Diffuse Tenosynovial Giant Cell Tumour Current Treatment Options: A Systematic Review
Received: 16-Aug-2021 / Accepted Date: 30-Aug-2021 / Published Date: 06-Sep-2021 DOI: 10.4172/2472-016X.1000153
Abstract
Aim: Diffuse Tenosynovial Giant Cell Tumour (TGCT) formerly recognized under the synonym Pigmented Villonodular Synovitis (PVNS), is a proliferative, locally destructive, benign synovial tumour. Which most commonly affects monoarticular weight bearing joints. This disease often results in a debilitating functional impairment for the patient, early osteoarthritis, coupled with a tenacious recurrence rate. Current treatment options include early synovectomy, radiation therapy and colony stimulating factor-one (CSF-1) inhibitor Pexidartinib. However, there is a dearth of treatment protocols and management can prove difficult. The purpose of this study was to systematically review the most recent treatment methods of TGCT affecting weight bearing knee, hip, and ankle joints.
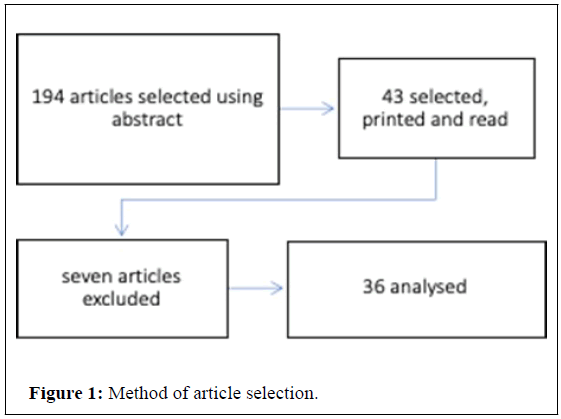
Methods: A systematic review of literature was carried out in July 2021. Keywords included “Treatment Options” and “Diffuse Tenosynovial Giant Cell Tumour.” The authors then examined 194 articles of which 36 articles were selected and read.
Study design: Review of Literature, level of evidence IV.
Results: 36 articles were selected.
Conclusion: It is apparent diffuse TGCT has the potential to cause severe functional impairment for the patient. A combination approach utilizing both surgical and systemic treatment modalities appear the current best clinical practice against this obdurate tumour.
Keywords: Diffuse tenosynovial giant cell tumour; Pigmented villonodular synovitis; Pexidartinib; Arthroscopic synovectomy; Open total synovectomy; Radiotherapy; CSF-1 inhibitors; Limb amputation
Introduction
Diffuse tenosynovial giant cell tumour (D-TGCT) is an uncommon benign neoplasm. Hypertrophic in nature, it can occur in tendon sheaths. Diffuse TGCT was first recorded in medical literature by Chassaignac in 1882. As a disease process, it has been recorded to affect a variety of joints within the body, however for the purposes of this review; I will focus on D-TGCT affecting weight bearing hip, knee, and ankle joints intra particularly. Despite being ascribed as benign it yields significant local destruction, therefore ensuring initiation of early treatment is vital. Treatment options currently available include arthroscopic synovectomy, open total synovectomy, radiotherapy, CSF-1 inhibitors, and limb amputation. The objective of this systematic review of the literature was to analyze the current treatment options used for diffuse TGCT of the lower limb, and their clinical efficacy.
Methodology
Selection criteria
Inclusion criteria were all articles who discussed treatment modalities for diffuse type TGCT of the lower limb. Pre-selection criteria is listed below, any articles which did not meet selection criteria were removed from study:
1. Free articles
2. PubMed articles
3. English articles
4. Abstract available
5. Treatment of diffuse TGCT
6. Lower limb diffuse TGCT, hip, knee, ankle only
7. Not limited by
8. Year of publication
9. Patient age
10. Type of article
Research methods
During July 2021, a PubMed bibliographic search was performed in PubMed, there was no time limit set for this literature search. Keywords “Diffuse Tenosynovial Giant Cell Tumour” and “Treatment Options.” Authors then selectively decided which articles directly responded to the question requirements. This was achieved firstly using article abstracts, then articles were thoroughly read to assess compatibility with the research question.
This systematic review is structured according to the PRISMA checklist for systematic reviews in Figure 1.
Results
Thirty articles for this systematic review were selected and read. There were seven articles which were not included secondary to unclear outcomes, nodular TGCT or limited information in comparison to other articles available in Table 1.
| Treatment modalities | Number of studies | Total number of patients |
|---|---|---|
| Radiotherapy | 10 | 104 |
| Synovectomy | 17 | 169 |
| Drug therapies | 7 | 116 |
| Limb amputation | 1 | 4 |
Table 1: Different treatment modalities of diffuse TGCT, the number of studies included and their respective patient population.
