Case Report: Acute Calcific Tendonitis at the Pectoralis Major Attachment-A Benign Cause of Red Flag Signs
Received: 20-Dec-2018 / Accepted Date: 31-Dec-2018 / Published Date: 07-Jan-2019 DOI: 10.4172/2472-016X.1000127
Abstract
Introduction: Acute calcific tendonitis at the pectoralis major insertion is rarely reported in the radiology literature, but not in the Orthopaedic literature. We present a case that illustrates the typical findings with discussion from a shoulder surgeon, and a senior radiologist.
Case Study: A 60-year-old woman was woken at night with sudden onset left shoulder and arm pain. She was otherwise systemically well. Her shoulder range of motion was globally restricted. Past medical history included previous spinal surgery and a hepatitis A infection within the last year.
Plain radiographs of the shoulder and humerus were unremarkable save for a small an anterior proximal humeral protuberance at the junction of proximal third and distal two-thirds of the humeral shaft. Blood tests were unremarkable. CT and MRI imaging showed a calcific tendon with associated cortical defect, and surrounding inflammation.
Because of the sinister red flag symptoms (night pain) and suggestion of cortical erosion with periosteal reaction, the differential diagnosis list included sarcoma. For this reason, it was referred to the local sarcoma service. This was reviewed by a senior radiologist. The diagnosis of calcific tendonitis of pectoralis major calcific tendonitis was made. The decision was made by the Sarcoma MDT to not biopsy the lesion but instead review clinically with interval scan and safety netting.
On six week clinic follow up the patient’s symptoms had improved. Because of the knowledge regarding this potential diagnosis, unnecessary invasive diagnostic procedures (CT biopsy) or surgeries were avoided. Repeat MRI at three month showed resolution of changes.
Conclusion: Both Orthopaedic surgeons within sarcoma services and wider members of the multidisciplinary team should be aware of this diagnosis. This would help to prevent over investigation of benign self-limiting pathologies.
Keywords: Calcific tendonitis; Osteosarcoma; Sarcoma; Pectoralis major
Introduction
Calcific tendonitis is a common diagnosis often seen around the rotator cuff musculature and has been reported extensively in the literature [1]. Calcific tendonitis in the pectoralis major tendon is rare and can be mistaken for malignant pathology. We present a case of calcific tendonitis in the pectoralis major tendon. The aim of this report is to describe the case, make recommendations of management and to summarise the literature.
History
A retired right hand dominant 60-year-old woman woke with sudden onset left shoulder and arm pain. The pain was so severe that she attended the Emergency Department. She was otherwise systemically well. She had globally restricted shoulder movement to a third of normal on passive and active movement due to the pain. The pain was maximal anteriorly in the upper arm. Her history was typical of someone with acute calcific tendonitis of the shoulder except the pain was maximal in the upper part of the upper arm and not in the shoulder. Past medical history included previous spinal surgery and a hepatitis A infection within the last year but nil else of note. She had no previous complaints regarding her left shoulder. She takes no regular medication and has no allergies.
