Effective Prevention and Control of Corona Virus Disease 2019 (COVID-19) Experiences from Inflection Point for SARS
Received: 22-Feb-2021 / Accepted Date: 18-Mar-2021 / Published Date: 25-Mar-2021 DOI: 10.4172/2329-6879.1000340
Abstract
Objective: Severe acute respiratory syndrome (SARS) occurred from November 2002 to June 2003, mainly in Mainland China and Hong Kong. Based on possible reasons which may cause the inflection point in SARS, this commentary discusses experiences in the prevention and control of SARS, and makes enlightening suggestions as to how Corona Virus Disease 2019 (COVID-19) can be effectively contained.
Study design: Factors triggering the inflection point in SARS were analyzed to obtain valuable and reproducible initiatives to contain COVID-19.
Methods: The relationship between the inflection point of SARA and important events and measures that affect the prevalence and control of SARS was analyzed and discussed.
Results: During the campaign against SARS, intervention, attitude, time, seasons and weather were the important factors related to the inflection point. Based on these factors, several countermeasures should be employed in the fight against COVID-19, such as practicing effective intervention and scientific prevention, using experiences in controlling SARS in Beijing as a reference, effectively control of the source of the infection and super spreaders.
Conclusion: Through searching for scientific interventions and taking into valuable experiences available into account, we find out possible reasons which may cause the inflection point for SARS, and make enlightening suggestions for the effective prevention and control of COVID-19. Hopefully, enlightening insights and suggestions will further help contain COVID-19.
Keywords: SARS; Epidemic; Inflection point; Corona Virus Disease 2019
Introduction
Severe acute respiratory syndrome (SARS), emerged at the beginning of the 21st century, although the main battlefield was in China, was a great threat and challenge on the world and to mankind. In the fight against SARS, Chinese government and Chinese people waged an all-out, concerted effort to create scientific and effective countermeasures to deal with the killer epidemic, ushering in an inflection point, finally prevented and controlled the spread of the epidemic in an all-round way. In December 2019, 27 cases of a newlyreported viral pneumonia were first reported in Wuhan, then the infection spread with Wuhan as the center. A new type of coronavirus, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) which was named by World Health Organization (WHO), was isolated from clinical samples on January 7, 2020, and the gene sequence of the virus was then publicized. This commentary discusses possible reasons which may cause the inflection point in SARS, and makes enlightening suggestions for the effective prevention and control of Corona Virus Disease 2019 (COVID-19).
Measures against SARS and Major Progress Achieved
Important Turning Points in SARS
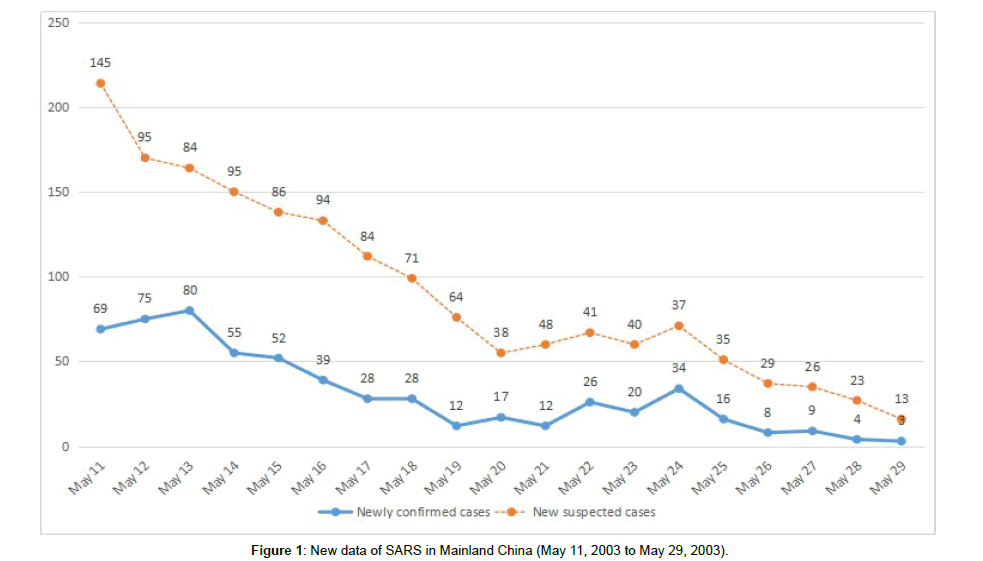
On November 16, 2002, the earliest case of SARS was confirmed in Heyuan, Guangdong, China. The patient’s condition suddenly worsened, showing interstitial pneumonia and acute respiratory distress syndrome, and 8 medical staff were infected during the treatment [1]. The disease, however, was not reported because it was not included in the 35 infectious diseases listed in the Law of the People’s Republic of China on Prevention and Treatment of Infectious Diseases. It became a concern in February 2003 when an outbreak that began in Guangdong [2] spread nationwide with the Spring Festival Travel Rush (when people from all corners of China travel to their hometowns to spend the Chinese Lunar New Year with their families; hereinafter referred to as ‘Chunyun’). The first SARS patient in Hong Kong and Taiwan were then confirmed on February 22 [3] and February 25 [4], respectively. On March 6, SARS landed and then spread rapidly in Beijing [5]. On May 12, newly confirmed cases of China were less than 100 as the inflection point emerged. On may 19th, the number of new cases of SARS in Beijing became less than 10, and 0 case of SARS was reported nationwide on June 4th.
