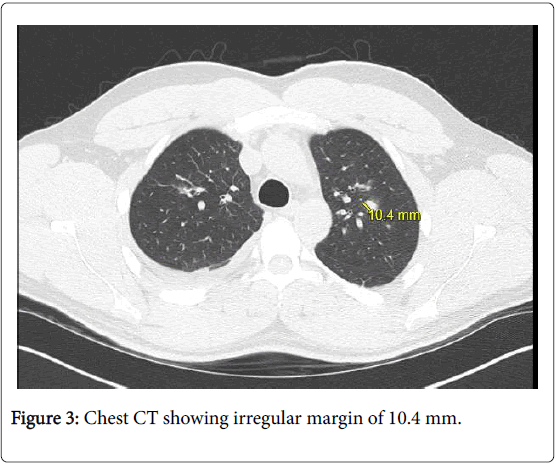
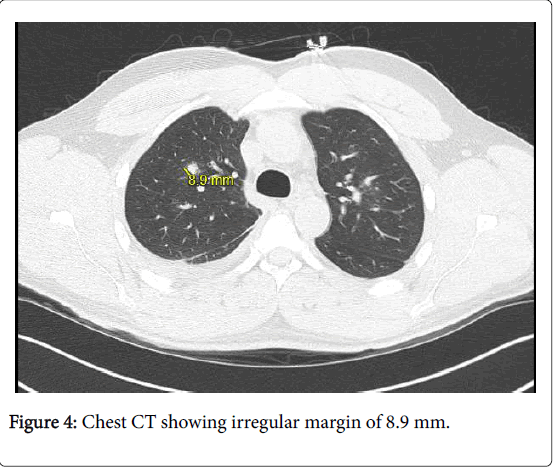
Subsequent chest CT demonstrated scattered ground-glass opacities with bilateral pulmonary nodules which appeared spiculated with irregular margins (Figures 2-4). There was a bilateral pleural effusion with consolidation in the left lung base that was believed to represent a possible inflammatory change. These findings were initially concerning for bronchopneumonia versus metastatic disease. Subsequently, the patient underwent bronchoscopy with bronchoalveolar lavage, cryobiopsy, and CT-guided biopsy of the pulmonary nodules; all of which were ultimately non-diagnostic and revealed only benign lung tissue with mild fibrosis and neutrophils. Ultrasound guided thoracentesis was performed which removed 330 ml of pleural fluid. Analysis of this fluid revealed a transudate effusion. Cytology examination was non-contributive. The patient’s pleuritic chest pain was quite severe and managed with opioid pain medication. He was given a trial of methylprednisone and a 10-day course of ampicillin/ sulbactam.
The steroids appeared to stop the patient’s spiking fevers and nocturnal diaphoresis but no underlying diagnoses could be established. All infectious workup, including blood cultures, HIV, Quantiferon Gold Assay, PPD, and bronchial biopsy results were negative. Furthermore, GMS, AFB, and Truant special stains were negative for fungal elements and mycobacteria. Infection was thus no longer supported by these negative special stains and despite the low sensitivity of these methods, an infectious etiology became highly unlikely considering the patient’s other extensively negative testing. Eventually, the patient underwent a VATS (video-assisted thoracoscopic surgery) biopsy, which revealed non-caseating granulomas along with granulomas containing prominent neutrophilic microabscesses.
No epithelioid or multinucleated giant cells were observed. This finding led to the differential diagnosis of either a vasculitis or a pulmonary manifestation of CD. Granulomatosis with polyangiitis typically presents with a combination of glomerulonephritis with necrotizing granulomatous vasculitis of the upper and lower respiratory tracks. Pulmonary nodular infiltrates are common in this condition as well, but are often found with cavitation. Eosinophilic granulomatosis with polyangiitis also typically presents with opacities and pulmonary nodules on chest radiograph. For our patient, urinalysis was unremarkable and ANCA was negative. Biopsy also did not reveal the characteristic geographic necrosis and acute and chronic inflammation changes which are typical of granulomatosis with polyangiitis. VATs biopsy of the lung nodule also did not reveal the fibrinoid necrotizing epithelioid and eosinophilic granulomas one would expect with Eosinophilic Granulomatosis.
Blood vessels and bronchia were unremarkable with no evidence of vasculitis or geographic necrosis which further argued against Eosinophilic Granulomatosis with Polyangiitis and Granulomatosis with Polyangiitis. Ultimately, the diagnosis of pulmonary Crohn’s disease with pulmonary necrobiotic nodules was established given the pathology results and negative ANCA and serology results. The patient was started on systemic steroids at a dose of 0.5-1 mg of prednisone/kg daily with a maximum daily dose of no more than 60 mg. The patient’s pleuritic chest pain and shortness of breath improved. The patient was then discharged on a prolonged steroid course which would remain in place for at least one year. He was also started on prophylactic sulfamethoxazole/trimethoprim along with vitamin D supplementation since the patient was going to be on chronic steroid therapy.