Radiotherapy
In 2009 highlighted the increased rate of local TGCT reoccurrence when surgical resection is used as a monotherapy [1]. Post total synovectomy external beam radiation therapy or IR injection of yttrium-90 produced significantly better results. Their study included 12 diffuse TGCT patients who received an external beam radiation regime, around six to eight weeks post anterior and posterior synovectomy. They employed a variety of means to assess recurrence rates, magnetic resonance imaging coupled with X-Ray and clinical examination between twenty and thirty-six months. There were no cases of disease recurrence or articular damage furthermore no complications were recorded.
The use of combined surgical and radiation therapy is evidenced in an earlier study examining diffuse foot and ankle TGCT treatment [2]. In their prospective study, they followed up seven patients at a mean of 24 months who underwent total synovectomy and radiotherapy. They report six patients reported lower pain scores and better functional outcomes, whilst no patients were found to have disease recurrence.
The IR injection of Yttrium-90 silicate into eight patients’ knees with diffuse TGCT was examined [3]. A recurrence rate of 75% was recorded post either one or two total synovectomies. Post one or two treatments with yttrium, arthroscopy and biopsy six months later revealed both less villi numerus and less prominent. Furthermore, there were no complications noted with radiosynoviotheses [1].
It was assessed the long-term functional outcomes regarding different treatment modalities of diffuse TGCT in the knee joint. They looked at twenty-two years’ worth of data within a single center. Twenty-four patients were included, nineteen of which underwent open total synovectomy and five who underwent arthroscopic synovectomy. Fourteen of these patients underwent radiotherapy median thirty-five Gy. They found a 45.45% recurrence rate. However, this rate was only 8.3% in the group who underwent adjuvant radiotherapy, in comparison to the higher rate of 57.1% in those without adjuvant radiotherapy.
Surgical treatment
They compare rates of recurrence and knee joint arthritis in open versus arthroscopic surgical management of TGCT. Using retrospective analysis, they identified forty-eight patients with knee TGCT, treated either by open posterior approach, open anterior approach, or open posterior coupled with arthroscopic anterior or a purely arthroscopic surgical approach. They also analyzed recurrence rates, joint arthritis rates and patient statistics. Their median follow up was forty months. Recurrence rates were found to be 9% in the open posterior combined with arthroscopic anterior group. Much lower than the arthroscopic group 62%, and the purely open group 64%. Furthermore, there were no statistical difference between arthritis progression in groups. The most common complication found was hemarthrosis with was dragged in 6% of study group. They conclude by purporting that higher recurrence rate in arthroscopic group may be explained by difficulty in synovial removal using a posterior arthroscopic approach.
In direct comparison, highlight a current lack of consensus within the surgical community of open or arthroscopic diffuse TGCT removal [4]. They emphasize early surgical treatment is beneficial in overall disease remission. They discuss arthroscopic synovectomy as having a reduced morbidity whilst, open synovectomy has a higher disease remission rate. In their systematic review they were unable to comment with total confidence on which technique is more successful at halting osteoarthritis progression and ultimately the requirement of a total knee arthroplasty.
The aim was to investigate longitudinal clinical outcomes of TGCT removal either via an open or arthroscopic approachs through a systematic literature review. They selected forty articles, and found in diffuse TGCT, arthroscopic synovectomy has only been reported within the knee joint. They could not therefore verify that surgical treatment avoids joint osteoarthritis within ankle and hip joints.
They evaluated the longitudinal clinical results of total synovectomy in TGCT of the knee joint. Nineteen patients underwent open total synovectomy, fifteen of these had diffuse TGCT. Mean of 80.2-months clinical follow-up. An adjuvant radiotherapy course was completed by one patient secondary to disease recurrence. It was found that disease recurrence occurred in five patients, whilst four patients underwent a secondary total synovectomy. There were two patients who underwent three synovectomies. Throughout this study a total of seven patients underwent a total knee arthroplasty. There were no cases of septic arthritis or hemarthrosis. Whilst they found three patients had post-surgery joint stiffness. Knee society scores ranged from eight-‘perfect’, nine-‘good’ and two ‘bad.’
The paper describes a case report of ten-year-old patient diagnoses with diffuse TGCT, on a background of four months of intermittent, unilateral knee pain and swelling [5]. Arthroscopic synovectomy was undertaken and histology confirmation of TGCT. No further surgeries were required, and no post-operative complications occurred.
