Comparison of Quality of Life after Mandibular Resection: A Cohort Study of Patients in the Same Institution
Received: 04-Feb-2016 / Accepted Date: 22-Apr-2016 / Published Date: 25-Apr-2016 DOI: 10.4172/2161-0681.1000271
Abstract
Objective: The surgical treatment of benign locally invasive lesions of the mandible can have deleterious effects on a patient’s quality of life (QOL). To evaluate and compare the QOL in two cohort groups of patients who underwent mandibular resection for benign locally invasive lesions of the mandible. Methods: This was a seven year prospective study using the modified University of Washington Quality of life (UW-QOL) Questionnaire, version 4. The two cohorts studied were those that were rehabilitated, and those not rehabilitated. The questionnaire was administered to the patients at 18 months after marginal mandibular and segmental mandibular resections respectively. Statistical analysis was performed using EPI INFO 7 software package and level of significance was set at p<0.05. Results: This showed that 71/87 subjects who had resections responded; 34 marginal mandibular, and 37 segmental mandibular were studied. The socio-demographic variables presented no statistically significant relationship regardless of the status of rehabilitation. Most patients without rehabilitation had a lower QOL score for functional daily activities like chewing, speech and psychological effects of low mood and anxiety compared with the rehabilitated group; and that socio-economic class of the patients was the best predictor of better QOL. Conclusion: The major concerns of patients who have undergone mandibular resection were chewing ability, speech, appearance, anxiety and low mood, and these concerns were expressed more in the non-rehabilitated. The trends and determinant of QOL observed should be used to decide targeted support in order to assist the patients overcome their deformities and disabilities.
Keywords: Mandibular resection; Quality of life; Cohort study; Outcome assessment
313254Introduction
The existing literature shows that the eradication of many pathological processes involving the jaws particularly the mandible has led to facial deformity and functional impairment [1,2]. Consequently, the surgical treatment of benign locally invasive lesions of the mandible can have deleterious effects on a patient’s quality of life (QOL), and these may include aesthetics, functional and psychological issues among others [3,4]. This is because mandibular resection secondary to neoplastic aetiology can cause extensive composite defects which leads to dramatic loss in quality of life [5,6]. Most of the affected patients manage to cope with these disabilities even after secondary procedures to restore anatomy and function of the lost tissues [7]. Thus, the role of the mouth and teeth in patient’s daily life should be put in perspective in order to appreciate the consequences of these disease conditions and the adverse effects of the surgical procedures employed to eliminate them.
Research to determine how health problems influence life quality, disability, impairment and function suggest that the presence or absence of health complaints alone is an insufficient reason for subjective health status evaluation [8]. This is also consequent upon the assumption that poor health means poor quality of life while on the contrary many people with chronic disabling disorders rate their quality of life higher than the healthy [8,9]. QOL is a measure that reflects many of these variables and can be used as an outcome criterion, along with such factors like mortality, morbidity, survival and recurrence [9]. QOL is a patients’ appraisal of, and satisfaction with their current level of functioning compared with a perceived or expected ideal [10]. QOL has been longitudinally followed in patients’ with oral and pharyngeal squamous cell carcinoma as a function of time and tumour stage, [11] site of lesion, patient demographics and method of reconstruction or rehabilitation [12]. This has helped researchers to identify the clinical determinants of QOL, time course and magnitude of recovery from disease process [13].
Since the perception of QOL has a subjective component and could vary from one locality to another, obtaining baseline information from patients who have undergone ablative surgeries in the mandible is important for researchers and healthcare planners in a particular environment [8]. This is particularly important in our environment where most of these patients who have undergone these surgeries are abandoned to their fate with its attendant adverse consequences. The present study prospectively evaluated and compared the QOL in two different cohorts of patients who underwent mandibular resection for benign locally invasive lesions of the mandible using the University of Washington’s Quality of life Questionnaire (UW-QOL), version 4 as modified by Young et al. [3] over a period of seven years.
