Evaluation of the Efficacy of Platelet-Rich Fibrin after Removal of Impacted Mandibular Third Molars: A Systematic Review
Received: 27-Jan-2022 / Manuscript No. johh-22-52525 / Editor assigned: 31-Jan-2022 / PreQC No. johh-22-52525 (PQ) / Reviewed: 14-Feb-2022 / QC No. johh-22-52525 / Revised: 21-Feb-2022 / Manuscript No. johh-22-52525 (R) / Accepted Date: 21-Feb-2022 / Published Date: 28-Feb-2022 DOI: 10.4172/2332-0702.1000299
Abstract
Platelet-rich fibrin (PRF) is the second generation of platelet concentrates collected on a single fibrin matrix that contains various autologous cytokines and immune cells. PRF is extracted from plasma through centrifugation of autologous peripheral blood. Platelet concentrates can be used in alveolar socket to accelerate both soft and hard tissue healing by releasing growth factors. This systematic review aims to evaluate the efficacy of a local application of PRF on postoperative healing after an impacted mandibular third molar extraction. A comprehensive literature search using the advanced features of PubMed, Cochrane Library, and Scopus databases was carried out. 7 study articles accomplished the selection criteria and were included in this review. The results indicated that the local application of autologous PRF in the alveolar socket after impacted mandibular third molar extraction has a beneficial effect on postoperative outcomes. It significantly releases pain, reduces swelling. The increase of growth factors enhances bone healing. Unfortunately, no significant positive effect on postoperative trismus between PRF and control groups was observed in this review
Keywords: Bone healing; pain; Platelet-rich fibrin; Swelling; Tooth extraction
Keywords
Bone healing; pain; Platelet-rich fibrin; Swelling; Tooth
Introduction
The surgical extraction of an impacted third molar is one of the most common surgical procedures performed by oral and maxillofacial surgeons [1]. Impacted third molars, also known as wisdom teeth, need to be extracted if the teeth are symptomatic or diseased, overcrowded, or in abnormal position [2, 3]. The surgical removal of impacted mandibular wisdom tooth results in postoperative inflammatory symptoms, such as pain, swelling, or trismus that reduce the patient’s quality of life [4]. However, in some cases, several postoperative complications, e.g. infection, alveolar osteitis, paresthesia, persistent oroantral communication, hematoma were reported [5]. In addition, the residual amount of alveolar bone usually takes several months to a year to gradually reossify and fill the entire alveolar socket. Several attempts, including platelet-rich plasma, platelet-rich fibrin (PRF) [6], plasma rich in growth factors (PRGF), concentrated growth factors (CGF) [7], propolis extract [8], autogenous dentin [9], G bone (Hydroxyapatite) and G-Graft (Hydroxyapatite with Collagen) [10] administration have been used inside the alveolar socket to reduce postoperative outcomes following mandibular third molar surgery
PRF is the second generation of platelet concentrates collected on a single fibrin matrix that contains various autologous cytokines and immune cells. PRF is extracted from plasma through centrifugation of autologous peripheral blood. Due to the absence of anticoagulant, the blood starts to coagulate as soon as it contacts with the tube surface, and it decreases the time of centrifugation to concentrate fibrinogen [11, 12]. Dr. Joseph Choukroun was the first introduced a PRF for use in oral and maxillofacial surgery in 2001 [11, 12]. Platelet concentrates can be used to accelerate both soft and hard tissue healing by releasing growth factors. PRF is extensively used in oral surgical interventions, such as implantation, dentoalveolar surgery, etc. [13]. Nonetheless, its effect on postoperative healing is still under discussion.
This systematic review aims to evaluate the efficacy of a local application of PRF on postoperative pain, swelling, trismus, and bone healing after an impacted mandibular third molar extraction.
Methods
This systematic review was performed according to Preferred Reporting Items for Systematic Review (PRISMA) guidelines. The following PICO strategy was establishe:
•The participants (P) – healthy adult patients requiring bilateral impacted third molar extraction;
• The intervention (I) – the use of PRF after third molar extraction;
• The comparison (C) – comparison between PRF usage and natural healing in the extraction socket;
• The outcomes (O) – pain, swelling, trismus, and bone healing.