Arthroscopic treatment challenges are frequent due to limited joint exposure [6]. They report a new technique in surgically removing diffuse TGCT located within the hip joint. This is via a puncture capsulotomy, which enables total surgical vision through both the peripheral and central compartments. This, they report is essential for total tumour debridement, ensuring extra attention is paid to both the lateral and medial synovium’s folds. It emphasizes the importance of ensuring there is no high outflow irrigation used and temperature should remain a constant, as this reduces risk of chondral damage [6]. They also advised against using a shaver, as this can encourage further tumour seeding. Puncture capsulotomy doesn’t require capsular repair, furthermore it ensures the iliofemoral ligament remains intact. It reports a systematic review case series which portrays lower recurrence rates with arthroscopic treatment of hip TGCT at 7.7% in direct comparison to an open synovectomy treatment with a recurrence rate of 17.8% [6].
The lack of literature of hip TGCT is highlighted within the paediatric population. They report two case reports of hip TGCT [7]. They retrospectively reviewed TGCT patients less than nineteen years of age, in one clinical center manage through via arthroscopic total synovectomy. They reported a total of five patients were included, there were seven operations in total. Only one patient was diagnosed with diffuse TGCT at mean clinical review, thirty-two months, all patients were in clinical remission. The diffuse TGCT patient unfortunately demonstrated pre-surgical degenerative change and progressive postoperative functional reduction.
The paper described their arthroscopic technique for treatment of diffuse TGCT. They advised use of a leg holder which increases access to the joint and allows for knee flexion intraoperatively, allowing debridement within posterolateral and medial compartments [8]. Increasing the number of portals used including: superomedial; superolateral; accessory posteromedial and accessory posterolateral. Adequate access through the posterolateral portal, they state enables tumour clearance close to cruciate ligaments. They encourage regular shaver changing up to three, and cycling between portals, 30°C-70°C degree arthroscopes.
There was a retrospective review of arthroscopic treatment of diffuse TGCT with no adjuvant radiotherapy [9]. They reviewed 40 patients, with both local and diffuse TGCT between 1987-2012, with a mean seven-year follow-up. In diffuse TGCT there was a five-year reoccurrence free survival probability of 57%. However, there were twelve patients who had tumour reoccurrences between 3 months-24 months.
It also recommends the arthroscopic treatment of TGCT within the hip joint. Similarly, to they advise multiple portals for adequate exposure [8,10]. Furthermore, performing a T-capsulotomy enables the surgeon better access to hips peripheral and central compartments.
They followed 26 patients who were diagnosed with TGCT of their knee joint, between 1996-2012. Yearly clinical follow up and MRIs with Knee Society Score grading methods employed. Fifteen patients had diffuse TGCT, four patients underwent open anterior partial synovectomy, whilst one patient underwent arthroscopic partial synovectomy, secondary to posterior synovium remaining intact. It was reported no further surgery or symptoms. Whilst the ten other patients underwent total synovectomy, seven open staged arthrotomies, two arthroscopic and one full anterior arthroscopic with a posterior open synovectomy. They noted that two of their patients suffered from diffuse TGCT reoccurrence, one patient was treated with further anterior arthroscopic debridement and open resection posteriorly. Whilst the other underwent arthroscopic resection. They did not use adjuvant radiation therapy during this trial as there was concern expressed regarding radiation induced sarcomas.
They reviewed articles published between 2010-2013 to assess open versus arthroscopic approaches for treatment of TGCT. An analysis of ten studies was undertaken, the TGCT recurrence rate with open synovectomy was 26.7% whilst arthroscopic synovectomy was found to be 24.6%. Furthermore, complication rates were 5.7% and 3.2%. It was concluded that there was no significant difference between the surgical techniques regarding recurrence or complication rates.
They evaluated recurrence rates of TGCT in the knee joint post primary arthroscopic synovectomy, retrospectively analyzed seven patients with diffuse TGCT, who underwent total synovectomy coupled with chemical synovectomy-pre 2007 Osmic acid and post-2007 Hexacetonide [11]. There were two patients who had tumour recurrence post two and five years, open synovectomy was performed, and no further recurrence was found on last follow-up. Therefore, they conclude that arthroscopic synovectomy provides excellent disease control of TGCT [11].
They advised multi-treatment approach for diffuse TGCT. Surgery with necessary adjuvant treatments judged on a patient by patients’ basis [12].