Major Countermeasures for SRAS
For the sudden outbreak of SARS, effective emergency response policies and measures were formulated. First, SARS was added in the Law of the People’s Republic of China on Prevention and Treatment of Infectious Diseases; people in the country were mobilized to make joint efforts in containing SARS. Second, the former Ministry of Health implemented a new system to ensure one report on SARS per day, and ensured that information about SARS was open and transparent. Third, public places, transport and group activities were uniformly supervised. Forth, Xiaotangshan Hospital was built up in time for treating SARS patients. Fifth, persons in close contact with confirmed SARS patients were careful tracked and isolated. Sixth, strict disinfection was conducted, covering places vulnerable to SARS in all corners of the country; various disinfection systems were established. Besides the 6 countermeasures, controlling the source of infection and blocking routes of transmission are particularly important. For example, the first case in Sichuan was transferred from the Center for Disease Control and Prevention (CDC) in Guangdong to CDC in Sichuan, and the patient was immediately isolated and admitted to hospital; and people in close contact with the patient were also isolated and observed, which ensured the ultimate success in the combat against SARS [6]. Effective inspections and monitoring were carried out to locate every suspected SARS patient. Defenses against SARS were constructed. The epidemic reporting system was regulated; and a strict epidemiological investigation and a prevention network were formed to treat suspected cases timely and locally. A family-by-family survey was carried out where the epidemic broke out to ensure that no case was missed. In order to block the route of transmission, we firmly controlled the sources of infection, and strictly grasped any useful information about diagnosed patients, suspected persons in close contact with confirmed SARS patients. Careful disinfection was conducted, and qualified professionals were designated to be responsible for the implementation of systems, procedures, inspections and supervision.
Factors Related to the Inflection Point
Time
SARS lasted for 7 months, from November 26, 2002 to June 2003, centered in Guangdong and Beijing in which about 52% of SARS cases were diagnosed. More than 50 new cases per day were added in Guangdong from February 5 to 10 before Chunyun which further aggravated the situation. The number of patients centered in Guangdong rose to 218 two months after the confirmation of the first case, and to over a thousand four months later. The epidemic then moved to North China, centered around Beijing, for about 40 days. There was a marked increase in new cases on April 19 which peaked on April 29 (more than 100 cases) and began to descend on May 12, all the way down. A number of causes, in which the most important was human intervention, simultaneously changed the trend of SARS epidemic in Mainland China (Figure 1).
Interventions
Human intervention was undoubtedly the most important and decisive factor in creating the inflection point of SARS. In the early stage of SARS, the epidemic spread rapidly because of unclear understanding of the disease, hasty preparation of all aspects, late disclosure of information, insufficient protection for health-care workers (18.8% of the SARS patients were health-care workers) and ineffective human intervention. The second peak in Beijing did not emerge until strict disinfection, isolation, health care protection, management of the vulnerable group, social mobilization and other unprecedented measures were taken. The inflection point came into view about 20 days after the implementation of those interventions which were then carried out all over the country, resulting in good control of the epidemic. Among all the human interventions for SARS, blocking the transmission chain was the most important and effective.