Investigations
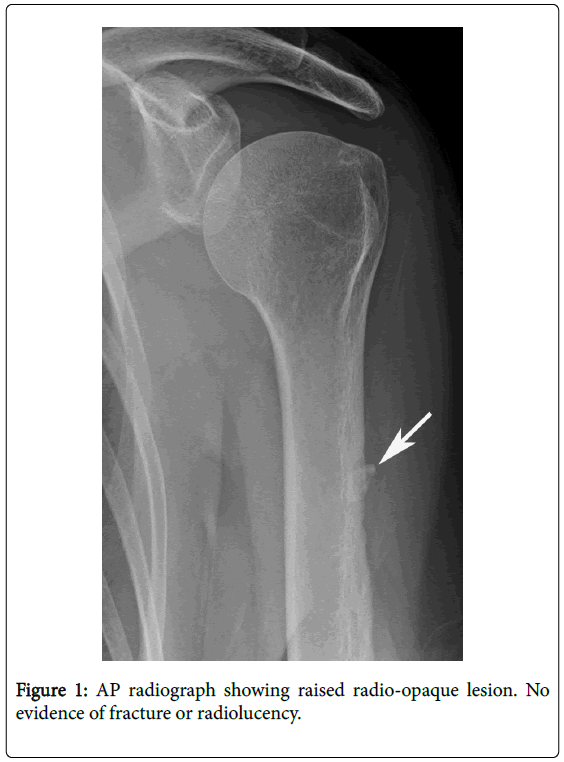
Plain radiographs of the shoulder and humerus were unremarkable save for a small anterior proximal humeral protuberance at the junction of proximal third and distal two-thirds of the humeral shaft (Figure 1). Blood tests were unremarkable with a slightly raised white cell count of 11.6 (laboratory range maximum 10.8), C reactive protein 12 (laboratory range maximum four) and a slightly raised Alkaline phosphatase of 157 (laboratory range 30-130). Calcium was normal. Erythrocyte sedimentation rate was not performed. She was discharged home and an appointment was made to see an orthopaedic surgeon specialising in the shoulder joint.
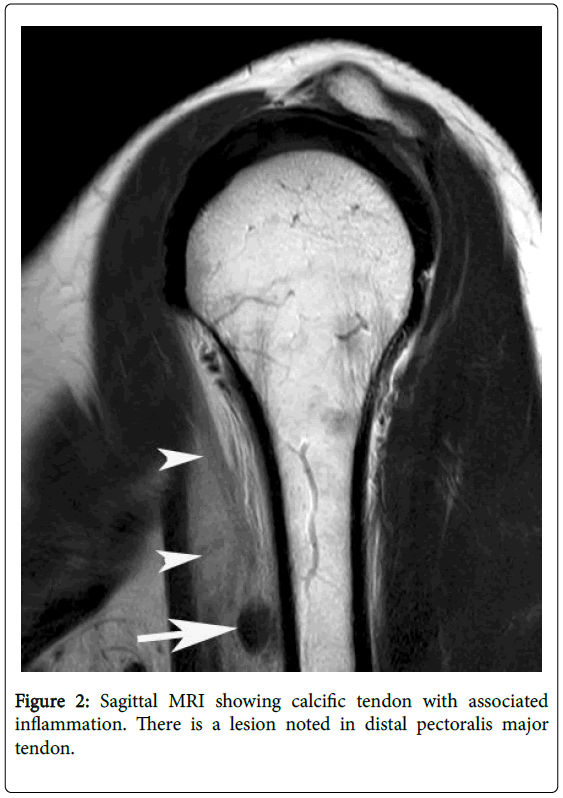
The patient underwent Magnetic resonance imaging (MRI) examination of the shoulder and the upper arm in the outpatient department (Figure 2). MRI imaging modality was chosen to better assess the soft tissue of the arm. This was reported locally as “a 13 mm irregular ovoid lesion between the long head of biceps tendon and the anterior margin of the humerus, 75 mm distal to the humeral head; it appears exophytic, apposed to the cortex of the lateral lip of the bicipital groove. It displaces the biceps tendon anteriorly. There is a large amount of surrounding soft tissue oedema. The [pectoralis major] tendon does not appear inflamed or torn”. The differential diagnosis included paraosteal sarcoma.