There systematic review of TGCT corresponds to previous clinical studies of diffuse TGCT and its persistent disease progression. Arthroscopic approach versus open is no more clarified given their findings [13].
They retrospectively examined surgical treatment of osseous erosion of diffuse TGCT within the ankle joint [14]. They selected fifteen patients with diffuse TGCT who were managed with open synovectomy and then bone grafting for subchondral cysts. They followed up at a mean time of 37.4 months. Fifteen patients had erosion of the talus; five patients had distal tibial involvement whilst seven patients also had tendon involvement. Furthermore, two patients had significant progression of ankle osteoarthritis which required ankle fusion.
It describes their first case series of limb amputation for recurrent diffuse or metastatic TGCT [15]. Initially treatment with open or arthroscopic synovectomies, radio synovectomy and external beam radiotherapy plus tyrosine kinase inhibitor therapy were employed. However secondary to infection, peri prosthetic fracture, pain and significantly reduced mobility and quality of life, limb amputations were used.
They aimed to assess the differences between staged anterior and posterior synovectomies over simultaneous surgery [16]. They retrospectively examined nineteen diffuse TGCT patients from 2001-2007, with a median follow up of ninety-eight months. On an MRI exam, there was residual tumour in five patients, however there was no progression in three with a knee score of 86-90. However, two patients found to have recurrence six and nine months.
Drug therapies
The largest of phase III TGCT trials is a random double-blinded multicenter trial, named ENLIVEN. (NCT02371369) It included centers across 12 countries, inclusion criteria included 120 patients with symptomatic TGCT which was not surgical respectable. The was random assignment to pexidartinib and placebo. There was split dosing of morning and evening pexidartinib, 400 mg and 600 mg for a total period of 2 weeks and then a dose reduction of 400 mg BD for 5.5 months. Phase II of this study-initiated crossover for placebo cohort post 6 months. The response rate was measured at week 25 via ROM assessment in large joints and tumour volumes, whilst quantitative surveys of pain and patient satisfaction were employed. 61 patients were delegated to pexidartinib treatment group whilst 59 were assigned to placebo group. An initial endpoint was set at 25 weeks, with 15% patients fulfilling criteria to meet a complete response whilst 24% displayed a partial response. Tumour volume scores decreased in 56% patients, 5% pexidartinib and 51% partial responders. Of note there were response rates still recorded 6 months and 17 months being the longest recorded response rates. There was no tumour progression noted. Patient recorded surveys convey large improvements in ROM and not statistically significant pain score reductions in pexidartinib groups. It was noted in the ENLIVEN trial 23 patients in pexidartinib group (38%) 6 patients (10%) in placebo underwent a dose reduction secondary to side effects. Side effects reported included 54% fatigue, deranged LFT’s (39%) and diarrhoea (25%). The ENLIVEN trial demonstrated hepatic enzyme derangement to be reversible AST and ALT increases. It appears there is transient Kupffer liver cell cytotoxicity when taking pexidartinib, therefore slowing transaminase clearance.
They cultured fibroblast-like synoviocytes (FLS) a cell which comprises TGCT synovial structure. Cadherin-11 is a molecule that controls adhesion of cells in FLS and as a result has an important role in TGCT aberrant pathogenesis [17]. They down-regulated cadherin-11 via siRNA and they evaluated invasion and movement of TGCT FLS using wound healing assays. They found inflammatory factors in TGCT patients synovial fluid to have increased regulation, with increased amounts of Cadherin-11. They found that by downregulating cadherin-11 blocked inflammatory factor pathways and prevented the migration of TGCT FLS.
They examined the efficacy and safety of intravenous emactuzumab as a systemic treatment option in diffuse TGCT. Emactuzumab is an anti-colony stimulating factor 1 receptor (CSF-1R). Patients were followed up two years post treatment, they received a dose of emactuzumab every two weeks, with optimum dosing of 1 gm. Assessment involved qualitative surveys to assess life quality, adverse effects or complications and tumour biopsy to assess biomarkers. MRI imaging was used to investigate tumour burden and size. There were sixty-three patients included with reported side effects of asthenia, oedema, and pruritus. Biopsy in thirty-six patients revealed a CSF1R and macrophage reduction. Study objective response rate 71% and quality of life improvements were reported, with a reliable drug safety profile.