Search strategy
A comprehensive literature search using the advanced features of PubMed, Cochrane Library, and Scopus databases was carried out. The following keywords were used in the search strategy: “plateletrich fibrin“ and “tooth extraction“ and “healing“. The literature search was restricted to articles written in English language and published within the past 5 years, from 2016 to March 2021. No search limitations concerning publication country or status were applied.
Selection Criteria
The inclusion criteria included randomized controlled trials, as well as comparative studies, double-blinded, split-mouth randomized studies, controlled clinical trials, in adult patients that compared the efficacy of a local application of PRF in the extraction socket of mandibular third molar versus natural alveolar socket healing. The patients were older than 18 years old with bilateral impacted mandibular third molars that required surgical extraction.
Any other types of studies, such as case reports, animal research, systematic reviews or meta-analyses, were excluded. Studies that analyzed the effect of PRF versus natural healing in extraction socket of other teeth than mandibular third molars or the comparison of PRF and other biological material as a socket filling in the mandibular third molars also were excluded.
Surgical procedure in selected studies
All surgical procedures were carried out under local anesthesia. An inferior alveolar nerve block was performed with administration of 2% lidocaine with adrenaline in 1:80000 concentrate [14, 15] or 4% articaine with adrenaline in 1:20000 [16]. Other studies [6, 17-19] did not revealed anesthetic used for procedure. Four studies [15-18] used a full thickness three-corned mucoperiosteal flap design while three studies [6, 14, 19] did not specified technique used. Tooth sectioning was performed if needed and the tooth was removed. The alveolar socket was irrigated with saline and the PRF was placed in the study side while the control side were left empty to heal natural. Primary closure of both sides was achieved by suturing with 3-0 [14, 15, 18, 19] or 4-0 [16] black braided silk. Post-extraction instructions were given, and patients were recalled for further follow-ups
PRF preparation
Methods for PRF preparation in included studies are presented in Table 1. A different volume of blood drawn into test tubes was observed in included studies: 5 ml [6], 5 – 10 ml [19], 10 ml [15, 16, 18], and 20 ml [14, 17]. All research did not add any anticoagulant in a test tube. A blood sample was immediately centrifuged mostly at 3000 rpm for 10 min [6, 14, 17, 19] or at 2700 rpm for 12 min [16, 18]. One study used the centrifuge at 3000 rpm for 12 min [15]. A PRF clot, formed in the middle layer, was separated from the red blood cell, and placed in the extraction socket. A lack of information about the actual increase of platelet concentration after the centrifugation process was observed.
| Authors, Year | Volume of blood drawn, ml |
Centrifugation parameters: speed; time | Centrifugation system |
|---|---|---|---|
| Doiphode et al. 2016 | 5 | 3000 RPM; 10 Min | NR |
| Revathy et al. 2018 | 20 | 3000 RPM; 10 Min | NR |
| Dar et al. 2018 | 10 | 3000 RPM; 12 Min | Table-top centrifuge |
| Asutay et al. 2017 | 10 | 2700 RPM; 12 Min | NR |
| Jeyaraj et al. 2018 | 20 | 3000 RPM; 10 Min | Table-top centrifuge |
| Kapse et al. 2018 | 10 | 2700 RPM; 12 Min | A bench-top centrifuge (R-4C DX, REMI; Mumbai, India) |
| Varghese et al. 2017 | 5 – 10 | 3000 RPM; 10 Min | Remi R 23, Remi Laboratories |
| Min = Minutes; NR = Not Reported; RPM = Round Per Minute | |||
Table 1: Methods for PRF preparation in included studies.
