Comparison of colorectal cancer burden in: opportunity for sharing lessons and expand partnership in health care in two BRICS countries
Received: 10-Jul-2020 / Accepted Date: 20-Aug-2020 / Published Date: 27-Aug-2020 DOI: 10.4172/2161-069X.1000626
Abstract
Background: Colorectal cancer (CRC) is now ranked among the three most frequent cancers globally. As the level of human development is increasing, so is the CRC burden in South Africa (SA) and Brazil (BR). Monitoring CRC epidemiological trends is important to ensure responsive policies informing public health detection and control. The study compared CRC incidence and mortality patterns in SA and BR.
Methods: National-level prevalence, incidence, mortality data was obtained from the WHO cancer database (GLOBOCAN 2018) and extracted for the two countries.
Results: CRC is the top four and five leading cancer in SA and BR, respectively. In 2018, the number of new CRC cases in South Africa 6 937 cases (6.5% of all cancer cases) while in Brazil there were 51 783 (9.3% of all cancer cases). The CRC incidence rate in SA was 1.1 times higher in males than in females, while in BR, CRC rate was 1.07 times higher in females than in males (females: 10.2, males: 9.5 per 100 000). The incidence cumulative risk was slightly lower in in South Africa (1.03%) than in Brazil (1.2%) - The mortality cumulative risk was at 0.54% in South Africa and 0.60% in Brazil. The highest age-standardized incidence rate (ASIR) is observed in Brazil with 19.6 per 100 000 population compared to South Africa that reported 14.4. per 100 000 population. The age-standardized mortality rates (ASMRs) were above 10 per 100 000 population for both sexes in both countries.
Conclusion: Epidemiological variation in CRC between countries reflects differences in terms of socio-economic development. Noting that the CRC burden is increasing, there are opportunities for sharing lessons learned between developed and developing countries, to improve surveillance systems at sub-national levels. In addition, the data highlight the needs for targeting CRC screening campaigns by gender, socio-economical status, ethnicity background and geography to yield better results.
Keywords: Colorectal cancer; CRC incidence and mortality; South Africa; Brazil
Introduction
The Global Burden of Cancer Study 2018 (GLOBOCAN) reported that colorectal cancer (CRC) ranks as the 3rd most common cancer globally. The report, states that globally, there were over 1.8 million new CRC cases and 881,000 deaths in 2018 [1]. Although, the developed countries have higher estimates of CRC than the developing countries (Low and Medium income Countries) data show that there is a gradual increase of CRC new cases in middle income countries such as South Africa (SA) and Brazil (BR) with new cases in 2018 reported at 6 937 (6.5% of all cancer cases) and 59 783 (9.3% of all cancer cases) in SA and in BR respectively [2,3]. It is considered as a marker of socioeconomic development with the rising of incidence rates in tandem with increasing Human development index (HDI) [4-6]. In addition, there are associated risk factors for CRC reported including obesity, alcohol and tobacco usage, diabetes mellitus, poor nutrition and sedentary lifestyle [7-9].
In 2018, the CRC estimated age-standardized (World) incidence rates (ASIR) were estimated to be at 14.4 and 19.3 per 100 000 for SA and BR respectively. It is projected that by 2030, CRC new cases will increase by 46% and 39% in South Africa and Brazil respectively. The cumulative incidence rate of CRC is 0.54 and it is the top six leading cause of death in South Africa [1]. Colon and rectum cancer (called colorectal cancer) is the third most lethal type of cancer in women and the fourth in men in Brazil [10]. There are 3 508 affected males (7.3% of all cancer cases in males) and 3 429 affected females (5.7% of all cancer cases in females).
The CRC morbidity, globally, has affected the disability-adjusted life years (DALY) due to premature death from CRC and increased related medical costs of individuals living with CRC [11].
Considering the above, it is vitally important to have accurate population based national cancer registries that will enable the developing countries to accurately estimate the true incidence, prevalence and burden of CRC. The availability of high-quality, local data cannot be over-emphasised to improve the robustness of the estimates submitted by countries and will provide governments, particularly, in developing countries with the local data needed to prioritise and evaluate cancer control efforts [6]. Brazil, in most recent years has managed to develop a population based registry while South Africa is in the process, with the protocol for data collection been published in 2019 and the new CRC estimates expected to be published in 2020 [12]. These initiatives will reduce CRC uncertainty attributable to scarce data, partial cancer registries and inaccurate CRC research publications.
Furthermore, it is reported that CRC screening or diagnostic services are limited to certain geographical areas within countries, limiting access and screening to those at high risk based on their personal background. This selected approach neglects general screening that could reduce late presentation of new cases and add value only if supported by data to ensure the right people at right time are accurately targeted, as evidence has shown that early detection of CRC drastically reduces mortality and prolongs survival [13]. However, less is known regarding the yield of screening, and the burden at local level, as risks may vary by geography or type of screening offered. Moreover, despite significant advances in standard of care therapies, the 5-year survival rate for metastatic CRC, globally, remains around 12%. Immunotherapy has not provided the robust advances in CRC, unlike what has been achieved in other malignancies [6].