It reports on Imatinib Mesylate (IM) and its ability to block CSF-1R thereby reducing tumour pathogenesis, evaluating this via tumour volume assessment through PET-CT and MRI [18]. Twenty-five patients were given IM, thirteen of these had diffuse TGCT. Median treatment time was seven months. Unfortunately, 80% of patients ceased treatment secondary to insufficient response or imminent surgery. MRI of affected joints portrayed 32% partial response rate and 63% static disease. PET-CT revealed a reduced mean difference of 5.3 between post IM and pre-treatment. In fifteen patients there was no correlation achieved between PET-CT and MRI. It is apparent there is some moderate response to IM displayed through PET-CT.
The systematic review highlights Pexidartinib’s upregulation effect on M2 macrophage's anti-oncogenic activity in the context of diffuse TGCT [19].
They retrospectively examined diffuse TGCT management via CSF-1R tyrosine kinase inhibitors (TKI) in a long-term setting [20]. Thirty-nine patients who had been previously treated for a median of seven months with either CSF-1R TKI or Ab. There was a median review time of thirty months, it was found that 56% were tumour progression free at this time. Fifteen patients had disease recurrence after CSF-1R inhibitor and twelve of these had a second line treatment for six to twelve months. Post these six patients had a persistent reoccurrence and five of these had a third treatment from five-nine months.
They report on a diffuse TGCT patient who post receiving pexidartinib treatment sustained a 48% reduction in tumour volume [21]. This was only four months from receiving her initial dose. Fiftyfive months post treatment initiation her disease remained stable with a significant reduction in symptoms.
Discussion
Radiotherapy appears to have excellent use in the treatment of diffuse TGCT as a combination therapy. In this study it is apparent that the combination of moderate dosed radiotherapy is of great benefit to locally control diffuse knee joint TGCT, whilst maintaining joint functionality.
They similarly report on the benefits of combined external beam radiotherapy and surgical synovectomy. Particularly in those with multiple soft tissue neoplasms within a joint [22]. They examined fifty patients who underwent treatment for diffuse TGCT between 1972 and 2006. Patients were clinically reviewed at their presentation and then again, at one year. Whilst one patient had malignant TGCT, forty-nine had diffused both intra and extra-particular type. 60% of these patients had two previous resections pre-radiotherapy. Mean radiation dosage used was 39.8 Gy. Furthermore, at mean follow up of ninety-four months, 94% of patients did not have disease recurrence or had stable disease on MRI. It is apparent that a combination approach promotes significantly reduced disease burden and a beneficial functional outcome in comparison to surgery alone.
In their case study reports an excellent clinical outcome of a 27- year-old diagnosed with diffuse TCGT of her right knee [23]. A combined open synovectomy with external beam radiotherapy, gave two years of remission. MRI diagnosed recurrence and a total arthroscopic synovectomy was carried out with further adjuvant radiotherapy. This allowed further remission without recurrence of 1 year. This combined approach appears a successful treatment method, like the study [1].
The potential of radiation induced cancers is highlighted via their study, the risk of radiotherapy treatment in benign diseases [24]. The risk of radiation induced cancer years post treatment. They examined epidemiological and phantom studies and found the risk of radiation induced cancer in benign disease to be low in adults, if using advised dosage protocols.
Interestingly, reported treatment of diffuse TGCT in a 33-year-old males knee joint using radio synovectomy as a primary treatment modality [25]. Yttrium-90 hydroxyapatite was selected secondary to desirable decay characteristics. The patient on three-month review reported greater joint function and a reduction in overall joint size. This monotherapy appears an unusual approach as generally radiotherapy is combined with a surgical treatment.
They discuss about radio synovectomy as a repeatable method of TCGT treatment. Reducing synovial villi, joint effusion and halting active synovitis. Injection of radiocolloid irradiates synovial cells, causing a fibrotic reaction and preventing further tumour burden. They recommend ultrasound guided isotope injection for precision and further ultrasound assessment during review to assess for synovial fibrosis. They report a success rate of between 65%-80%. This study agrees with earlier study using Yttrium-90 [3].
In their retrospective observation study assessed outcomes of arthroscopically assisted radiotherapy of knee joint TGCT [14]. They selected twenty-eight TCGT patients between 2006 and 2011. Twenty-six patients had adjuvant post arthroscopic synovectomy radiotherapy. Mean follow up was fifty-four months. Patients who underwent adjuvant radiotherapy had no tumour recurrence. Whilst their knee function score increased significantly post therapy. They conclude that radiotherapy is essential to prevent disease recurrence.
