Combined Posterior and Anterior Ankle Arthroscopy as Effective Treatment for Ankle Kashin-Beck Disease
Received: 10-Jul-2018 / Accepted Date: 03-Oct-2018 / Published Date: 10-Nov-2018
Abstract
Kashin-Beck disease (KBD) is an endemic disease which may affect extremity joints. The ankle joint is commonly involved in KBD due to its undertaking all the weight of the body. Ankle arthroscopy combined with hindfoot arthroscopy has a significant effect in treating patients with ankle KBD in the short term, especially in improving the range of ankle motion. Yet the arthroscopic treatment of ankle KBD has highlighted the lack of research to assess the arthroscopic approach for treating this disease. In this study, a prospective study of patients previously suffering from ankle Kashin- Beck then undergoing arthroscopic surgery was carried out. 30 feet of 26 patients with ankle Kashin-Beck Disease received treatment of ankle arthroscopy during October 2013 and November 2014, involving 12 men and 14 women, aging from 29 to 64 years old were involved. Our results suggested treatment for ankle KBD by combined anterior and posterior arthroscopy has a significant effect in improving symptoms both anteriorly and posteriorly.
Level of evidence: Level II (low-powered prospective randomized trial)
Keywords: Kaschin-Beck disease; Ankle; Arthroscopy; Anterior and posterior
Introduction
Kashin-Beck disease (KBD) is an endemic disease involving many joints, especially distal joints, of which most commonly affected joints are the knees, ankles, wrists, elbows, with a pathological basis of cell apoptosis of articular cartilage and growth plate cartilage. It was first reported in 1919, and more than 1million [1] individuals involved with KBD in a limited endemic area in the western and northeast area of China, extending all the way to the Eastern Siberia, Russia, and a small part in Northern. In China, keshan county of Heilongjiang province is an active endemic area of KBD, where the subjects of our study mostly came from.
Hinse-Nkamp [2] suggested that the ankles joints were inevitably involving in 89.5% of KBD patients, the clinical manifestations include progressive pain, recurrent swell, restricted movement, and secondary osteoarthritis of ankle joint, eventually, growth retardation and disability in its advanced stages, which are mostly responsible for the poor quality of life, due to its higher incidence of the ankle and serious consequences for the daily life, the study of treatment for ankle KBD is essential.
During the past few decades, arthrotomy had been one of the most prevalent approaches in the treatment of ankle diseases. As the arthroscopy technique has constantly improved, it has replaced arthrotomy with its highly effective, minimal invasion, and lower rates of complications. However, the research on arthroscopic treatment for ankle KBD was rare, as it is a disease of throughout the joint. In other words, both anterior and posterior ankle joint are involved, based on above thoughts. In this study, we analyzed 30 feet of 26 patients with ankle KBD who were surgically treated by ankle arthroscopy in our hospital during October 2013 and November 2014 to test the efficiency of arthroscopic debridement by combined anterior and posterior approach for treating ankle Kashin-Beck disease is effective.
Research Methodology
Subjects
A total of 26 patients (12 men and 14 women) with ankle KBD received treatment of ankle arthroscopy during October 2013 and November 2014 were involved in this study. The patients had a mean age of 42.1 years (range 29 to 64). There were 12 right ankles, 10 left ankles, and 4 cases of bilateral ankles, which all were treated at the same time with a median history of 4.3 years (range 6 months to 12 years).
Inclusion criteria
A definitive diagnosis of KBD, following the diagnostic criteria of KBD which was ratified by Chinese State Administration for Quality and Technology Supervision in 1995, a conservative treatment was performed at least three months which consisted of oral nonsteroidal anti-inflammatory drugs, physiotherapy, activity modification, a limit motion of ankle joint. X-ray demonstrated osteophytes forming on the anterior and posterior aspects of the ankle along with an enlargement ankle, sclerosis of tibiotalar aspect, cystic lesion or a collapse of the bone cortex.