Methods
This prospective study was done between January 2008 and December 2014. Ethical approval was obtained from the Research Ethics Committee of the institution, and the study was done in accordance with the Helsinki Declaration of 1975, as revised in 2000 after obtaining informed consent from the subjects. A total of 71/87 subjects who had undergone mandibular resection (34 marginal mandibular resection, 37 segmental mandibular resection) for benign locally invasive mandibular lesions at our institution through intra-oral approach were studied prospectively by personal interview, using University of Washington’s Quality of life Questionnaire (UW-QOL), version 4 as modified by Young et al. [3]. The 71 patients were those that responded to the questionnaire while the rest did not respond. This study did not include all consecutive patients earlier treated in this institution as some of the subjects could not be reached or contacted at 18 months post-surgery when the questionnaire was administered to those studied them.
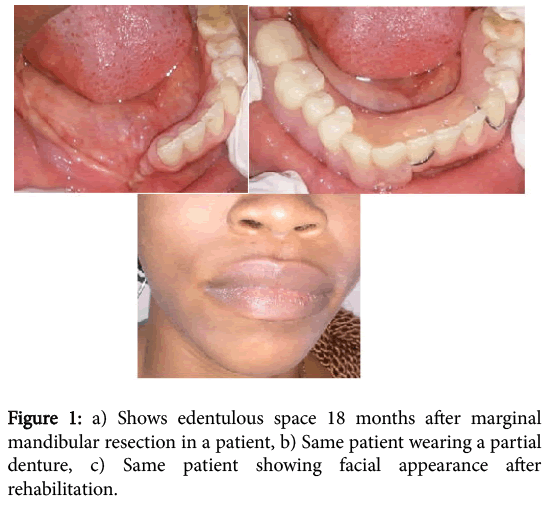
The modification of the questionnaire was done such that the word cancer was replaced with the words mandibular resection in the mood, anxiety, and global domains. This module containing items exploring side effects and symptoms of treatment have three sections with 16 items. This questionnaire is validated and has been shown to adhere to internal consistency, is reliable and has domains that are specific to head and neck pathology [3] (Figure 1).
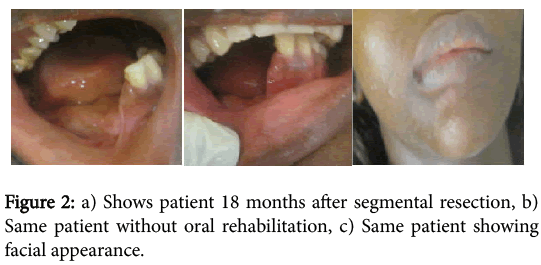
The patients 71 included in the study were in two categories. 1]. Control Marginal group: Those that had marginal mandibular resection and were rehabilitated 12 months after surgery with partial denture prosthesis to replace lost dentition only at the site of resection as the remaining rim of bone was adequate to support the partial denture prosthesis. 2]. Experimental Segmental with no reconstruction group: Those that were treated by segmental mandibular resection, and later rehabilitated only by inter-maxillary fixation to prevent the collapse of the remaining bone segments. The inter-maxillary fixation was done one week after surgery and was left in-situ for six weeks. For these patients no further treatment at the site of resection was done to provide reconstruction plate or bone grafting and dental prosthesis to correct the bone discontinuity defect and replacement of lost dentition.
Other data collected in the two groups were age, gender, socioeconomic status, type/site of lesion, size of healed wound, and reason(s) for no rehabilitation in the experimental segmental with no reconstruction group. Patients’ socio-economic status was classified using Adedeji’s [14] classifications of 1985 (Figure 2).
Also, not all the patients contacted in the two groups responded to the questionnaire; six in the control marginal group and 10 in the experimental segmental with no reconstruction did not respond. To avoid a possible selection bias some characteristics of the responders and non-responders were compared. Student’s t-test and Fisher’s exact tests did not show statistically significant differences (data not shown; p>0.05) between non-responders and responders, so it was assumed that the participants in the study are representative of the total patients in the two cohorts. All other statistical analyses were performed using EPI INFO 7, version 0.2.0, 2012 software package (CDC, Atlanta, GA, USA) and level of significance was set at p<0.05.