In their retrospective analysis of clinical outcomes of TGCT knee joints post combined low dose radiotherapy and both open and arthroscopic synovectomy [26]. They reviewed twenty-three patients between 1998-2007. They found nineteen patients had primary TGCT whilst four had recurring TGCT. Post total synovectomy, six open and seventeen arthroscopic, each patient received a radiation dose of either 6-MV or 4-MV, a 20 Gy median dose through ten fractions. It was found that at median review, only four patients had disease recurrence, with a remission median of five years. Three of the patients underwent further synovectomy and this was permissive to disease remission. However, univariate analysis dosage of radiation, joint trauma or age were not predictive factors to disease control. Twenty-two patients in total advised good knee function, whilst there was no radiation induced neoplasia or toxicity. Similarly, to conclude that post-surgical adjuvant radiotherapy is effective against disease burden and recurrence in TGCT [14]. They also advise low dose 20 Gy portrays similar efficacy as 35 Gy dosage.
Surgical treatment
Surgical treatment of diffuse TGCT appears vital to adequate treatment of this disease. Tumour debulking and debridement is essential for joint functioning and patient quality of life. In their longitudinal analysis, concluded that neither a single surgical nor combination treatment of diffuse TGCT can provide an absolute solution [27]. They do not differentiate between open or arthroscopic total synovectomy; unlike they state both to be a gold standard treatment approach [28].
Furthermore, they found combined anterior and posterior synovectomies with adjuvant radiotherapy ensured rates of recovery like that with staged synovectomies [16]. They advise for bony destruction of the ankle joint with diffuse TGCT bone grafting and open synovectomy provides effective management [29].
They found no significant difference between the surgical techniques regarding recurrence or complication rates [30]. In this study it is apparent that most orthopedic centers rely on a combined approach of anterior arthroscopic first stage and then an open posterior stage in knee joint diffuse TGCT [30].
The concluded that arthroscopic debridement displayed excellent efficacy as a treatment method against both local and diffuse TGCT [9]. Whilst tumour recurrence can be arthroscopically debrided, allowing the patients a good functional recovery.
They do mention that in most cases using their arthroscopic technique should enable good tumour removal [8]. However, in a minority of cases an open posterior synovectomy can be used in combination.
The study they highlight the lack of pediatric diffuse TGCT cases and treatment methods documented. It is apparent further research is evidently required on pediatric prognosis and treatment.
In this study, they highlight there is a role for amputation in extreme cases of this locally aggressive disease [15]. This is an important option to give to patients in recurrent treatment resistant diffuse TGCT. This drastic end stage treatment can, in severe cases, improve the patient’s quality of life.
Drug therapies
The study highlights that more clinical trials are required to identify further CSF-1R inhibitors which can be paired with adjuvant therapies [19]. This is seconded by their study on Imatinib Mesylate, more research into this drug is required, it appears there is a moderate response to this drug, could more efficacious drug deliverance be achieved? [31].
This study concluded combined therapeutic treatment lines are required for almost 50% of relapsing diffuse TGCT patients [20]. Whilst in study suggests pexidartinib’s use as a neoadjuvant presurgical method of reducing tumour volume, thereby reducing surgical risk, and improving surgical outcomes [21]. In their study emactuzumab demonstrated substantial levels of symptomatic improvement within the patient cohort, this is promising however more research is required [18]. Similarly, it is apparent cadherin-11 is an important factor in TGCT pathogenesis, inhibiting cadherin-11 and downregulating inflammatory pathways presents a new option for a systemic therapeutic treatment avenue [17].
Pexidartinib is the first inhibitor of CSF-1R to have gained FDA approval. The pre-clinical data have demonstrated the use of pexidartinib not only against TGCT but also in the treatment of other solid tumors [32]. Currently Pexidartinib has no FDA approval for use in other cancers. The FDA current treatment guidelines are 400 mg PO BD [33]. The ENLIVEN study patient follow ups demonstrated increased response rates than observed in the study [34]. There are well documented side effects from pexidartinib, particularly deranged liver enzymes and potentially critical hepatotoxicity [35,36]. There is a risk evaluation and mitigation strategy (REMs) program which allows these events to be recorded and evaluated properly [37].
Conclusion
It is apparent that treatment of diffuse TGCT is slowly expanding to halt this destructive disease process. Localized disease form can often be managed with arthroscopic synovectomy. However, diffuse TGCT is much more difficult to treat well. This review of literature portrays that arthroscopic synovectomy for non-recurrent diffuse TGCT is often efficacious. However, in persistent occurrences open surgery combined with adjuvant radiotherapy and CSF-1R inhibitors appears of great clinical benefit. Limitations of this study include using one literature database and free articles with an English translation. Recommendations include further large longitudinal random cohort trials, across multiple orthopedic treatment centers.