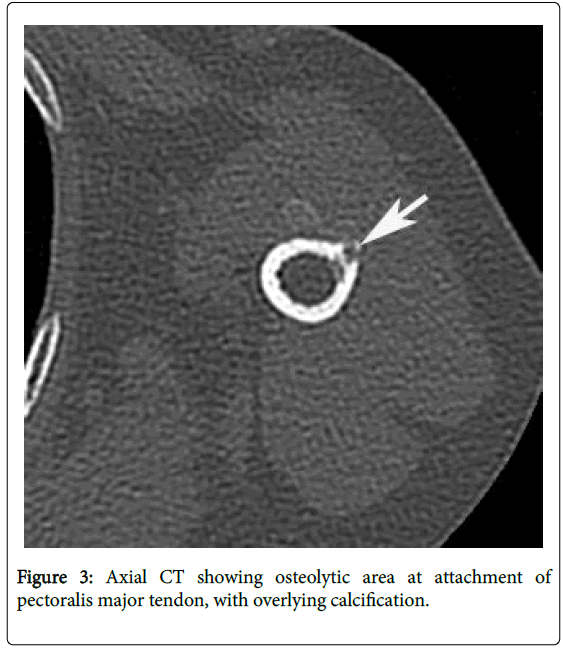
The patient then underwent a Computerised Tomography (CT) scan for further assessment of the lesion in a following outpatient appointment (Figure 3). CT was utlised as it best assesses cortical involvement and break through. This reported “an area of ossification of the biceps closely related to the proximal shaft of the humerus, there is a small associated defect in the cortex of the humerus.”
Because of differential diagnosis including parosteal osteosarcoma, the patient was referred to a tertiary sarcoma centre. Review of the scans by the senior radiologist felt this was typical of acute calcific tendonitis of the pectoralis major insertion, a benign pathology. Consequently, it was advised that biopsy of the lesion was not necessary. As with more common acute calcific tendonitis of the rotator cuff, the patient was initially managed conservatively with simple analgesia and physiotherapy [1].
Follow up
Telephone consultation follow up at six weeks revealed the painless range of motion had increased. Repeat MRI at three months showed resolution of soft tissue inflammation and associated cortical reaction. Patient was discharged with safety netting and no further invasive management, including biopsy, was required.
Discussion
Calcific tendonitis, caused by calcium hydroxyapatite deposition in tendons, is a common pathology encountered by orthopaedic shoulder specialists. Frequently, calcific tendonitis affects rotator cuff muscles, particularly supraspinatus [2]. This pathology has also been reported to affect other skeletal muscles including gluteals [3], vastus lateralis [4], and gastrocnemius [5]. Involvement in the pectoralis major insertion is a rare occurrence. Calcific tendonitis of the pectoralis major tendon insertion has been reported in the literature previously [6]. Our management varies from Durr (1997) as we did not require tissue biopsy to confirm our diagnosis, due to radiological investigation, and propose conservative management. This offers confirmation of different centre perspective of biopsy not being required for investigation of this condition, as reported by Flemming in 2003.
Pathogenesis of calcific tendonitis remains unclear. One leading theory suggests cartilage metaplasia as a response to hypoxaemia. The supraspinatus has an area- the critical zone- with a relatively poor blood supply. This might explain the prevalence of the pathology in the vascular watershed area of the supraspinatus. It is during the period of reabsorption of the deposited crystals that pain is most severe. This is thought to be linked to increased vascularity in the tendons during reabsorption [1]. Absorption pathophysiology of these calcium hydroxyapatite crystals remains unclear and requires further research [7].
Bone erosion can also be seen with calcific tendonitis. Cortical erosion is the most common manifestation of bone involvement in calcific tendonitis [8]. Despite this, radiological evidence of bone destruction can be indicative of malignant diagnoses [9] and therefore careful assessment of calcific tendonitis patients is required.
In retrospect one can see that the opacity seen on the plain radiographs is an area of calcification in the soft tissues. This is similar to the radiologically observed calcification that is usually seen in patients with acute calcific tendonitis of the rotator cuff musculature.
The MRI shows the typical features of acute inflammation at the level of the pectoralis major tendon with calcification. CT scan showed osteolytic area in humerus with overlying ossification in keeping with potential bone erosion.