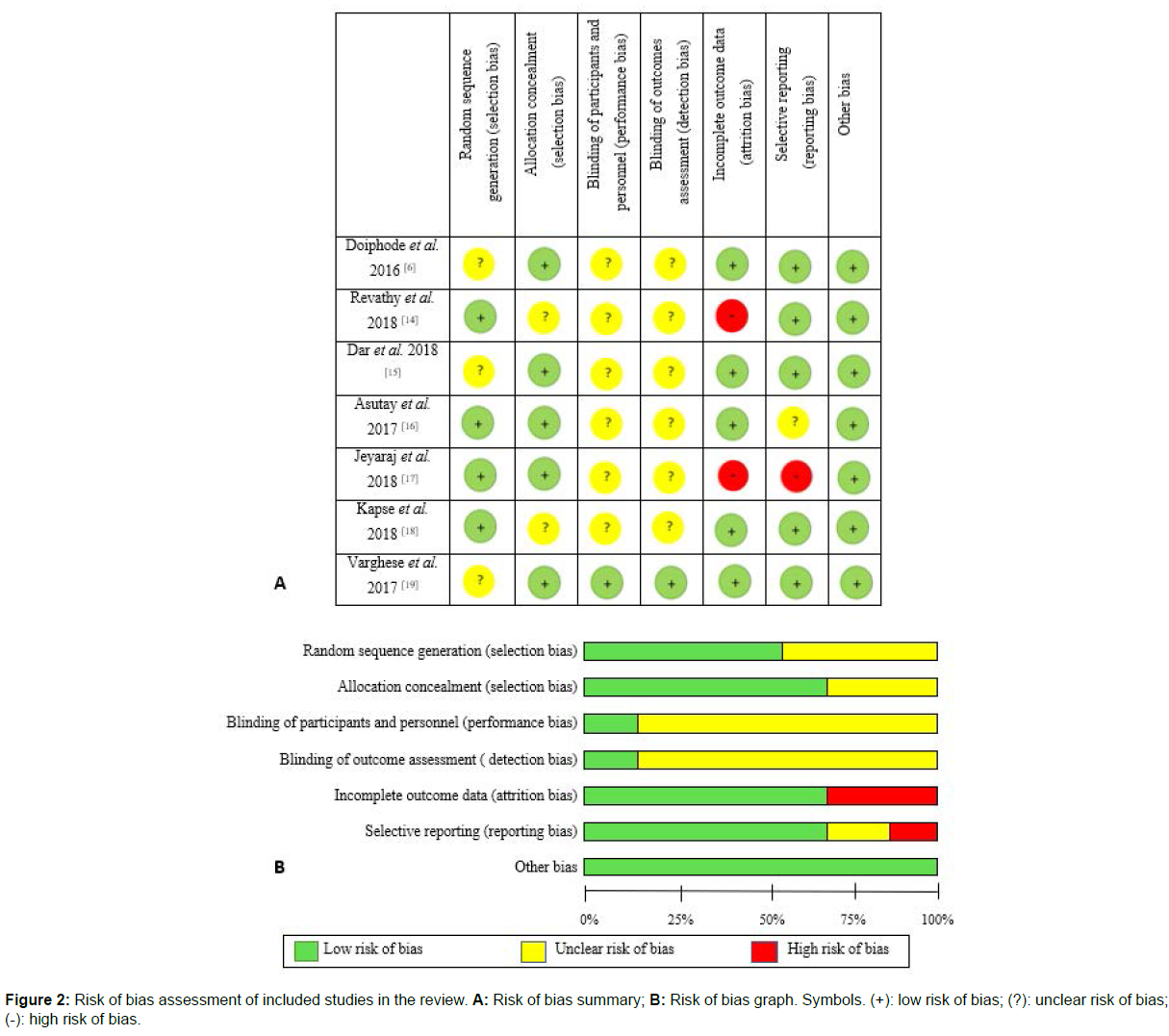
Quality assessment
The Cochrane Collaboration’s tool for assessing risk of bias was used to evaluate the quality of the selected studies. A total of seven domains were analyzed: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential threats to validity. Each component was classified as low-risk, unclear-risk, or high-risk.
Results
Study selection
The electronic and manual search of literature yielded 572 articles, of which 27 were duplicates and were excluded. A total of 545 articles were included in title and abstract screening. After the eligibility process 45 records were obtained and the full text of the related studies was read. Finally, a total of 7 articles fulfilled all necessary inclusion criteria in this systematic review. The publication years varied from 2016 to2021. The included studies were quantitatively and qualitatively analyzed. A search strategy was presented in PRISMA flow diagram Figure 1. The main characteristics of included studies are summarized in Table 2.