Currently, there are gaps in understanding CRC and prevention and treatment in South Africa. Most focus is on breast, lung, cervical cancer based on the top three causes of cancer related deaths. However policy and programmes have made great strides to highlight risk factors for all non-communicable diseases and have developed a health promotion to raise awareness of dangers of non-communicable diseases including cancer and the benefits of healthy lifestyles [9].
Studies have focused on diagnostics and treatment and less so on screening approaches, health promotion and validation of molecular classifications and clinical factors. Moreover, progress is slow with regard to the clinical translation and precision medicine to reduce the number of unsuccessful treatments of CRC patients and CRCrelated deaths [11]. This calls for greater focus on prevention and early detection as prevention is better than treatment, in particular, in developing countries where resources are limited.
Given this situation, this study attempts to compare the CRC burden in terms of the estimated CRC incidence, mortality and survival rate based on the GLOBOCAN data for South Africa and Brazil. In addition, the study compares the temporal trend and projections of these estimates over 10 years (2030) between the two countries that have economic cooperation to identify similarities, differences and lessons that could be learned through current partnership between the two countries in their effort to control CRC. Understanding the incidence, prevalence, survival and projections of CRC is imperative to inform policy, practice and future research [1].
Why measure the incidence, mortality and survival of CRC in South Africa (SA) and Brazil (BR)?
The World Health Organisation and United Joint Programme on AIDS had recognised BRICS as emerging economies that pose great potential to advance global health bringing new perspective and solutions to address health challenges (Harmer, 2013; WHO, 2011). The BRICS Health Ministers in 2011, declared to coordinate, cooperate and consult each other for collective action through south-to south partnerships on matters affecting global health (BRICS, 2011). Based on this cooperation, and the fact that each country has brought unique contributions to advance global health, comparing, health indicators among BRICS as new geo-economic and political bloc and highlighting opportunities for greater collective action becomes necessary for BRICS to advance and also influence global health.
We aimed to analyse CRC data from South Africa and Brazil, to benchmark, because:
• The two countries are both in the high middle income countries based on the World Bank socioeconomic status and economical ranking of countries.
• The countries are both members of BRICS group with economic cooperation including India, Russia and China.
• Both countries have undergone socio-political and economic transformation in the past 20 years affecting lifestyle and behavioural risks to CRC.
• Both countries have similar cancer data collection strategies to monitor morbidity and mortality trends.
• Have similar public health disease burden, communicable and non-communicable diseases as well as causes of deaths and morbidity.
• The current CRC burden is almost the same in both countries ASMR (SA=7.9% and BR=9%) per 100 000.
• It is estimated that by 2030, the CRC new cases will increase by 46% and 39% in South Africa and Brazil respectively.
Methods
The study analysed and compared the burden of CRC between South Africa and Brazil, based on latest WHO global cancer estimates. Detailed descriptions of the methodology and approach used to analyse data published in GLOBOCAN 2018 have been published elsewhere [1,6,10].
Sources of cancer data
Data was extracted from the GLOBOCAN 2012 -2018 on CRC incidence, prevalence, and mortality pertaining South Africa and Brazil. The estimates come from the analysis of CRC mortality estimates from national cancer registries, that are either population based as in the case of Brazil or pathology based as is the case in South Africa [1,8] as reported in the Global Burden of Cancer Study 2018 report.
Statistical analysis
In this study, absolute numbers of deaths, the mortality rates, new cases, incidence, 5 year prevalence and proportions and ratios were extracted and compared between two countries. Data on the incidence age-standardized rate (ASR; per 100,000 person-years), 5-year prevalence of cancers (proportion per 100,000), as well as the ASR and cumulative risk (%, age 0-74) of cancer mortality were extracted from the report. The ASRs and 5-year prevalence of cancers are presented for men and women of South Africa and Brazil countries, respectively. The use of females to male ratios was also extracted to identify gender variations from the report.
The ASIR conversions were reported to have been based on world population net 2014. Annual trends in CRC are based on the GLOBOCAN data and were evaluated by the annual percentage change (APC) over time period as: [exp (β) -1] ×100), as reported in the Global Burden of Cancer Study 2018 report. Colorectal cancer survival was calculated using a mortality-incidence ratio (MIR), based on scaling factor and projections of 10-year prevalence of each country and were calculated and reported as MIR. All data extracted was entered in Microsoft excel 2015 for comparison [1].
Ethical approval and consent of the study was provided by the Ethical Medical Review Committee of the University of Antwerp in April 2020 [No. EC 20/11/127].