Seasons and weather
SARS basically conforms to the law that the incidence of respiratory infectious diseases increases between winter and spring [7]. A global incident map displaying outbreaks of SARS provided by WHO clearly shows that the steadily high SARS incidence from January to May significantly decreased after mid-May [8]. Temperature and humidity are considered as factors that may affect the transmission of the SARS virus. The temperature in Beijing was lower than usual from January to March in 2003, with an average of 11°C in March and 20.5°C in April. When cold air masses arrived, coronaviruses were likely to spread [9]. Some scholars had analyzed the fluctuation in the daily incidence of SARS since the outbreak in Beijing and the correlation between meteorological factors and the incidence of SARS before inferred that low daytime temperature, low diurnal temperature range and relatively high humidity are beneficial to the spread of SARS [10]. Temperatures in and around Guangzhou in winter range from 5°C to 15°C. The weather is usually cold and rainy when the temperature drops. The temperature recovered rapidly after the beginning of spring, and the average temperature from March to May were 17.7°C, 21.9°C and 25.6°C, respectively. The epidemic peaked in February and March in Guangzhou as well as in April in Beijing, with relatively low peak temperatures in both places. The inflection points of SARS in Guangzhou and that in Beijing were around mid-April and May 10 when the temperature recovered significantly. Therefore, the temperature cannot be excluded from factors affecting the inflection point of SARS.
Attitude
The effect of infection prevention and control can be determined by attitude. Groups and societies are composed of individuals which is the most basic unit of the society. The attitude of individuals will directly or indirectly affect groups and societies, and affect the prevention and control of the epidemic. It is essential for every person to be responsible, proactive, honest and cooperative in containing the epidemic. Everyone in the society was involved in control of the source of infection, the investigation into suspected cases, the observation on persons in close contact with confirmed SARS patients, and in maintaining environmental and personal hygiene and so on. During the outbreak of SARS, CDCs and individuals made concerted efforts to actively participated in disease control and strict disinfection. Checkpoints were set up to check persons in close contact with confirmed SARS patients, which played a positive role of blocking the infection. Also, maintaining a good state of mind during the outbreak of an epidemic, such as being prudent, peaceful, sensible, judicious, will benefit both individuals and the society. Honesty and cooperation are also beneficial to the combat against the epidemic. In the early stage of SARS, the attitude of varied groups and individuals towards epidemic prevention and control is inconsistent, yet it greatly changed as the epidemic developed into the middle and late stage. Social groups, organizations, communities became increasingly responsible, and the fight against the epidemic has been reinforced significantly.
From SARS to Control of COVID-19
SARS and COVID-19
Chinese scientists isolated a new coronavirus, which was named SARS-CoV-2, from clinical samples on January 7, 2020, and published its gene sequence [11]. SARS-CoV-2 is a kind of coronavirus which causes pathogenic pneumonia, and its routes and ways of transmission and pathogenesis are similar as the SARS virus. On January 23, 2020, a preliminary estimate of the virulence (R0) of SARS-CoV-2 published by WHO was estimated between 1.4 to 2.5 which was close to that of the SARS virus in the early stage in 2003 and that of H1N1 flu virus in 2009 [12]. Still, there are similarities and differences between them in many ways, and our understanding of SARS-CoV-2 is far from enough. In view of infection prevention and control and the clinical data, the situation is more complicated and severe than expected. For example, compared with the SARS virus, the transmission rate of SARS-CoV-2 in the population is faster, and the range of transmission is broader; mild and asymptomatic cases bring new difficult problems for containing the pandemic; the source of the virus is still unclear, although recent studies from research institutes such as South China Agricultural University have shown that Manis pentadactyla is the potential intermediate host of SARS-CoV-2; the transmission dynamics and the full spectrum of SARS-CoV-2 are also unknown [13].
Enlightenment from SARS
SARS is both a lesson and a success in human history. For example, a hint was gotten regarding the development and governance of the country during a pandemic. Human beings should live harmoniously with the nature, cherish the environment, protect the nature, and truly achieve scientific, coordinated and sustainable development. In public health crisis management, it is suggested that drawing up strategies at a macro level, coordinating the overall situation, and further planning and constructing public health, from hardware to software, from system to mechanism, to achieve effective response. Promoting health has become a very important issue in the social development. It is an attention-grabbing project which concerns the well-being of people. Relevant personnel training and supporting work must keep up with new needs. Great efforts must be guaranteed to construct a public health team and strengthen the capacity to provide public health services.
Suggestions on Containing COVID-19
Effective intervention is the top priority: Human interventions in the pandemic play a decisive role in the emergence of the inflection point. Effective interventions include two main factors. First, social mobilization, joint defense and control, collective actions, individual responsibility are needed. Second, it is necessary to go all out to block the transmission chain by establishing relevant organizations and organizing personnel in each link to be responsible for the formulation of action plans, coordination, and the implementation of inspection. Importance must be further put in the prevention of the spread of COVID-19 before people get back to work from isolation, which must not be overlooked.