Exclusion criteria
An extremely narrowing joint space which could not present enough operating space even by a traction device, the motion of dorsiflexion and plantar flexion was too limited to operate, a severe deformity which needed arthrotomies such as osteotomy or arthrodesis and coagulopathy gout.
Surgical techniques
After induction of spinal anesthesia, the patient was placed in a supine position with the ankles placing just over the distal edge of the operating table to allow free dorsiflexion and plantar flexion to provide enough space, a traction device which made the neurovascular structures more vulnerable to damage was not utilized unless necessary [3]. A pneumo-tourniquet was used in the root of the affected thigh, with a pressure of 300 mmHg, the standard anteromedial and anterolateral portals were made at a length of 5 mm. A syringe needle was inserted into the joint space to guide the arthroscopy along with to expand available space by injecting normal saline. An ankle arthroscope with a 30° angle was then applied to examine the tibiotalar, the lateral interarticular sulcus of the talus, the neck of talus, the medial interarticular sulcus of the talus, deltoid ligament, the wall of the posterior joint capsule, and the medial compartment of ankle joint successively. After that, the hypertrophic synovial synovium and scar tissues were subsequently resected to clear up the field of operation, any detached articular cartilage fragment or any intraarticular free body was required to remove by an arthroscopic shaver, care was taken to ensure a stable cartilage rim around the lesion religion of talus cartilage, above all, the most indispensable procedure was removing impinging bone of the anterior border of distal tibia and talus until the impinging was relieved judged by moving the ankle joint passively.
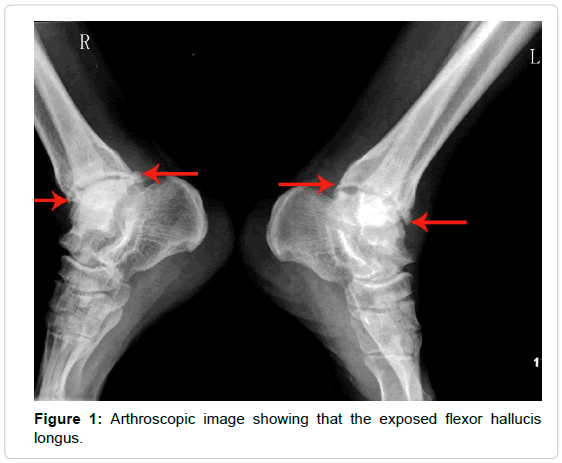
The patient was then turned over to the prone position. Standard poster lateral and posteromedial portals described by Van Dijk [4] were made adjacent to the flexor halluces longus on a line drawn from lateral malleolus parallel to the sole of the foot. It was critical to locate the tendon of the flexor hallucis longus (Figure 1) so as to avoid damaging the posteromedial vessels and nerves. Any posterior pathologic tissues, particularly the osteophytes of posterior tibia were polished by a high-speed abrasive drilling or resected by a rongeur until the impinging was relieved. After a thorough hemostasis of the region where the osteophytes were resected, the two small incisions were then closed. A compression bandage was applied after surgery. The opposite ankle was then operated by the same approach if the patient was bilateral ankles involved.
Active range of motion was allowed the following day and full weight bearing was allowed 2 weeks after surgery, for those who had bilateral ankles surgery, we recommended a little later than 2 weeks after surgery for full weight bearing.
Evaluation
Clinical results were assessed by comparing AOFAS scores, VAS pain scores, WOMAC scores, and active plantar and dorsal flexion angles preoperatively and postoperatively at a period of 3 months, 6 months, and 12 months, the AOFAS scores was graded as excellent, good, fair, or poor and was assessed at the final follow-up visit.
Statistical analysis
All the data were analyzed by using SPSS version 19.0, the statistical results were indicated as mean ± SD. Preoperative and postoperative differences were considered significant when the p-value was ≤ 0.05. Comparisons of preoperative and postoperative scores were made using paired t- tests.