Results
This showed that 71/87 subjects who had undergone mandibular resection (34 marginal mandibular, 37 segmental mandibular) for benign locally invasive mandibular lesions through intra-oral approach responded to the questionnaire and were studied. The study revealed that in the rehabilitated (control) group, the age of subjects ranged from 18-55 years with mean at 35.0 ± 9.6 years, while in those that were not rehabilitated (experimental), the age range was 18-56 years and mean 34.2 ± 8.5 years (Table 1).
| Variable | Patients with partial denture rehabilitation ( n=34) | Patients without partial denture rehabilitation(n=37) |
|---|---|---|
| Frequency (%) | Frequency (%) | |
| Age | ||
| 11-20 years | 3(8.8) | 2(5.4) |
| 21-30 years | 8(23.5) | 11(29.7) |
| 31-40 years | 12(35.3) | 15(40.5) |
| 41-50 years | 9(26.5) | 8(21.6) |
| 51-60 years | 2(5.9) | 1(2.7) |
| Total | 34(100.0) | 37(100.0) |
| Sex | ||
| Male | 21(61.8) | 22(59.5) |
| Female | 13(38.2) | 15(40.5) |
| Total | 34(100.0) | 37(100.0) |
| Socioeconomic status | ||
| Class 1 | 2(5.9) | 0(0.0) |
| Class 2 | 13(38.2) | 0(0.0) |
| Class 3 | 9(26.5) | 6(16.2) |
| Class 4 | 8(23.5) | 24(64.9) |
| Class 5 | 2(5.9) | 7(18.9) |
| Total | 34(100.0) | 37(100.0) |
Table 1: Socio-demographic characteristics of patients.
Majority (n=51, 71.8%) of the subjects in the two groups were in the 2nd-4th decade of life. There were relatively similar numbers of male to male and female to female in the two categories; however, when the two groups are combined, the male: female ratio is 1.5:1 (Table 1). Majority (n=31, 83.8%) of those that were not rehabilitated (experimental group) were in the lower socio-economic class while those (n=22, 64.7%) that were rehabilitated were in the higher class. The socio-demographic variables presented no statistically significant relationship as P-values were >0.05 regardless of the status of rehabilitation.
The distribution of the types of lesion and sites of resected mandible are also shown (Table 2).
| Types | Rehabilitated Frequency (%) | Not rehabilitated Frequency (%) | |
|---|---|---|---|
| Ameloblastoma | 7 (20.6) | 15 (40.6) | |
| Ossifying fibroma | 9 (26.5) | 4 (10.8) | |
| Odontogenic fibromyxoma | 3 (8.8) | 5 (13.5) | |
| Cementoblastoma | 4 (11.8) | - | |
| Complex odontoma | 4 (11.8) | - | |
| Ameloblasticfibroodontoma | - | 4 (10.8) | |
| Odontogenic fibroma | - | 4 (10.8) | |
| Central giant cell granuloma | 3 (8.8) | - | |
| Calcifying epithelial odontogenic tumour | 2 (5.9) | 1 (2.7) | |
| Odontogenic keratocyst | - | 2 (5.4) | |
| Ameloblastic fibroma | - | 2 (5.4) | |
| Adenomatoid odontogenic tumour | 1(2.9) | - | |
| Compound odontoma | 1 (2.9) | - | |
| Total | 34 (100.0) | 37 (100.0) | |
| Site | |||
| Lateral/posterior | 13 (38.3) | 11 (29.7) | |
| Lateral/central | 8 (23.5) | 12 (32.4) | |
| Posterior | 7 (20.6) | 7 (19.0) | |
| Central | 3 (8.8) | 5 (13.5) | |
| Lateral | 3 (8.8) | 2 (5.4) | |
| Total | 34 (100.0) | 37 (100.0) | |
Table 2: Types of lesions and sites of the resected mandible in both groups.
These conditions were all locally invasive lesions. All the subjects in the two groups became partially edentulous following the resection. For the rehabilitated group, the healed wound size ranged from 5.8-12.3 cm with mean at 8.6 ± 2.0 cm while in those that were not rehabilitated the size ranged from 6.9-12.7 cm and mean, 8.6 ± 1.3 cm. Majority of the resections were done in the lateral/posterior (n=24, 68.0%) and lateral/central (n=20, 55.9%) parts of the mandible. There was no significant (P=0.24) relationship between the size of the healed wound and site of the resected mandible when the two cohorts of patients are compared.
NB: Central=symphysis, lateral=parasymphysis, posterior=body, angle, ramus, condyles.