Scientific prevention is one of the effective countermeasures: Scientific prevention can guarantee effective achievements in containing an epidemic. The epidemiological data of SARS cases have shown that SARS tends to be lethal and highly contagious, and is more likely to occur in urban areas and be affected by seasons and aggregation of people [14-17]. These manifestations are directly correlated with the biological characteristics of pathogenic coronaviruses, thus a comprehensive and layered analysis is carried out to formulate corresponding strategies, accelerate basic scientific research and prospective clinical research, and establish a mutual connection between basic and clinical research, including the recognition of the entire disease spectrum, so as to better achieve scientific prevention and treatment of the epidemic [16].
Aerosol and fecal-oral transmission have been intensively studied and ascertained. The importance in clarifying this matter is due to the COVID-19 outbreak. Besides, it is necessary to make people understand varied transmission routes of COVID-19, which is conducive to better prevention and control of the pandemic.
Experiences in controlling SARS in Beijing can be used as a reference: A detailed analysis of the SARS epidemic in Beijing shows that it has gone through five phases [18], importing, ascending, peaking, descending and terminating. The distribution of onset time are characterized by steep and rapid descending after the peak, which is significantly different from that in Hong Kong and Guangzhou in China, and that in Canada [19, 20]. Unlike common infectious diseases, the transmission of SARS did not repeat after the peak, which justifies the effective measures implemented in Beijing during the outbreak. The experiences are replicable and significant. Beijing’s experiences in controlling SARS, including the prevention of repeated outbreaks, deserve to be thoroughly discussed, and scientific prevention and control procedures and methods can be summarized and formulated.
The source of the infection should be controlled: The priority should be given to the control of patients, the source of the COVID-19 pandemic, which is the key to infection prevention and control [21]. In order to support the treatment, it is necessary to open special channels for clinical trials of drugs and strive to find and apply effective drugs as soon as possible. Remdesivir, a new drug, has proven effective in trials in the United States [13], and a phase III clinical trial has been initiated in Wuhan. Relevant departments should pay timely attention to it and other new drugs in clinical trials. Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies, and further follow-up is needed.
Super spreaders should be prevented and controlled: During the SARS outbreak, the super spreaders had a very negative impact on the prevention and control of the epidemic. The emergence of super spreaders may be closely related to the infectiousness and pathogenicity of strains of a virus. A total of 160 patients were infected by a super spreader in Tianjin [20]. Yet Shandong reported that no one was infected when no special protection was taken, although 26 people were in contact with a super spreader [22]. It is of special significance to analyze the causes of super spreaders, and deepen the understanding of the characteristics of a virus and the law of evolution. At the same time, it is necessary to guard against the emergence of super spreaders of COVID-19.
Conclusion
Searches for relevant evidence
By searching PubMed, Cochrane Library, CNKI, CBM, etc., we found 11 systematic reviews and meta-analyses related to the prevention and control of SARS and Middle East respiratory syndrome (MERS). These studies show that there is evidence on the prevention and treatment of SARS and MERS, such as real-time PCR tests for etiological diagnosis, clinical treatment focusing on patients with underlying diseases, and personal protective measures for health care personnel such as personal protective equipment and guidelines for operating procedure. However, there is barely any scientific evidence on vaccines and clinical medication, such as randomized controlled trials of and prospective studies on therapeutic drugs. It is suggested that the clinical research on COVID-19 can focus on serum antibody for neutralizing virus, the efficacy and safety of antiviral drugs, and the reduction of pathological immune response in patients.
About the Inflection Point
The success of the combat against COVID-19 seems promising based on SARS experiences. The inflection point of SARS emerged in less than 70 days after the outbreak in Beijing, in about 5 months in Guangdong, and in less than 6 months nationwide. The time in which the inflection point of COVID-19 in Mainland China occurs is expected to be less than that of SARS in 2003 based on the situation in Beijing and other factors such as nationwide prevention, control and social mobilization. The identification of the pathogen of COVID-19 took 3 months less than that of SARS in 2003. Chinese people willingly minimize personnel contact and social activities as much as possible considering the scale and flow of infected people in Wuhan, which may be a positive and decisive factor in the fight against COVID-19.
Valuable Experiences Available
In the fight against SARS, we have gained valuable experiences and a relatively complete implementation method. The reinforcement of relevant laws also directly or indirectly affect key factors of the prevention and control of the epidemic. All the previously mentioned countermeasures are well applied in the prevention and control of COVID-19, and the expected effects have been achieved. Enlightening insights and suggestions will further help contain COVID-19.
Acknowledgements
Not applicable.
Funding
None.