Results
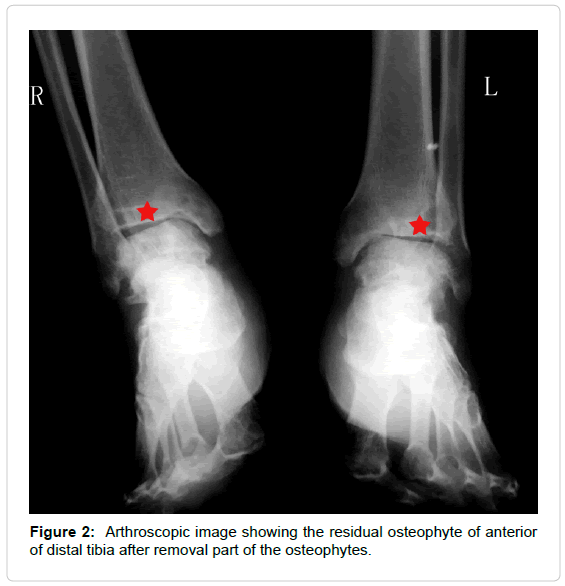
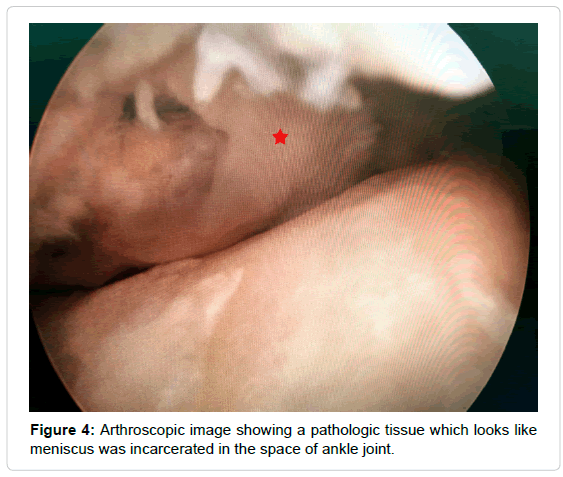
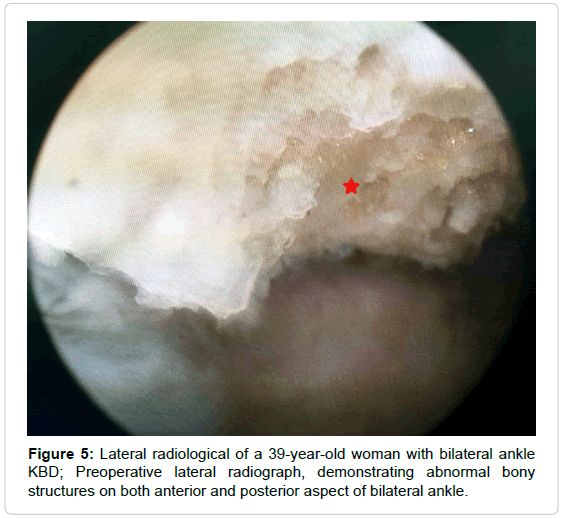
Among the 26 patients (30 ankles), osteophytes formation at the anterior and posterior of joint margins were present in all the subjects (Figures 2 and 3), free bodies were present in 18 subjects, Chondral damage of tibial pla fond or talar dome was found in 24 subjects. The tissues seem like meniscus were present in 6 subjects (Figure 4).