QOL calculated for patients with partial denture rehabilitation showed good mean and best scores for shoulder, pain, activity and recreation, while anxiety and appearance had the lowest UW-QOL scores (Table 3). Taste, chewing, mood and speech were not adversely affected, but best QOL was not attained by most patients.
| Variable | 0 | 25 | 30 | 50 | 70 | 75 | 100 | Mean | % Best Score of 100 |
|---|---|---|---|---|---|---|---|---|---|
| Pain | 1 | 33 | 99 | 97 | |||||
| Appearance | 15 | 18 | 1 | 65 | 3 | ||||
| Activity | 10 | 24 | 93 | 71 | |||||
| Recreation | 1 | 9 | 24 | 92 | 71 | ||||
| Swallowing | 1 | 33 | 99 | 97 | |||||
| Chewing | 15 | 19 | 78 | 56 | |||||
| Speech | 25 | 9 | 78 | 27 | |||||
| Shoulder | 34 | 100 | 100 | ||||||
| Taste | 2 | 17 | 15 | 81 | 44 | ||||
| Saliva | 12 | 22 | 89 | 65 | |||||
| Mood | 7 | 24 | 3 | 72 | 9 | ||||
| Anxiety | 12 | 17 | 5 | 60 | 15 |
Table 3: Frequency table showing quality of life scores of patients with partial denture rehabilitation in University of Washington (N=34).
QOL calculated for patients without rehabilitation showed good score for mean and best score for shoulder, saliva, pain and swallowing, while chewing and anxiety had the lowest UW-QOL scores (Table 4).
| Variable | 0 | 25 | 30 | 50 | 70 | 75 | 100 | Mean | % Best Score of 100 |
|---|---|---|---|---|---|---|---|---|---|
| Pain | 9 | 28 | 94 | 76 | |||||
| Appearance | 6 | 28 | 3 | 73 | 8 | ||||
| Activity | 2 | 30 | 5 | 77 | 14 | ||||
| Recreation | 1 | 29 | 7 | 79 | 2 | ||||
| Swallowing | 13 | 24 | 90 | 65 | |||||
| Chewing | 37 | 50 | 0 | ||||||
| Speech | 9 | 25 | 3 | 63 | 8 | ||||
| Shoulder | 37 | 100 | 100 | ||||||
| Taste | 22 | 15 | 82 | 41 | |||||
| Saliva | 8 | 29 | 94 | 78 | |||||
| Mood | 9 | 5 | 22 | 1 | 60 | 3 | |||
| Anxiety | 16 | 21 | 53 | 0 |
Table 4: Frequency table showing quality of life scores in patients without partial denture rehabilitation in University of Washington (N=37).
Taste, activity and recreation were not adversely affected, but best quality of life was not attained by most of the patients. Most of the patients without rehabilitation had a lower QOL score for functional daily activities like chewing, speech and psychological effects of low mood and anxiety compared with the rehabilitated respondents (Table 4).
The UW-QOL importance question score was used to assess the most important complaint by the patients. In those rehabilitated, appearance and activity were the most important concerns while pain, recreation, shoulder, and anxiety were the least important concerns (Table 5).
| Variable | Patients with partial denture rehabilitation choosing the domain N=34 (%) | Rank order | Patients without partial denture rehabilitation choosing the domain N=37 (%) | Rank order |
|---|---|---|---|---|
| Pain | 0 | 9 | 0 | 8 |
| Appearance | 34(100.0) | 1 | 37(100.0) | 1 |
| Activity | 34(100.0) | 1 | 12(32.4) | 4 |
| Recreation | 0 | 9 | 0 | 8 |
| Swallowing | 2(5.9) | 8 | 2(5.4) | 6 |
| Chewing | 32(94.1) | 3 | 37(100) | 1 |
| Speech | 19(55.9) | 4 | 14(37.8) | 3 |
| Shoulder | 0 | 9 | 0 | 8 |
| Taste | 3(8.8) | 6 | 1(2.7) | 7 |
| Saliva | 3(8.8) | 6 | 0 | 8 |
| Mood | 8(23.5) | 5 | 8(21.6) | 5 |
| Anxiety | 0 | 9 | 0 | 8 |
Table 5: Comparison of important question score among patients in both groups in University of Washington.