Results
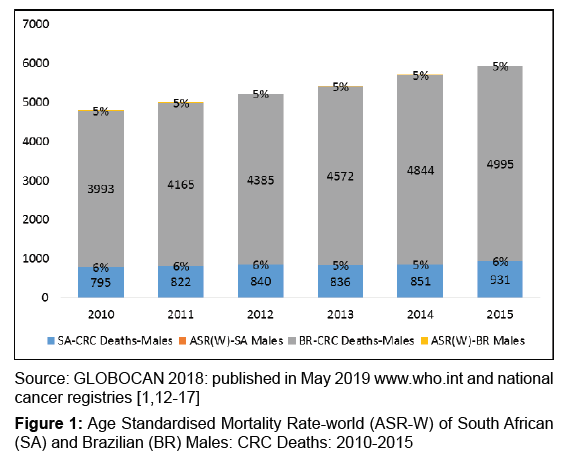
An upward trend in CRC mortality cases is observed in both countries from 2010 to 2015 in Figure 1. There is 25% increase in mortality among males with CRC in Brazil from 3 993 in 2010 to 4 995 in 2015. The increase is also observed in South Africa, with 795 mortality cases in 2010 and 931 cases in 2015, showing a 17% increase between the six year periods [1,12-17].
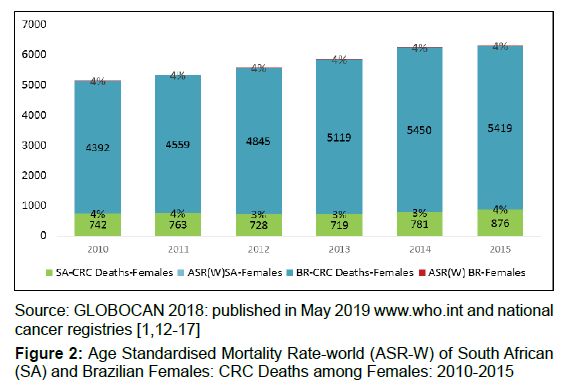
There were 4392 (44.7%) CRC related deaths recorded in 2010 among the Brazilian females and 5 419 in 2015, a 23% increase between the six year period, depicted in Figure 2. There were 742 CRC related deaths recorded in 2010 among South African females and 876 in 2015, an 18% increase between the six year periods. The age-standardised mortality rate of CRC in 2015 was 1.2 times higher among Brazilian males compared to females in 2015 (4.91 and 3.96 per 100,000, respectively).
The age-standardised mortality rate of CRC in 2015 was 1.5 times higher among South African males compared to females in 2015 (5.59 and 3.69 per 100,000, respectively). By 2018 as tabulated in Table 1 below, the recorded mortality cases were 2 498 with a crude rate of 0.54 and 15 344 with crude rate of 0.60 in South Africa and Brazil respectively. The age-standardised mortality rate of CRC has increased in both sexes an all ages in both countries to 7.6 and 9.0 per 10 000 respectively. Colorectal cancer prevalence is 15.7/100,000 and 31.4/100,000 in South Africa and Brazil, respectively.
| Country | ||
|---|---|---|
| Colorectal Cancer Burden | South Africa | Brazil |
| Mortality Cases in 2018 (per 100 000) | 2 498 | 15 344 |
| Crude Mortality Rate | 0.54 | 0.6 |
| CRC Mortality Rank in cancer deaths | 6 | 4 |
| Age-standardized (World) mortality | 7.6 | 9 |
| 5-year prevalence (all ages) | 9 031 | 66 182 |
| 5-year prevalence proportion (all ages) | 15.73/100 000 | 31.39/100 000 |
Table 1: Colorectal Cancer mortality and survival in South Africa and Brazil 2018.
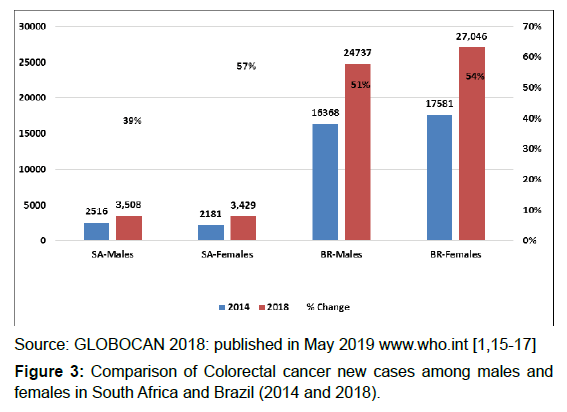
When comparing the CRC new cases between 2014 and 2018, the Figure 3 depicts that there are more CRC new cases in Brazil than in South Africa. However, the CRC new cases have increased more than half among males in Brazil and more than a third among males in South Africa. The CRC new cases in females have increased by 54% in Brazil and by 57% in South Africa within four years.