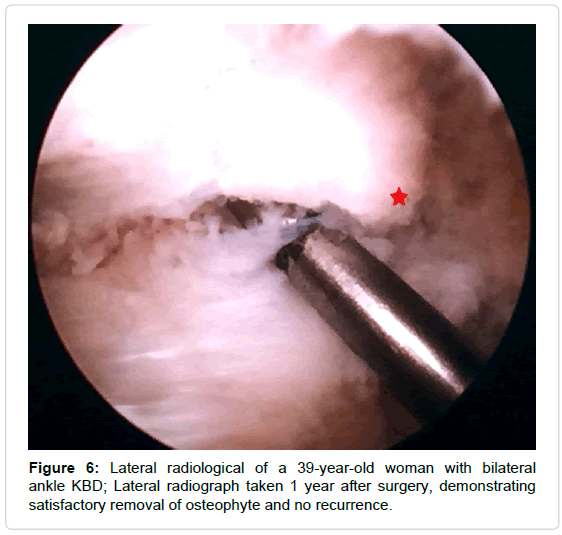
The preoperative scores were assessed by an experienced physiotherapist who was unaware the details of our study, all patients who involved this study have received a follow-up at a period of 3 months, 6 months, and 1 year by the same physiotherapist and were operated by a single senior surgeon. The follow-up results showed that all incisions were primary healing, no complications, such as deep surgical wound infection or neurovascular injury occurred. No X-ray plain film revealed a recurrence of either anterior or posterior osteophyte (Figures 5 and 6).
The median AOFAS score increased from 59.4 points preoperatively to 91.7 points at final follow-up (p<0.01), with an excellent and good rate of 88.67% (26 was excellent and good of 30 subjects), and the median VAS score was changed from 4.64 points preoperatively to 1.02 points at final follow-up (p<0.01). Median WOMAC score was changed from 24.24 to 4.71 at final follow-up (p<0.01), Median active plantar and dorsal flexion angles improved significantly from 10.8° and 13.45° before surgery to 39.2° and 33.78° at the final follow-up respectively (p<0.01, p<0.01) (Table 1).
| Peroid | AOFAS | VAS | WOMAC | Plantar flexion degree | Dorsal flexion degree |
|---|---|---|---|---|---|
| Pre-operative | 59.43 ± 6.7 | 4.64 ± 0.56 | 24.24 ± 4.05 | 10.8 ± 3.7° | 13.45 ± 3.1° |
| 3 months | 75.2 ± 3.72 | 1.87 ± 0.22 | 9.25 ± 3.17 | 30.5 ± 5.8° | 27.11 ± 2.46° |
| t | 14.979 | 9.671 | 18.561 | 19.347 | 15.285 |
| P | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
| 6 months | 89.5 ± 8.25 | 1.15 ± 0.32 | 6.43 ± 2.81 | 37.1 ± 8.2° | 31.34 ± 5.2° |
| t | 24.372 | 12.539 | 22.218 | 19.673 | 17.346 |
| P | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
| 1 year | 91.7 ± 5.19 | 1.02 ± 0.23 | 4.71 ± 1.43 | 39.2 ± 4.7° | 33.78 ± 5.3° |
| t | 26.749 | 14.351 | 25.326 | 21.241 | 19.873 |
| P | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
Abbreviations: AOFAS: The American Orthopedic Foot and Ankle Society Score System, VAS: Pain and Visual Analog Score, WOMAC: The Western Ontario and Mcmaster Universities.
Table 1: Results of arthroscopic treatment for ankle KBD at 3-month, 6-month, 1-year follow-up (N=30 feet in 26 patients).
Discussion
The cause of KBD remains unclear. It has been suggested that the deficiency of selenium, high humic acid levels in drinking water, and fungi on storage grains are the causes of KBD. Besides, the genetic involvement [5-8] and inflammation and immune activation [9] had also been proved to play an important role in KBD. KBD occurs in childhood and continues to progress even in adulthood, during which the symptoms and signs become more severe due to continuous damage to the joint cartilage [10].
Conservative treatment mainly including rest, physical therapy [11], oral administration vitamin C and vitamin E, Selenium preparations and chondroitin sulfate are effective approaches at the early stage of KBD; oral administration Selenium preparations were confirmed to block the disease progress in childhood in recent study [12]. For those who have a serious pain around ankle joint, oral non-steroidal anti-inflammatory drugs and sodium hyaluronate injection of ankle joint have been mainly utilized, but neither presents a significant therapeutic effect [13]. Arthrotomy was typically performed after non-operative management fails, since this method was associated with massive wounds and high incidence of neurovascular injury [14]. Ankle arthroscopy has been one of the most effective approaches instead of arthrotomy in the examining and the treatment of ankle osteoarthritis since it has the potential to shorten the recovery time and limit the surgical morbidity [15]. Ankle arthroscopy was first proposed and applied by Johnson since 1980s, but it was developed slowly during a long time for that the space of tibiotalar joint is too limited, which leads to a high technological requirement of the operation. As the arthroscopy equipment has been continuously improved in recent years, the skills of operating ankle arthroscopy is enhanced as well [16-18], then van Dijk [3] developed the posterior approach of hind foot Arthroscopy, since that the ankle pathologic features located far posterior in the ankle joint remain difficult to reach from anterior portals because of its shape.