Chewing and speech were also indicated as important complaints with scores of (94.1%) and (55.9%) respectively (Table 5). For those without rehabilitation, chewing (100.0%) and appearance (100.0%) were the most important concerns while pain, recreation, shoulder and anxiety were the least important concerns. Activity and speech were also indicated as important complaints with scores of (32.4%) and (37.8%) respectively.
The University of Washington global question score was used to compare the QOL before the tumour occurred in patients with and without partial denture rehabilitation. Table 6 shows the mean difference in health related QOL before the tumour and overall QOL / health related-QOL during the last seven days in patients with partial denture rehabilitation was lower [15-17] compared to patients without partial denture rehabilitation [18-20]. The percentage best scores for patients with partial denture rehabilitation were 56% compared to 40% in patients without rehabilitation.
| Variable | 0 | 20 | 25 | 40 | 50 | 60 | 75 | 80 | 100 | Mean | Best Score % | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A. Health-related QOL compared to month before tumour | With rehabilitation | 11 | 22 | 1 | 68 | 100 | ||||||
| No rehabilitation | 8 | 26 | 57 | 78 | ||||||||
| B. Health-related QOL during the past 7 days | With rehabilitation | 15 | 18 | 1 | 52 | 56 | ||||||
| No rehabilitation | 8 | 29 | 37 | 40 | ||||||||
| C. Overall QOL during the past 7 days | With rehabilitation | 15 | 18 | 1 | 52 | 56 | ||||||
| No rehabilitation | 8 | 29 | 37 | 40 | ||||||||
Table 6: Comparison of global question score among patients with and without partial denture rehabilitation.
There was no significant association between UW-QOL global scores on any of the variables studied. However, binary logistic regression for dichotomous variables was done to determine the best predictors for UW-QOL best scores, it showed only significant (β=0.876, P=0.031) association for socioeconomic class in the rehabilitated group (Table 6).
In response to the issues that were not adequately addressed by the questionnaire, numbness and biting of the lower lip in addition to inability to purse the lip were the concerns. In the rehabilitated group, two (5.9%) patients complained of numbness of the lower lip while one of them also complained of biting the lower lip when chewing. In the non-rehabilitated group, 10 (27.0%) patients had issues that were not addressed by the questionnaire; seven complained of numbness of the lower lip and four out of the seven also reported biting the lower lip while chewing, whereas the remaining three subjects reported inability to purse the lip.
The reasons given by the subjects in the experimental segmental with no reconstruction group for failure to undergo rehabilitation were as follows: financial constraints (n=32, 86.5%), not wanting bone taken from another part of the body/prosthesis to correct bony discontinuity defect (n=2, 5.4%), doubtful about the outcome of the rehabilitative procedures (n=2, 5.4%), and no reason (n=1, 2.7%).
Discussion
Oral health is an important part of general health and contributes to overall health-related QOL (HRQOL) [15]. Health-related QOL emphasizes health as opposed to disease and acknowledges that health is multi-dimensional while recognizing outcomes of preventive and treatment services, or no treatment at all as measurable and useful concepts [8,16]. Also, recognizing that clinical or self-reported oral health-related QOL indicators are both an outcome of one episode of care as well as risk or determinant of future episodes of care encourages the examination of long-term impact at the individual level [17]. Consequently, this study shows that most patients without rehabilitation had a lower QOL score for functional daily activities like chewing, speech and psychological effects of low mood and anxiety compared with the rehabilitated group; and that socio-economic class of the patients was the best predictor of better QOL. This better outcome in the rehabilitated patients resulted in their enhanced overall wellbeing more than the non-rehabilitated, and is in accordance with the literature [18,19].