The Table 2 shows both CRC new cases by country and the agestandardised incidence rate of CRC per 100,000.
| New Cases and Age-standardised incidence rate in 2018 | Both Sexes | Males | Females | Ratio between Gender |
|---|---|---|---|---|
| South Africa CRC New Cases (percentage of all cancer cases) | 6 937 (6.5%) | 3 508 (7.3%) | 3 429 (5.7%) | |
| Age-standardized (World) incidence rates per 100 000 | 14.4 | 7.3 | 7.1 | 1.02 |
| Southern Africa UN Region* CRC incidence rate per 100 000 | 13.4 | 16.8 | 11.28 | |
| Brazil CRC New Cases (percentage of all cancer cases) | 51 783 (9.3%) | 24 737 (8.9%) | 27 046 (9.6%) | |
| Age-standardized incidence rates per 100 000 (Globally) | 19.6 | 9.5 | 10.2 | 1.07 |
| South America UN Region** CRC incidence rate per 100 000 | 18.6 | 20.6 | 17.1 |
Source: GLOBOCAN 2018: published in May 2019 www.who.int [1]
* Southern Africa Region: United Nations Region definition [https://gco.iarc.fr/today/data/factsheets/populations/991-who-africa-region-afro-fact-sheets.pdf]
** South America Region: United Nations Region definition [https://gco.iarc.fr/today/data/factsheets/populations/931-south-america-fact-sheets.pdf]
Table 2: The age-standardized incidence rate of CRC per 100,000 in 2018 by country.
The age-standardised incidence rate was higher in Brazil (19.6 per 100,000) compared to South Africa (14.4 per 100,000). However, the Brazilian women had a higher CRC incidence rate than Brazilian men (10.2 and 9.5 per 100,000, respectively). Overall, Brazil (19.6 versus 18. 6 per 100,000) and South Africa (14.4 versus 13.4 per 100 000) have higher incidence rates than their regional age standardised incidence rate estimates [1,15-17].
The CRC new cases in SA were 6.5% of all cancer cases compared to 9.3% in BR, showing a 2% higher rate than SA.
Gender variation of new cases were also noted, with CRC about 1.1 times higher in males than in females in South Africa, while in Brazil, the women had about 1.07 times higher new CRC cases.
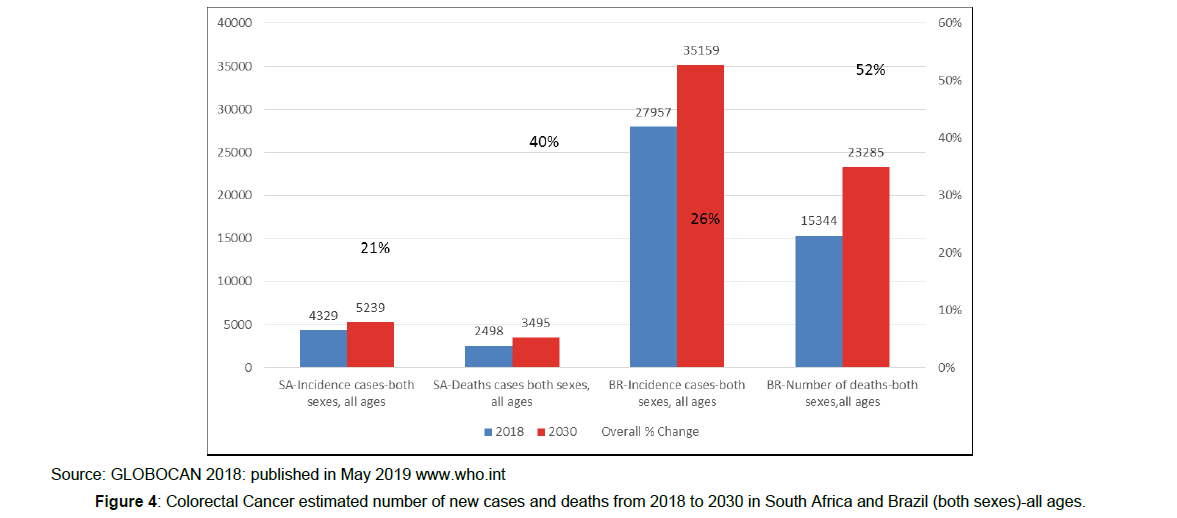
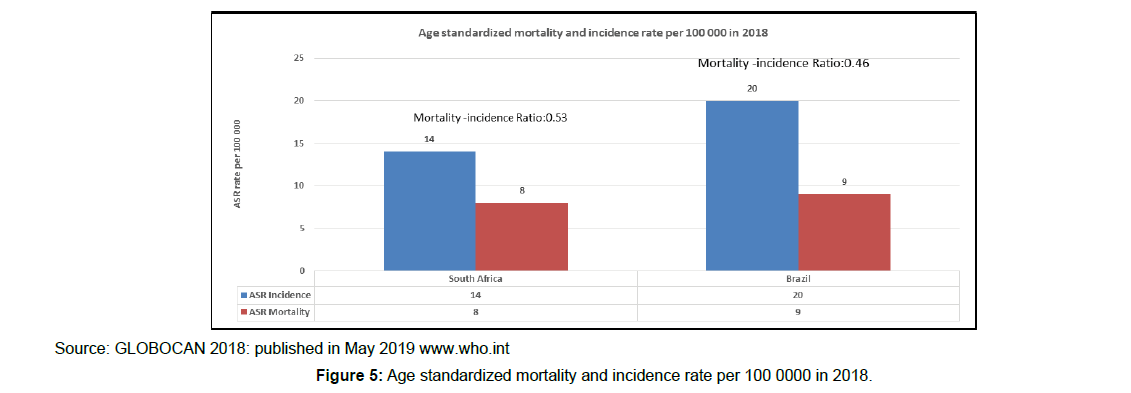
As indicated in Figure 4, in both counties the APC is more than a third in both countries, with MIR at 1.76. The estimated number of new cases will increase by 46% (27 957 in 2018 to 40 866 in 2030) and 39% (4 329 in 2018 to 6 012 in 2030) in South Africa and Brazil respectively and the estimated number of deaths will increase by 52% (15 344 in 2018 to 23 285 in 2030) and 40% (2 498 in 2018 and 3 495 in 2030) in South Africa and Brazil, respectively. South Africa mortalityincidence ratio is 0.53 and Brazil is 0.46, reflecting the survival rates in each country, as depicted in Figure 5 above.
Discussion
Using data from GLOBOCAN (2010-2018), we highlighted two countries of interests and compared the CRC burden. . There are noticeable differences in the incidence, mortality and survival rates in South Africa and Brazil. Noting Figure 1 and 2, Brazil has a higher mortality rate than South Africa. However, the ASR among men is higher in South African men than in Brazilian men. Females in both countries have similar mortality ASR. The main finding of this study was that in Brazil as in South Africa CRC age standardised incidence rates, in 2018 were higher than the overall regional rates.