Discussion
Pulmonary Crohn’s disease is an extremely rare manifestation of Crohn’s disease with a paucity of reported cases. The overall prevalence of pulmonary involvement is believed to be around 0.4% [5]. Although subclinical changes representing underlying bronchial inflammation have been described in about half of adults with CD [3]. There are a number of proposed mechanisms by which the lungs are thought to become involved in CD. These include the common embryological origin of the lung and gastrointestinal tract [6], similar immune system mechanics within the pulmonary and intestinal mucosa [7], the presence of circulating immune complexes and auto-antibodies [8], and the adverse pulmonary effects of some drugs used in the treatment of CD. These medications include sulfasalazine, mesalamine, and methotrexate, and the development of opportunistic lung infections as the result of immunosuppressive treatment [2].
The most common presentation is typically in a patient with longstanding CD with atypical chest pain and pulmonary symptoms. Symptoms encompass non-specific pleuritic chest pain, shortness of breath either with rest or exertion, and cough which can be productive or dry. Fevers, chills, and night sweats may or may not be present. Interstitial lung disease with and without organizing pneumonia, noncaseating granulomatous inflammation and fibrosis, parenchymal nodules with granulomata, alveolitis, alveolar consolidation, mycobacterium xenopi infection, colopleural fistula and fecopneumothorax have all been described as pulmonary manifestations of CD [2]. Bronchiectasis has become recognized as the most commonly reported airway disease, and is defined as an abnormal and irreversible dilation of the medium sized bronchioles [9]. However, a less-recognized pulmonary extra intestinal manifestation involves the development of pulmonary nodular disease which is rarely reported in the literature [10]. It is this lesser known manifestation of pulmonary CD which our patient was found to have.
Conclusion
Pulmonary CD is a rare extraintestinal manifestation. Within this disease category, the pulmonary nodular manifestation is even more infrequent. When this specific extraintestinal pathology is found, the histology usually shows nodules composed of aggregates of neutrophils with necrosis and frequent cavitation [10]. The mainstay of treatment is typically recognized as steroids with possible infection prophylaxis [2]. It is important for clinicians to be aware of the lung manifestations of CD as they can often vary in presentation and can represent a confusing diagnostic picture necessitating a complex work-up. Patients with CD should undergo pulmonary evaluation including physical examination, chest X-ray and pulmonary function tests. Invasive measures such as bronchoscopy and thoracoscopy, can also be considered to reach a final diagnosis. Physicians should have a high index of suspicion for pulmonary Crohn’s in CD patients with pleuritic chest pain and pulmonary nodules in order to initiate appropriate treatment and avoid complications.
References
- Ephgrave K (2007) Extra-intestinal manifestations of crohn’s disease. Surg Clin North Am 87: 673-680.
- Lu DG (2014) Pulmonary manifestations of crohn’s disease. World J Gastroenterol 20: 133.
- Bonniere P, Wallaert B, Cortot A, Marchandise X, Riou Y, et al. (1986) Latent pulmonary involvement in crohn’s disease: Biological, functional, bronchoalveolar lavage and scintigraphic studies. Gut 27: 919-925.
- Rothfuss KS, Stange EF, Herrlinger KR (2006) Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol 12: 4819-4831.
- Rogers BHG, Clark LM, Kirsner JB (1971) The epidemiologic and demographic characteristics of inflammatory bowel disease: An analysis of a computerized file of 1400 patients. J Chronic Dis 24: 743-773.
- MacDermott RP, Nash GS, Nahm MH (1989) Antibody secretion by human intestinal mononuclear cells from normal controls and inflammatory bowel disease patients. Immunol Invest 18: 449-457.
- Bienenstock J, McDermott M (1978) A common mucosal immunologic system involving the bronchus, breast and bowel. Adv Exp Med Biol 107: 53-59.
- Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, et al. (2012) Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 491: 119-124.
- Butland RJA, Cole P, Citron KM, Turner-Warwick M (1981) Chronic bronchial suppuration and inflammatory bowel disease. Qjm: Int J Med 50: 63-75.
- Golpe R, Mateos A, Pérez-Valcárcel J, Lapeña JA, GarcÃa-Figueiras R, et al. (2003) Multiple pulmonary nodules in a patient with Crohn’s disease. Respiration 70: 306-309.
Citation: Sperling M (2018) Case of a 38 Year Old Male with Pulmonary Crohn's Disease. J Gastrointest Dig Syst 8: 563. DOI: 10.4172/2161-069X.1000563
Copyright: © 2018 Sperling M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4803
- [From(publication date): 0-2018 - Oct 14, 2025]
- Breakdown by view type
- HTML page views: 3946
- PDF downloads: 857