The major reason for non-rehabilitation of patients in the experimental group was financial constraints. This financial constraint may have resulted in delay in treatment of the lesions, which allowed the lesions to progress in size leading to segmental mandibular resection as treatment modality rather than marginal mandibular resection. As the majority of them (n=31/37, 83.8%) are in the lower socio-economic class and in their prime age, the intervention of the relevant government agencies and non-governmental organizations to assist these patients overcome their deformities and live a more purposeful and appreciative life will be beneficial to them and the society. This is necessary in order to accomplish the core healthcare system values in our environment which include universal access to all citizens, effective care for better health outcomes, efficient use of resources, high-quality services and responsiveness to patient concerns. There is also the need to counsel the patients on the prognosis of the rehabilitative procedures such as the use of mandibular reconstruction plates, vascularized or non-vascularized bone grafts, and the replacement of the lost dentition by the use of partial dentures or implant-supported dentures so that they can appreciate the benefits better. These treatments are possible because of recent advances made in bone physiology, immunological concepts, tissue banking procedures, and surgical principles including the fabrication of oral and maxillofacial prosthesis which have made possible the successful reconstruction of most maxillofacial bony defects and lost dentition [3-5].
Some of the variables considered in this study such as shoulder, saliva, pain, taste and swallowing played little or no part in the determination of QOL in this series. This is to be expected as the lesions were all benign and locally invasive, and consequently the surgical procedures were limited to the sites where the lesions presented. This is similar to the report of Okoturo et al. [18,20] but differ from those of other researchers [3,21] where malignant lesions were reported and the surgical procedures were extended farther beyond the limit of the lesions.
Also, because of the many variables considered in this study, it was difficult to separate out individual determinants of QOL and this affected the statistically significant result obtained. As reported by earlier authors’ time since the initial resection appears to be an important determinant of QOL [22,23]. This may not have altered the results obtained in the present study as the questionnaire was administered on all the patients at 18 months after the initial surgery. However, it appears likely that over time as patient continue to heal, they become more adaptive, and possibly even learn to live better with difficulties and concerns and become more philosophical [3].
Patients’ age and gender did not play significant role in the present study as the age and gender in the two groups were comparably the same. However, according to Young et al. [3] patients’ age seems to play a role, as the younger a patient at the time of initial resection and rehabilitation, the better they seem to adapt, and the better the overall QOL. Also, gender appears to play a role, especially in global measures, as men more often achieve higher scores on the HRQOL including expressing less concern with pain over time than females [3,15,21]. Furthermore, it has been noted that time since resection and age at the time of resection have significant interactions with several QOL domains, particularly pain and speech, in that younger patients and those with most time since initial resection may appear to have fewer concerns with pain and with speech difficulties [3]. However, pain and to some extent speech were not of particular concern to the subjects in the present study due to the benign nature of the lesions and time the questionnaire was administered.
The locations and sizes of the mandibular defects in both categories of patients in the present study did not significantly affect HRQOL. On the contrary, Young et al. [3] noted that the site of resection appears to have some implications with resections (posterior) involving the mandibular angle having the most adverse effects on appearance and those involving the parasymphysis (lateral) having the most deleterious effect on overall QOL. Young et al. [3] and Rogers et al. [23] have also shown that parasymphysis resections adversely affect appearance, chewing, and lip support and it is likely that these factors contributed to a lower overall QOL in their series.
The report of numbness and biting of the lower lip by some patients in both groups was a consequence of the resection due to injury to the inferior alveolar nerve. It is surprising that only few patients mentioned it negatively in these series because all the patients studied experienced lip numbness after the resection. This may be because this complication has resolved in those that did not complain. Inability to purse the lip by some patients may be due to lack of bony support to the lower lip or it may have been subjective as the oro-facial muscles especially around the lips were not paralyzed before or after the resection. Young et al. [3] also reported numbness/biting of the lower lip and inability to purse the lip in their study.
Conclusion
This study has shown that the major concerns of the patients who have undergone mandibular resection due to benign locally invasive lesions were chewing ability, speech, appearance, anxiety and low mood, and these concerns were expressed more in the nonrehabilitated than the rehabilitated patients. These concerns should be kept in mind when they are being rehabilitated, and multi-disciplinary team work should be encouraged for their management. The trends and determinant of QOL observed should be used to decide targeted support in order to assist the patients overcome their deformities and disabilities.
References
- Luo HY, Li TJ (2009) Odontogenic tumors: a study of 1309 cases in a Chinese population. Oral Oncol 45: 706-711.
- Anyanechi CE, Saheeb BD (2014) A review of 156 odontogenic tumours in Calabar, Nigeria. Ghana Med J 48: 163-167.
- Young CW, Pogrel MA, Schmidt BL (2007) Quality of life in patients undergoing segmental mandibular resection and staged reconstruction with nonvascularized bone grafts. J Oral MaxillofacSurg 65: 706-712.