The comparisons and differences observed in the two countries match global literature that reports the striking differences in CRC mortality and incidence between developed and developing countries. Globally, CRC incidence rate is projected to increase by around 40% over the next 12 years (from 2018 to 2030), and South Africa and Brazil have similar projections [1,6,11].
There are considerable differences in the incidence and mortality of CRC among South Africans and Brazilians. Despite geographical variation, similar findings have been observed elsewhere that the agestandardised incidence of CRC is usually higher in males than females, as shown by the data from South Africa. The minimum estimated difference in the rate of CRC was observed amongst men from South Africa and Brazil (4.9 and 5.5 per 100,000 respectively). Similarly, for females, minor differences in the rate of CRC were observed with 3.96 and 3.69 per 100,000 in Brazilian and South African females, respectively [10,18].
Brazilian females are at higher risk of CRC than males, compelling that the CRC control programmes be tailored to the high risks groups by gender in each country. It has been reported that the southern and south-eastern regions have a profile closer to that of developed countries. To monitor the trends accurately, this calls for better profiling of the population and monitor the geographic variations including epidemiological and nutritional transition [14,19] as well as quality of life’s standards. In addition, it will be important to consider socioeconomic status as well as ethnicity including ancestral traits within and between the regions that could predispose certain population to CRC in South Africa and Brazil. Cronje in the study published in 2009 reported that in South Africa, CRC affects people of Caucasian and African descent. Therefore, prioritising CRC screening among these two groups cannot be overemphasised. The study by de Oliveira, 2018 reported that the South, South East and Midwestern regions in Brazil have higher CRC incidence, affecting younger population with African ancestry confirming similar observations among people with African descent in South Africa and Unites States of America. Consequently, calling for ethinical and regional targeting of CRC screening campaigns [20,21].
Literature attributes lower CRC new cases among females to existence of reproductive hormones that could be protective against CRC through changes in bile synthesis and secretion resulting in lower bile acids in the colon [16, 17]. However, Brazil seems to negate this assertion as the age-standardised incidence of CRC is much higher among females than males. It has been documented that there are regional inequalities in Brazil and these are more pronounced among women, and could explain the rising CRC ASR among females compared to males [18].
Mortality and incidence of CRC is also influenced by the screening patterns, time of diagnosis, with early diagnosis prolonging survival, while late diagnosis drastically reduces survival to less than 20%, as shown by literature [22,23]. WHO non-communicable disease (NCD) plan advocates for population-based CRC screening, including using a faecal occult blood test as appropriate at age >50, linked with timely treatment [24]. However, this measure, is not yet implemented in Brazil nor in South Africa.