Several studies which had been published to describe anterior and posterior arthroscopic treatment for ankle disease of impingement syndrome mainly caused by overuse or post-traumatic problems had shown to be effective results [19-24]. However, the study about the arthroscopic treatment of ankle KBD is rare because of its endemicity which means that it occurs only in certain areas and leads to limited study previous methods had mostly dealt with the anterior issues only by anterior approach regardless of the posterior pathological changes, which demonstrated a significant improvement in anterior symptoms after surgery. Our study proposed a method combined anterior and posterior arthroscopic debridement for treating ankle KBD, which compensates for the neglect of posterior ankle issues of previous studies. It has proved to be a considerable significance by contrasting the score of AOFAS, VAS, WOMAC and the degrees of plantar and dorsal flexion preoperatively and postoperatively after 3 months, 6 months, and 1 year (p<0.01). Thus, we concluded that arthroscopic debridement by anterior and posterior approach can alleviate pain, increase the motion degree of ankle, improve the function of walking in the treatment of ankle KBD, especially significant in improving activity of ankle joint in the short term.
How to operate properly and validly during the procedure is the key to obtaining a good therapeutic effect, here are some issues which need to be paid attention to we had concluded:
1. A pneumatic tourniquet was bundled on the affected thigh to reduce the bleeding so as to make the surgery field clearer, with a pressure of 300 mmHg at maximum 90 minutes, however, there was more probability of neurovascular injury;
2. We slid a cushion to prop up the affected hip slightly, then marked the position of the vessels and nerves, the typically anteromedial and anterolateral portals was utilized, if necessary, an auxiliary incision was also needed, it was critical to locate the tendon of the flexor hallucis longus (Figure 4) so as to avoid damaging the posteromedial vessels and nerves. Then the facet of medial malleoli and the talus, the sagittal sulcus and medial sulcus of the talus, the lateral shoulder of talus, the lateral tibiofibular joint, and the lateral sulcus of talus were examined successively, in addition, the posterior tibiotalar capsular and the posterior compartment of the ankle joint were also included;
3. Not only could it clear the surgery field, but also alleviate the symptoms of pain to remove the hypertrophic synovium, there still might be some synovium remained in the medial sulcus for its narrow spaces, moreover, the depth of reaching was limited in the case of vessels and nerves injury.
4. The soft tissues which were incarcerated in any joint space of ankle must be removed thoroughly for the reason that we regarded the Incarcerated tissues as a direct source of pain in ankles during walking.
5. After removing the desquamated cartilage of talus and tibia, care was taken to avoid creation of an overly large defect from excessive debridement, the instable cartilage must be resected through for that it might sequentially proceed Incarcerating or to be a free body.
6. A high-speed abrasive drilling and a rongeur were utilized to remove osteophytes which were always spected in the anterior and posterior of distal tibia and to flatten the residual surface, What calls for special attention is that the high-speed abrasive drilling needs to be operated with its back to subcutaneous tissue in the case of damaging vessels and nerves. Issues about how much of the osteophyte needed to be removed have been varying, we considered that the amount was just enough once the ankle joint range freely, which was judged by moving the affected ankle joint passively without any impingement, observed by arthroscopy;