Conflict of Interest
None
References
- Nassar WAM, Bassiony AA, Elghazaly HA (2008) Treatment of diffuse pigmented villonodular synovitis of the knee with combined surgical and radiosynovectomy. HSS Journal 5: 19-23.
- Lee M, Mahroof S, Pringle J, Short SC, Briggs TWR (2005) Diffuse pigmented villonodular synovitis of the foot and ankle treated with surgery and radiotherapy. Int Orthop 29: 403-405.
- Franssen MJ, Boerbooms AM, Karthaus RP, Buijs WC, Van de Putte (1989) Treatment of pigmented villonodular synovitis of the knee with yttrium-90 silicate: prospective evaluations by arthroscopy, histology, and 99mTc pertechnetate uptake measurements. Ann Rheum Dis 48: 1007-1013.
- Quaresma MB, Portela J, Soares do Brito J (2020) Open versus arthroscopic surgery for diffuse tenosynovial giant-cell tumours of the knee: A systematic review. EFORT Open Rev 5: 339-346.
- Poutoglidou F, Metaxiotis D, Mpeletsiotis A (2020) Pigmented villonodular synovitis of the knee joint in a 10-year-old patient treated with an all-arthroscopic synovectomy: A case report. Cureus 12: e11929.
- Nazal MR, Parsa A, Martin SD (2019) Arthroscopic treatment of pigmented villonodular synovitis of the hip using puncture capsulotomy. Arthrosc Tech 8: 641-646.
- Willimon SC, Schrader T, Perkins CA (2018) Arthroscopic management of pigmented villonodular synovitis of the hip in children and adolescents. Orthop J Sports Med 6: 232596711876311.
- Chang JS, Higgins JP, Kosy JD, Theodor Poulos J (2017) Systematic arthroscopic treatment of diffuse pigmented villonodular synovitis in the knee. Arthrosc Tech 6: e1547-e1551.
- Jain JK, Vidyasagar JVS, Sagar R, Patel H, Chetan ML (2013) Arthroscopic synovectomy in pigmented villonodular synovitis of the knee: clinical series and outcome. Int Ortho 37: 2363-2369.
- Lee S, Haro MS, Riff A, Bush-Joseph CA, Nho SJ (2015) Arthroscopic technique for the treatment of pigmented villonodular synovitis of the hip. Arthrosc Tech 4: 41-46.
- Auregan JC, Bohu Y, Lefevre N, Klouche S, Naouri JF (2013) Primary arthroscopic synovectomy for pigmented villo-nodular synovitis of the knee: Recurrence rate and functional outcomes after a mean follow-up of seven years. Orthop Traumatol Surg Res 99: 937-943.
- Bernthal NM, Ishmael CR, Burke ZDC (2020) Management of pigmented villonodular synovitis (PVNS): an orthopedic surgeon’s perspective. Curr Oncol Rep 22: 56.
- Healey JH, Bernthal NM, Van de Sande M (2020) Management of tenosynovial giant cell tumor: A neoplastic and inflammatory disease. JAAOS: Global Research and Reviews 4: 20.00028.
- Li W, Sun X, Lin J, Ji W, Ruan D (2015) Arthroscopic synovectomy and postoperative assisted radiotherapy for treating diffuse pigmented villonodular synovitis of the knee: An Observational Retrospective Study. Pak J Med Sci 31: 4.
- Mastboom M, Verspoor F, Gelderblom H, Van de Sande M (2017) Limb amputation after multiple treatments of tensynovial giant cell tumour: Series of 4 Dutch Cases. Case Rep Orthop 17: 7402570.
- Chen, WM, Wu, PK, Liu (2012) Simultaneous anterior and posterior synovectomies for treating diffuse pigmented villonodular synovitis. Clin Orthop Relat Res 470: 1755-1762.
- Cao C, Wu F, Niu X, Hu X, Cheng J (2020) Cadherin-11 cooperates with inflammatory factors to promote the migration and invasion of fibroblast-like synoviocytes in pigmented villonodular synovitis. Theranostics 10: 10573-10588.
- Cassier PA, Italiano A, Gomez-Roca C, Le Tourneau C, Toulmonde M (2020) Long-term clinical activity, safety, and patient-reported quality of life for emactuzumab-treated patients with diffuse-type tenosynovial giant-cell tumour. Eur J Cancer 141: 162-170.
- Benner B, Good L, Quiroga D, Schultz TE, Kassem M (2020) Pexidartinib, a novel small molecule CSF-1R inhibitor in use for tenosynovial giant cell tumor: A systematic review of pre-clinical and clinical development. Drug Des Devel Ther 14: 1693-1704.