Nearly a third (29?) of CRC cases survive in Brazil and less so in South Africa (15%). Survival is influenced by a number of factors including medical advances, universal health care coverage, quality of services, equity in service provision, integrated package of services and, existence of laboratories and trained human resources. Furthermore, it has been found that where there are evidence based national cancer policies that address all stages of care, including awareness-raising, prevention, diagnosis, treatment, rehabilitation and palliative care, there tend to be better surveillance and control programmes [19,25- 27].
Survivorship in both countries is also influenced by existence of after cancer care services. Moreover, it is reported that the stage at which CRC is diagnosed is critical as later-stage diagnosis is reported to have poorer outcomes [19,26]. It has been also reported that the five-year survival rate is 90 per cent for CRC diagnosed at an early stage compared with 13 per cent for those diagnosed at a late stage. Noting the survival rate in South Africa, it could be explained by late presentation, which reflects on the status of screening and control programmes in the country, although Brazil is also not better off in this regard.
While survivorship is promising for CRC, a full understanding of what it will take for each country to achieve survival rate similar to developed countries is yet to be explored. The first step towards this discussion could be propelled by collection of well-structured population-based cancer registry data and data on cancer survivors’ needs [28].Together, these data could inform integrated care to cancer survivors and assist to better structure work place occupational health services, given the steady rise of the number of cancer survivors in South Africa and Brazil that could be part of the workforce [29,30].
Thus far, Brazil is ahead of South Africa on collecting the population based registries and South Africa can learn more from Brazil on the set-up and management thereof. The CRC mortality rate mirrors high income countries and is attributed to the changing socio-economic status and lifestyles that mirror the Western cultures reflected by changes in diet, physical activities and behavioural patterns such as alcohol and tobacco consumption and use [7]. In addition, this increase in both incidence and mortality rates impact on economic burden and poor CRC control programmes in both countries, putting high pressure on the already overwhelmed health system [30-32]. Unfortunately, this upward trajectory is expected in 2030 affecting both countries [33].
The overall CRC M/I ratio is an indirect measure of cancer survival and is calculated by dividing the mortality rate by incidence rate. Among the two countries, the M/I ratio is higher in South Africa than in Brazil, reflecting better CRC support and care (0.53 and 0.46 respectively). However, South Africa presents worse quality of life indicators than Brazil, hence within-country differences need to be considered as well as general indicators might not always show inequities that may exist within countries. This calls for intensified health promotion and screening programmes to ensure early detection and treatment to reduce mortality [34,35].
Therefore, the policy makers and programme managers need to consider CRC prevention interventions and there are opportunities for sharing of lessons and resources in both countries noting the current economic partnership. Health education and targeted CRC screening programmes among people at high risk, integrated with other noncommunicable diseases for sustainability will be essential to improve CRC disease control in both South Africa and Brazil [27,32,34].
South Africa has improved population health over the past 15 years despite high HIV prevalence. The presence of HIV treatment has sustained high prevalence rate and extended life expectancy of South Africans. With the growing ageing population and risk factors as a result of westernisation, there is increasing NCD burden, and rising costs of care [31,32,34].
Even though South Africa has good policies and plans focusing on NCDs to address and reduce risk factors for chronic diseases, strengthen prevention, and promote health promotion, South Africa’s challenge of growing health inequalities remains.
Hence, the distribution of health resources and services must strive to achieve CRC prevention and control coverage and efficiently address changing geographic-specific CRC burden. Furthermore, surveillance is essential to inform policy and advocating for support in areas demanding greater investments [17,23,24,27,34].
Strengths and limitations
The strength of this study was to work with incidence, mortality and survival estimates using the GLOBOCAN 2018 database to compare CRC between South Africa and Brazil.
However, there are limitations due to limited access to data, analysis by region was excluded, a major gap worth noting is that both South Africa and Brazil are countries with diverse population and cultures. Hence, it is important to analyse the incidence and mortality rate of CRC among main cultures or ethnicities within each country to inform priority interventions for each group and better understanding of genetic factors that influence aetiology of CRC among different ethnicities [30]. Moreover, age specific data need to be available to also inform optimal age for CRC screening.
Sparse data at the regional level is the biggest challenge for risk factor and mortality estimation. Furthermore, lack of data that specifies the site of the tumour in the colon (proximal, distal, or other) hinders the analysis and comparison of tumour sites to CRC incidence and mortality as done in other studies [32]. The lack of a harmonised system to connect different CRC data sources has impeded the comprehensive comparison between countries and within regional variability. Lack of stratification by region and age is another limitation. Advocacy on accurate, broad based data collection is needed to complete the picture of CRC burden and outcomes in South Africa and Brazil.