The multidisciplinary team recommended conservative management of this patient with observation, interval scanning and safety netting. This decision was because of the atraumatic history, satisfactory serum biochemistry results and the typical radiological findings of calcific tendonitis of the pectoralis major tendon. If the symptoms had failed to settle, the patient would have had further blood tests looking at inflammatory markers, repeat scan looking for development and the patient would be for consideration of tissue biopsy.
The condition can be treated with non-steroidal anti-inflammatory drugs (non-steroidal anti-inflammatory drugs), physiotherapy or cortisone injections [2]. Surgery can be suggested, with good outcome, in patients who do not respond to conservative measures [10]. However, these management options hinge on correct initial diagnosis.
Recommendation
Orthopaedic surgeons need to be aware of this unusual diagnosis. Appropriate radiological imaging (Initially X-ray, followed by MRI to look for any soft tissue component and then assessment with CT to assess the bone cortex more accurately) can help pinpoint this diagnosis under guidance of an experienced musculoskeletal radiologist. This will prevent invasive biopsy to confirm the diagnosis. Conservative treatment can be trialed initially with analgesia and physiotherapy. Interval scanning can be used if there remains any concern about resolution. Given sinister alternative diagnoses, there should be a low threshold for referral to an appropriate bone tumour centre for further assessment if any concern remains.
Consent
Patient provided consent for submission of this case report.
Competing Interests
Authors declare Nil competing interests.
Author’s Contributions
AS Analysed radiological investigations and provided figures used in this documentation. BG provided this case for review and offered insight in shoulder pathology. CGS was major contributor in writing the manuscript. All parties reviewed manuscript prior to submission.
Acknowledgements
Many thanks to the London Sarcoma Multidisciplinary team.
References
- Uhthoff HK, Loehr JW (1997) Calcific Tendinopathy of the rotator cuff pathogenesis, diagnosis, and management. J Am Acad Orthop Surg 5: 183-191.
- Chianca V, Albana D, Messina C, Midiri F, Mauri G, et al.(2018) Rotator cuff calcific tendinopathy: From diagnosis to treatment. Acta Bio Medica Atenei Parmensis 89: 186-196.
- Thornton MJ, Harries SR, Hughes PM, Whitehouse R, Carradine S (1998) Calcific tendinitis of the gluteus maximus tendon with abnormalities of cortical bone. Clin Radiol 53: 296-301.
- Ramon FA, Degryse HR, De Schepper AM, VanMark EA (1991) Calcific tendinitis of the vastus lateralis muscle: A report of three cases. Skeletal Radiol 20: 21-23.
- Iguchi Y, Ihara N, Hiijoka A, Uchida S, Nakamura T, et al. (2002) Calcific tendinitis of the gastrocnemius: A report of three cases. J  Bone Joint Surg 84: 431-432.
- Dürr HR, Lienemann A, Silbernagl H, Nerlick A, Refior HJ (1997) Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion. Eur Radiol 7: 1215–1217.
- Darrieutort-laffite C, Blanchard F, Le Goff B (2018) Calcific tendonitis of the rotator cuff: From formation to resorption. Joint Bone Spine 85: 687-692
- Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, et al.(2003) Osseous involvement in calcific tendinitis: A retrospective review of 50 cases. Am J Roentgenol 181:965-972.
- Teo HE, Peh WCG (2004) Primary bone tumours of adulthood. Cancer Imaging 4:74-83.
- Verstraelen FU, Fievez E, Janssen L, Morrenhof W (2017) Surgery for calcifying tendinitis of the shoulder: A systematic review.  World J Orthop 8: 424–430.
Citation: Stephens CG, Goldie B, Saifuddin A (2019) Case Report: Acute Calcific Tendonitis at the Pectoralis Major Attachment–A Benign Cause of Red Flag Signs. J Orthop Oncol 4: 127. DOI: 10.4172/2472-016X.1000127
Copyright: © 2019 Stephens CG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7315
- [From(publication date): 0-2018 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 6293
- PDF downloads: 1022