- Pogrel MA, Podlesh S, Anthony JP, Alexander J (1997) A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J Oral MaxillofacSurg 55: 1200-1206.
- Malik MA (2008) Textbook of oral and maxillofacial surgery, 2ndedn. Jaypee, New Delhi, pp: 469-496.
- Adekeye EO, Apapa DJ (1987) Complications and morbidity following surgical ablations of the jaws. West Afr J Med 6: 193-200.
- Tawfik MA, Zyada MM (2010) Odontogenictumors in Dakahlia, Egypt: analysis of 82 cases. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 109: e67-73.
- Green LW, Kreuter MW (1991) Health promotion planning: An educational and environmental approach. Mountain View, CA: Mayfield Publishing Company, pp 10-32.
- Hassan SJ, Weymuller EA Jr (1993) Assessment of quality of life in head and neck cancer patients. Head Neck 15: 485-496.
- Cella DF, Cherin EA (1988) Quality of life during and after cancer treatment. ComprTher 14: 69-75.
- Rogers SN, Lowe D, Brown JS, Vaughan ED (1999) The University of Washington head and neck cancer measure as a predictor of outcome following primary surgery for oral cancer. Head Neck 21: 394-401.
- Rogers SN, Lowe D, McNally D, Brown JS, Vaughan ED (2003) Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral MaxillofacSurg 61: 174-181.
- Lloyd S, Devesa-Martinez P, Howard DJ, Lund VJ (2003) Quality of life of patients undergoing surgical treatment of head and neck malignancy. ClinOtolaryngol Allied Sci 28: 524-532.
- Odedeji GA(1985) Socio-economic and cultural background of hospitalized children in Ilesha, Nigeria. Nig J Paed 1985; 12: 111-117.
- Shyama M, Honkala S, Al-Mutawa SA, Honkala E (2013) Oral health-related quality of life among parents and teachers of disabled schoolchildren in Kuwait. Med PrincPract 22: 285-290.
- Gift HC, Atchison KA, Dayton CM (1997) Conceptualizing oral health and oral health-related quality of life. SocSci Med 44: 601-608.
- Al-Shammari KF, Al-Ansari JM, Al-Khabbaz AK, Dashti A, Honkala EJ (2007) Self-reported oral hygiene habits and oral health problems of Kuwaiti adults. Med PrincPract 16: 15-21.
- Okoturo E, Ogunbanjo O, Akinleye A, Bardi M (2011) Quality of life of patients with segmental mandibular resection and immediate reconstruction with plates. J Oral MaxillofacSurg 69: 2253-2259.
- Schmelzeisen R, Neukam FW, Shirota T, Specht B, Wichmann M (1996) Postoperative function after implant insertion in vascularized bone grafts in maxilla and mandible. PlastReconstrSurg 97: 719-725.
- Schrag C, Chang YM, Tsai CY, Wei FC (2006) Complete rehabilitation of the mandible following segmental resection. J SurgOncol 94: 538-545.
- Hundepool AC, Dumans AG, Hofer SO, Fokkens NJ, Rayat SS, et al. (2008) Rehabilitation after mandibular reconstruction with fibula free-flap: clinical outcome and quality of life assessment. Int J Oral MaxillofacSurg 37: 1009-1013.
- Rogers SN, Panasar J, Pritchard K, Lowe D, Howell R, et al. (2005) Survey of oral rehabilitation in a consecutive series of 130 patients treated by primary resection for oral and oropharyngeal squamous cell carcinoma. Br J Oral MaxillofacSurg 43: 23-30.
- Rogers SN, Lowe D, Fisher SE, Brown JS, Vaughan ED (2002) Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral MaxillofacSurg 40: 11-18.
Citation: Anyanechi CE, Edet ES, Saheeb BD (2016) Comparison of Quality of Life after Mandibular Resection: A Cohort Study of Patients in the Same Institution. J Clin Exp Pathol 6:271. DOI: 10.4172/2161-0681.1000271
Copyright: © 2016 Anyanechi CE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12655
- [From(publication date): 4-2016 - Aug 31, 2025]
- Breakdown by view type
- HTML page views: 11697
- PDF downloads: 958