Another limitation on the incidence data is the cross sectional nature of measure hence, data from other points in time and changes in incidence trends are not considered. In addition, time factors also affect accuracy in that it does not assist a study to explain when, where and how target population is most at risk and is limited to define how the impact and extent of migration into and out of specific areas affects the incidence rate. All this affects the types of interventions that are necessary and appropriate for early detection and CRC control [31,34,36-38].
Conclusion
This analysis, as far as we know first of its kind, provides the most comprehensive comparison of two countries that are part of the emerging economics partnerships called, BRICS. This study highlights increasing CRC burden in both countries and identifies challenges, gaps and opportunities for collaboration between the two countries to improve CRC health outcomes and protect gains achieved by prevention and health promotion interventions. While the CRC incidence and mortality rates have increased, survival is also increasing gradually due to substantial improvement in screening and treatment and control interventions since 2010 GLOBOCAN data.
Increased CRC ASIR among Brazilian women and lower survival rate in South Africa highlights changeless inconsistency and inequity in service delivery across the geographical regions of the country. At national level, while the standard of living increases in both countries, so as the burden of non-communicable diseases and risk factors. Health Promotion interventions that increase demand for physical activity, reducing risky behaviour by rewarding healthy lifestyles and increasing accessible preventive tests for CRC for the whole population are necessary in both countries.
These data provides an opportunity for both countries to explore collaboration and offers opportunities for policy makers to target specific interventions that can improve survival rates and lower ASIR and morality rates by regions in the two countries. Furthermore, this comparative data creates opportunities for each country to share and learn from those regions where health gains have been made. The importance of combination of data sources cannot be emphasised, in spite of noting some of the limitations of the GLOBOCAN data. Surveillance through population based registries, behavioural surveys and routine health data are key components for effective and robust policy and efficient planning of cancer control. Hence, opportunities for collaboration exists in policy development, programme planning and implementation in monitoring and evaluation as well as future research through the economic partnership of the two countries.
What this study adds
• Our study compared CRC burden in two countries which are currently enjoying economic cooperation as part of the BRICS; there are currently no published comparisons on CRC burden, and to the best of our knowledge within BRICS.
• Our comparative data supports the notion of exploring policy to develop colorectal screening guidelines informed by regional data within countries and advocates for south –tosouth partnerships in CRC burden monitoring and screening for prevention, early detection and management to improve clinical outcomes
• Our data advocate for and highlight the importance for further research to understand the trends in the two countries through collaboration;
• Calls for the two countries to identify opportunities for innovations covering the whole spectrum of care i.e. screening tools to survivorship care.
References
- Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. (2017) Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 3(4): 524–548.
- United Nations Development Programme (2016) Human Development Report 2016: Human Development for Everyone. New York, NY: United Nations Development Programme.
- Bray F (2014) Transitions in human development and the global cancer burden. In: Stewart BW, Wild CP, eds. World Cancer Report 2014. Lyon: IARC Press 42-55.
- Fidler MM, Soerjomataram I, Bray F (2016) A global view on cancer incidence and national levels of the Human Development Index. Int J Cancer 139: 2436-2446.
- Silva DAS, Tremblay MS , Marinho de Souza M De F , Mooney M , Naghavi M , et al. (2018) Mortality and years of life lost by colorectal cancer attributable to physical inactivity in Brazil (1990–2015): Findings from the Global Burden of Disease Study.
- Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, et al. (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66: 683-691.
- World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) (2018) Continuous Update Project Report: Diet, Nutrition, Physical Activity and Colorectal Cancer 2016. Revised 2018. London: World Cancer Research Fund International.
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, et al. (2015) Cancer incidence and mortality - major patterns in GLOBOCAN 2012, worldwide and Georgia. Int J Cancer 136: E359–86.
- Cancer Association of South Africa (2012) National Cancer Registry. http://www.cansa.org.za/ files/2017/03/SA-National-Cancer-Registry-2012-web-Feb-2017.pdf (accessed December 28 2019) with South African National Cancer Registry. Cancer in South Africa (2010). Cited Oct 25 2018.
- Malta DC, Felisbino-Mendes MS, Machado ÃE, Passos VMA, Abreu DMX, et al. (2017) Risk factors related to the global burden of disease in Brazil and its Federated Units, 2015. Rev Bras Epidemiol 20(Suppl 01): 217–232.
- Global Burden of Disease Mortality and Causes of Death Collaborators, Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, et al. (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053): 1459–1544.
- South African National Cancer Registry. Cancer in South Africa (2011). Cited Oct 25 2018.
- South African National Cancer Registry. Cancer in South Africa (2012). Cited Oct 25 2018.
- South African National Cancer Registry. Cancer in South Africa (2013). Cited Oct 25 2018.
- McCabe M, Perner Y, Magobo R, Mirza S, Penny C (2019) South African National Cancer Registry. Cancer in South Africa (2014). Descriptive epidemiological study of South African colorectal cancer patients at a Johannesburg Hospital Academic institution (Cited Oct 25 2018). JGH Open 4(3): 360-367.