7. The free body which was always sought out in the medial ankle joint cavity must be taken out intact.
Though more time-consuming and complicated, the method of arthroscopic debridement by anterior and posterior approach had a significant effect in alleviating symptoms of patients with ankle KBD, especially the function of extension and flexion of ankle joint. However, since the KBD is a progressive disease [20-24], arthroscopic debridement can only delay instead of interrupt its progress, even though we had concluded that the arthroscopic debridement has a significant effect in the short term in treating ankle KBD, the midterm and long term observation is still needed to prove whether these significant results persist with time. Besides, for those cases of severe deformity and degeneration of ankle joint, arthrodesis, osteotomy, or even arthroplasty instead of arthroscopy is still needed. There were several limitations of this study. First, there were a limited number of patients and the period of postoperative follow-up was short, a long research and more subjects of this method are needed to further confirm the efficacy. Second, as this was a study in the absence of a control group, the effect of other surgical strategies, such as only by frontier approach or posterior approach, could not be directly compared. Third, our research was a retrospect study which was viewed as a preferred method by us for treating ankle KBD before it was conducted, which introduced the possibility of confirmation bias.
Conclusion
Combined posterior and anterior ankle arthroscopy was effective for the treatment of ankle Kashin-Beck Disease by alleviating pain around the ankle joint, increasing both plantar flexion and dorsal flexion degrees of the ankle, and improving the function of walking in the short term.
Future Prospects
What is the current knowledge on the topic?
The arthroscopic treatment of ankle Kashin-Beck disease had highlighted the lack of research, to assess the arthroscopic approach to treating this disease.
What question did this study address?
Combined posterior and anterior ankle arthroscopy was effective for the treatment of ankle Kashin-Beck Disease by alleviating pain around the ankle joint.
What does this study add to our knowledge?
Treatment for ankle KBD by combined anterior and posterior arthroscopy has a significant effect in improving symptoms both anteriorly and posteriorly.
How might this change clinical pharmacology or translational science?
We suggest treating KBD with combined anterior and posterior arthroscopy.
Conflict of Interest
The authors have not communicated any conflict of interest.
Funding
None.
References
- Wang, L.H., Fu, Y., Shi, Y.X & Wang, W.G T-2 toxin induces degenerative articular changes in rodents: link to Kaschin-Beck disease. Toxicol Pathol, 2011.39:502-507.
- Hinsenkamp, M., Ryppens, F., Begaux, F., Mathieu, F., De Maertelae, V., Lepeire, M., et al. The anatomical distribution of radiological abnormalities in Kashin-Beck disease in Tibet. Int Orthop, 2001.25:142-146.
- De Leeuw, P.A.J., Golanó, P., Clavero, J.A & Van Dijk, CN Anterior ankle arthroscopy, distraction or dorsiflexion? Knee Surg Sports Traumatol Arthrosc, 2010.18:594- 600.
- Van Dijk, C.N., Scholten, PE., Krips, R A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy, 2000.16:871-876.
- Guo, X., Ma, W.J., Zhang, F., Ren, F.L., Qu, C.J & Lammi, M.J Recent advances in the research of an endemic osteochondropathy in China: Kashin-Beck disease. Osteoarthritis Cartilage, 2014.22:1774-1783.Â
- Han, J., Li, D., Qu, C., Wang, D., Wang, L., Guo, X., et al. Altered expression of chondroitin sulfate structure modifying sulfotransferases in the articular cartilage from adult osteoarthritis and Kashin-Beck disease. Osteoarthritis Cartilage, 2017. 25:1372-1375.
- Tai, Z., Huang, L., Lu, F., Shi Y., Ma, S., Cheng J., et al. Association study of candidate genes for susceptibility to Kashin-Beck disease in a Tibetan population. Med Genet, 2017.18:69.
- Yu, F., Duan, C., Zhang, X., Yao, D., Si, G., Gao, Y., et al. RNA-seq analysis reveals different gene ontologies and pathways in rheumatoid arthritis and Kashin-Beck disease. Int J Rheum Dis, 2018.21:1686-1694.
- Han, J., Wang, W., Qu, C., Liu, R., Li, W., Gao, Z., et al. Role of inflammation in the process of clinical Kashin-Beck disease: latest findings and interpretations. Inflamm Res, 2015.64:853-860.