Availability of Data and Materials
The dataset used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Authors’ Contributions
SZF conceptualized the study, defined the analysis and revised the final version. WX and LWS analyzed the data and drafted the manuscript. MJ and SL contributed to the drafting and revising of the article. All authors read and approved the final version of the manuscript.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
References
- Xiao ZL, Chen SB, HE HQ, Xu YD, Liu XQ, et al. (2003) Infectious atypical pneumonia: the first case report. Xin Yi Xue 34(6):10-12.
- Feng CG. (2003) Development and Academic Progress of SARS (January 2003 to April 19, 2003). Ke Ji Dao Bao. (6).
- Chan-Yeung M, Yu WC. (2003) Outbreak of severe acute respiratory syndrome in Hong Kong Special Administrative Region: case report. BMJ 326:850-852.
- Twu SJ, Chen TJ, Chen CT, Olsen SJ, Lee LT, et al. (2003) Control measures for severe acute respiratory syndrome (SARS) in Taiwan. Emerg Infect Dis 9(6):718-720.
- Huang JH, Zhang WW, Chen LQ, Wang XH, Tan CJ, et al. (2003) Analysis on Infections Status of SARS Contact in Dongcheng Distric. Ji Bing Jian Ce 18(10):371-373.
- Song ZF, Liu G, Wu HY, Wang DZ, Wu XP, et al. (2003) The effective measures to intercept the infection chain of severe acute respiratory syndrome (SARS) in Sichuan province. Zhongguo Xun Zheng Yi Xue Za Zhi 3(2):144-149.
- Neuzil KM, Hohlbein C, Zhu Y. (2002) Illness among school children during influenza season. Archives of Pediatrics and Adolescent Medicine 156(10):986.
- WHO. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Geneva: WHO. 2003
- Zhang YL, Shou Shaowen, Zhang Peng, Chen Tie. (2004) Analysis of characteristics of weather and climate during SARS epidemic. Qi Xiang 30(2):46-49.
- Ye DX, Yang XW, Zhang Q. (2003) Analysis of the relationship between SARS and meteorological conditions in Beijing. Qi Xiang 29(10):42-45.
- Wang C, Horby PW, Haydon FG, Gao GF. (2020) A novel coronavirus outbreak of global health concern. Lancet 395(10223):470-473.
- World Health Organization (2005). Statement on the meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). [EB/OL]. https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov), 2020-01-23/2020-01-29
- World Health Organization (2005). Statement on the meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). [EB/OL]. https://www.who.int/news-room/detail/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov), 2020-01-23/2020-01-29
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, et al. (2020) First Case of 2019 Novel Coronavirus in the United States. NEJM.
- Riley S, Fraser C, Donnelly CA, Ghani AC, Abu-Raddad LJ, et al. (2003) Transmission dynamics of the etiological agent of SARS in HongKong: inpact of public health interventions. Science 300(5627):1961-1966.
- Donnelly CA, Ghani AC, Leung GM, Hedley AJ, Fraser C, et al. (2003) Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 361(9371):1761-1766.
- Dye C, Gay N. (2003) Modeling the SARS Epidemic. Science 300(5627):1884-1885.
- Liang WN, Mi J. (2003) Epidemiological Analysis of SARS in Beijing. Zhonghua Liu Xing Bing Xue Za Zhi 24(12):1096-1099.
- Wang M, Du L, Zhou DH, Di B, Liu YF, et al. (2003) Study on the epidemiology and measures for control on severe acute respiratory syndrome in Guangzhou city. Zhonghua Liu Xing Bing Xue Za Zhi. 24(5):353-357.
- Gully PR. (2003) National response to SARS: Canada. Presentation to WHO global conference on severe acute respiratory syndrome (SARS). Geneva 58:686-689.
- Wang XX, Feng HY, Liu D, Zhang ZL, Shan AL, et al. (2003) Evaluation of epidemic characteristics and main control measures of severe acute respiratory syndrome in Tianjin. Zhonghua Liu Xing Bing Xue Za Zhi. 24(7):565-569.
- Li Z, Wang XJ, Wang M, Lin Y, Ding SJ, et al. (2003) Analysis of serum antibody of SARS and type IV collagen in different populations. Shan Dong Yi Yao. 43(22):5.
Citation: Zhengfang S, Xiao W, Wusong L, Jing M, Li S (2021) Effective Prevention and Control of Corona Virus Disease 2019 (COVID-19): Experiences from Inflection Point for SARS. Occup Med Health Aff 9: 340. DOI: 10.4172/2329-6879.1000340
Copyright: © 2021 Zhengfang S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2710
- [From(publication date): 0-2021 - Dec 12, 2025]
- Breakdown by view type
- HTML page views: 1882
- PDF downloads: 828