- Souza DL, Jerez-Roig J, Cabral FJ, de Lima JR, Rutalira MK, et al. (2014) Colorectal cancer mortality in Brazil: predictions until the year 2025 and cancer control implications. Dis Colon Rectum 57(9): 1082-9.
- Stopa SR, Malta DC, Monteiro CN, Szwarcwald CL, Goldbaum M, et al. (2017) Use of and access to health services in Brazil, 2013 National Health Survey. Rev Saude Publica 51(suppl 1): 3s.
- Fuchs CS, Giovannucci EL, Colditz GA, Hunter DJ, Speizer FE, et al. (1994) A prospective study of family history and the risk of colorectal cancer. N Engl J Med 331: 1669-1674.
- Cancer Incidence in Brazil Estimativa 2018: Incidência de Câncer no Brasil Estimación 2018: Incidencia de Cáncer en Brasil Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2018: incidência de câncer no Brasil. Rio de Janeiro: INCA, 2017. 128 p. ISBN 978-85-7318-362-7 (printed version) ISBN 978-85-7318-361-0 (electronic version).
- Cronjé L, Paterson AC, Becker PJ (2009) Colorectal cancer in South Africa: a heritable cause suspected in many young black patients. S Afr Med J 99: 103–6.
- de OliveiraI MM, Dias de Oliveira Latorre MDR, Tanaka LF, Ross BM, Curado MP (2018) Disparities in colorectal cancer mortality across Brazilian States. Rev Bras Epidemiol 21 :e180012.
- Connell LC, Mota JM, Braghiroli MI, Hoff PM (2017) The rising incidence of younger patients with colorectal cancer: questions about screening, biology, and treatment. Curr Treat Options Oncol 18(4): 23.
- Siegel R, Desantis C, Jemal A (2017) Colorectal cancer statistics, 2014. CA Cancer J Clin 64(2): 104-17.
- Geneva: World Health Organization (2013) Global Action Plan for the Prevention and Control of NCDs 2013–2020.
- Anderson JC, Shaw RD (2014) Update on colon cancer screening: recent advances and observations in colorectal cancer screening. Curr Gastroenterol Rep 16: 403.
- Guerra MR, Bustamante-Teixeira MT, Corrêa CSL, Abreu DMX, Curado MP, et al. (2017) Magnitude and variation of the burden of cancer mortality in Brazil and Federation Units, 1990 and 2015. Rev Bras Epidemiol 20(Suppl 01): 102–115.
- The National Strategic Cancer Framework 2017-2022. The National Department of Health, Republic of South Africa, Pretoria, 2017.
- Graham A, Adeloye D, Grant L, Theodoratou E, Campbell H (2012) Estimating the incidence of colorectal cancer in Sub–Saharan Africa: A systematic analysis. J Glob Health 2(2): 020404.
- Souza DLB, Jerez-Roig J, Cabral FJ, Roberto F de Lima J, et al. (2014) The Economist Intelligence Unit: The challenges of providing integrated care for cancer survivors, Colorectal cancer mortality in Brazil: predictions until the year 2025 and cancer control implications. Dis Colon Rectum 57(9): 1082-9.
- Brand M, Gaylard P, Ramos J (2018) Colorectal cancer in South Africa: An assessment of disease presentation, treatment pathways and 5-year survival. S Afr Med J 108(2): 118-122.
- Stintzing S (2014) Management of colorectal cancer. F1000Prime Rep 6: 108.
- International Agency for Research on Cancer (2018) GLOBOCAN 2018: Estimated cancer incidence, mortality and prevalence worldwide in 2012-2018 (accessed 16 January 2020).
- Schreuders EH, Ruco A, Rabeneck L, Schoen RE, Sung JJY, et al. (2015) Colorectal cancer screening: a global overview of existing programmes. Gut 64: 1637-1649.
- Thun MJ, Wild CP, Colditz G. Framework for understanding cancer prevention. In: Thun MJ, Linet MS, Cerhan JR, Haiman CA, Schottenfeld D (2018) Cancer Epidemiology and Prevention. 4th ed. New York: Oxford University Press 1193-1204.
- Geneva: WHO World Health Organization (2012). Cancer: Fact Sheet no. 297.
- International Agency for Research on Cancer. GLOBOCAN 2008. Lyon, France: IARC, 2010.
Citation: Magwaza S, Hal G, Hoque M (2020) Comparison of Colorectal Cancer Burden: Opportunity for Sharing Lessons and Expand Partnership in Health Care in Two BRICS Countries. J Gastrointest Dig Syst 10: 626. DOI: 10.4172/2161-069X.1000626
Copyright: © 2020 Magwaza S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3345
- [From(publication date): 0-2020 - Nov 23, 2025]
- Breakdown by view type
- HTML page views: 2458
- PDF downloads: 887