- Huang, Q., Zhou, Z.K., Ma, J., Li, Y., Yang, X., Shen, B., et al. The arthropathic and functional impairment features of adult Kashin-Beck disease patients in Aba Tibetan area in China. Osteoarthritis Cartilage, 2015.23:601-606.
- Mathieu, F., Suetens, C., Begaux, F., De Maertelaer, V & Hinsenkamp, M Effects of physical therapy on patients with Kashin-Beck disease in Tibet. Int Orthop, 2001.259:191-193.
- Zhao, Z.J., Li, Q., Yang, P.Z., Wang, H., Kong, L.C., Wang, L.H., et al. Selenium: A protective factor for Kaschin-Beck disease in Qing-Tibet plateau. Biol Trace Elem Res, 2013.153:1-4.
- Pesquer, L., Guillo, S., Meyer, P & Hauger, O US in ankle impingement syndrome. J Ultrasound, 2014. 17: 89- 97.
- Coull, R., Raffiq, T., James, L.E & Stephens, MM Open treatment of anterior impingement of the ankle. J Bone Joint Surg Br, 2003. 85:550-553.
- Willits, K., Sonneveld, H., Amendola, A., Giffin, J.R., Griffin, S & Fowler, P.J Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy, 2008. 24:196-202.
- Jacobson, K., Ng, A & Haffner K.E Arthroscopic treatment of anterior ankle impingement. Clin Podiatr Med Surg, 2011, 28:491-510.
- Weiss, W.M., Sanders E.J., Crates J.M & Barber F.A Arthroscopic Excision of a Symptomatic Os Trigonum. Arthroscopy, 2015. 31:2082- 2088.
- Henkelmann, R., Schmal, H., Pilz, I.H., Salzmann, G.M., Dovi-Akue, D & Südkamp, N.P Prospective clinical trial of patients who underwent ankle arthroscopy with articular diseases to match clinical and radiological scores with intra-articular cytokines. Int Orthop, 2015. 39:1631-1637.
- Ogut, T., Ayhan, E., Irgit, K. & Sarikaya, A.I Endoscopic treatment of posterior ankle pain. Knee Surg Sports Traumatol Arthrosc, 2011.19:1355-1361.
- Wang, X., Zhao, Z., Liu, X., Zhang, J & Shen, J Combined posterior and anterior ankle arthroscopy for posterior and anterior ankle impingement syndrome in a switching position. Foot Ankle Int, 2014. 35:829-833.
- Miyamoto,W., Takao, M., Matsui, K & Matsushita,T Simultaneous ankle arthroscopy and hindfoot endoscopy for combined anterior and posterior ankle impingement syndrome in professional athletes. J Orthop Sci, 2015. 20:642-648.
- Kim, H.K., Jeon, J.Y, Dong, Q., Kim, H.N & Park, Y.W Ankle Arthroscopy in a Hanging Position combined with hindfoot endoscopy for the treatment of concurrent anterior and posterior impingement syndrome of the ankle. J Foot Ankl Surg, 2013. 52:704-709.
- Phisitkul, P., Tennant, J.N., Amendola, A Is there any value to arthroscopic debridement of ankle osteoarthritis and impingement? Foot Ankle Clin, 2013. 18:449-458.
- Wu, C., Zheng, J., Yao, X., Shan, H., Li, Y., Xu, P., et al. Defective autophagy in chondrocytes with Kashin-Beck disease but higher than osteoarthritis. Osteoarthritis and Cartilage, 2014. 22:1936-1946.
Citation: Li W, Wang W, Mei X, Shi Z (2018) Combined Posterior and Anterior Ankle Arthroscopy as Effective Treatment for Ankle Kashin-Beck Disease. Cell Mol Biol 64: 153.
Copyright: © 2018 Li W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4653
- [From(publication date): 0-2018 - Oct 07, 2025]
- Breakdown by view type
- HTML page views: 3587
- PDF downloads: 1066