- Brahmi M, Cassier P, Dufresne A, Chabaud S, Karanian M (2020) Long term follow-up of tyrosine kinase inhibitors treatments in inoperable or relapsing diffuse type tenosynovial giant cell tumours (dTGCT). PLoS ONE 15: e0233046.
- Giustini N, Bernthal NM, Bukata SV, Singh AS (2018) Tenosynovial giant cell tumor: Case report of a patient effectively treated with pexidartinib (PLX3397) and review of the literature. Clin Sarcoma Res 8: 1.
- Griffin AM, Ferguson PC, Catton CN, Chung PWM, White LM (2012) Long-term outcome of the treatment of high-risk tenosynovial giant cell tumor/pigmented villonodular synovitis with radiotherapy and surgery. Cancer 118: 4901-4909.
- Duan Y, Qian J, Chen K, Zhang Z (2018) Necessity of adjuvant postoperative radiotherapy for diffuse pigmented villonodular synovitis of the knee. Med 97: 9637.
- McKeown SR, Hatfield P, Prestwich RJ, Shaffer RE, Taylor RE (2015) Radiotherapy for benign disease; assessing the risk of radiation-induced cancer following exposure to intermediate dose radiation. Br J Radiol Suppl 88: 20150405.
- Kamaleshwaran K, Krishnan B, Gounder T, Chakraborty S, Kalarickal R (2015) Use of yttrium-90 hydroxyapatite radiosynovectomy as a primary modality of treatment in diffuse pigmented villonodular synovitis of the knee joint: A first case report. Indian J Nucl Med 30: 47.
- Park G, Kim YS, Kim JH, Lee S, Song SY (2012) Low-dose external beam radiotherapy as a postoperative treatment for patients with diffuse pigmented villonodular synovitis of the knee. Acta Orthopaedica 83: 256-260.
- Akinci O (2011) Long-term results of surgical treatment of pigmented villonodular synovitis of the knee. Acta Orthopaedica et Traumatologica Turcica 45: 149-155.
- Colman MW, Ye J, Weiss KR, Goodman MA, McGough RL (2013) Does combine open and arthroscopic synovectomy for diffuse PVNS of the knee improve recurrence rates? Clin Orthop Relat Res 471: 883-890.
- Li X, Xu Y, Zhu Y, Xu X (2017) Surgical treatment for diffused-type giant cell tumor (pigmented villonodular synovitis) about the ankle joint. BMC Musculoskelet Disord 18: 1.
- Rodriguez-Merchan EC (2014) Review article: Open versus arthroscopic synovectomy for pigmented villonodular synovitis of the knee. J Orthop Surg 22: 406-408.
- Mastboom MJL, Lips W, Van Langevelde K, Mifsud M, Ng C, McCarthy CL (2020) The effect of imatinib mesylate in diffuse-type tenosynovial giant cell tumours on MR imaging and PET-CT. Surg Oncol 35: 261-267.
- Chien JC, Wei YP, Chen CY, Hsiang WH, Wang YY (2021) Long-term functional outcomes of diffuse pigmented villonodular synovitis of knee. Medicine 100: e23794.
- Cwikla J, Zbikowski P, Kwiatkowska B, Buscombe J, Sudol-Szopinska I (2014) Radiosynowektomia chorobach reumatycznych. J Ultrason 14: 241-251.
- Moher D (2009) Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. Ann Intern Med 151: 264.
- Noailles T, Brulefert K, Briand S, Longis P, Andrieu K (2017) Giant cell tumor of tendon sheath: Open surgery or arthroscopic synovectomy? A systematic review of the literature. Orthop Traumatol Surg Res 103: 809-814.
- Sharma H, Rana B, Mahendra A, Jane MJ, Reid R (2007) Outcome of 17 pigmented villonodular synovitis (PVNS) of the Knee at 6 years mean follow-up. The Knee 14: 390-394.
- Tap W (2020) ENLIVEN study: Pexidartinib for tenosynovial giant cell tumor (TGCT). Future Oncol 16: 1875-1878.
Citation: Doran CFD, Miller P, Molloy AP (2021) Diffuse Tenosynovial Giant Cell Tumour Current Treatment Options: A Systematic Review. J Orthop Oncol 7:153. DOI: 10.4172/2472-016X.1000153
Copyright: © 2021 Doran CFD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2600
- [From(publication date): 0-2021 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 1895
- PDF downloads: 705