| Authors, Year | Follow-up visits | Pain | Swelling | Trismus | Bone healing |
|---|---|---|---|---|---|
| Doiphode et al. 2016 | 2nd, 4th, 6th months | - | - | - | Alveolar bone height (ABH) distal to 2nd molar preoperatively and 2 months postoperatively was higher in the PRF group, but in the control group it was higher on 4th and 6th months. The mean score of bone density was higher in the PRF group at all-time intervals comparing with the control group and it gradually increased in both groups (P<0.05). |
| Revathy et al. 2018 | 1st, 3rd, 6th months | - | - | - | More radio density was noted on PRF group compared with the control group at all-time intervals (P=0.061 and P=0.000 on 1st and 3rd, 6th months respectively). |
| Dar et al. 2018 | 1st, 3rd, 7th, 14th days, 4th and 12th weeks | The first day was evaluated as the most painful in both groups and a gradual decrease was observed (P<0.05). | The PRF group showed lower percentage of swelling at all points of time (P<0.05), but it was higher on the 1st postoperative day in both groups. | - | The bone healing score increased in both groups on 4th and 12th weeks, but it was higher in the PRF group (P<0.001). |
| Asutay et al. 2017 | 6th, 12th hours, 1st-7th days | The PRF group showed higher pain value at all points of time comparing with the non-PRF group (P>0.05). | The swelling score was higher in the control group on day 2, and in the PRF group it was higher on 7th day (P>0.05). | The higher trismus score was in the control group on both 2nd and 7th days comparing with the PRF group (P>0.05). | - |
| Jeyaraj et al. 2018 | Immediately after procedure, 3rd day, 2nd, 4th, 6th months | The mean pain score at day 3 was lower for the control group (P=0.009 and P=0.004 respectively). | The postoperative swelling was observed mostly as moderate and nil in the control and study groups respectively on day 3 (P<0.05). | The postoperative trismus occurred more in the control group than in the PRF group on 3rd day (P<0.05). |
A faster bone regeneration was noted in the PRF group within 8 weeks postoperatively (P<0.05). |
| Kapse et al. 2018 | 1st, 3rd, 7th, 14th days, 8th and 16th weeks | The postoperative pain level was lower for the PRF group during all follow-ups. (P<0.05). |
The facial swelling percentage was higher on day 3 in control group and gradually reduced over 14 days in both groups (P<0.05). | - | A better bone healing score was noticed in both groups at the 16th week compared with the 8th week (P<0.001). |
| Varghese et al. 2017 | 1st, 4th, 16th week | - | - | - | The mean bone healing percentage was significantly higher in the PRF group (P<0.05). |
Table 2: Characteristics of included studies.
Characteristics of included studies
Five of the studies were comparative; two of the studies were randomized clinical trials, including one double-blinded, split-mouth study. A total of 265 patients with ages ranging from 18 to 50 were included in the studies.
Risk of bias assessment
All 7 included studies were evaluated qualitatively by the tools of Cochrane Collaboration for the risk of bias (Figure 2). Two studies [14, 17] had a high risk of bias in incomplete outcome data (patients did not appear for follow-ups due to uncertain reasons [14] or the outcome was only mentioned not described in the article [17]). A high risk of bias in selective reporting was observed only in a study by Jeyaraj et al. [17]. The highest proportion of low risk of bias included other bias, allocation concealment, incomplete outcome data, and selective reporting. Meanwhile, blinding of participants and personnel, and blinding of outcome assessment were noted as the highest proportion of unclear risk bias.
Pain
Four articles [6, 16-18] analyzed postoperative pain levels at different time intervals after surgical extraction. The pain was evaluated using visual analogue scale (VAS). Two studies [15, 18] presented statistically highly significant reductions in pain (P<0.01) in the PRF group compared with the non-PRF group on the first post-operative day. However, a study by Asutay et al. [16] showed no statistically significant effect of PRF in pain one day after the surgery, even though the mean pain score was higher on the PRF group (27.35±31.70 and 22.20±21.70 respectively). A favorable effect of PRF (P<0.05) on the 3rd day was seen in the fourth study that evaluated the post-operative pain [17] and the mean pain score was lower on the study group comparing with the control group (15±1.009 and 33±1.179 respectively). Cases of gradual decrease in postoperative pain in both groups during follow-ups after 1-14 days were found in three articles [15, 16, 18] of four that analyzed postoperative pain. Kapse et al. [18] and Dar et al. [15] established that the correlations among the age, gender, and type of impaction in both groups were not statistically significant.
Swelling
Four articles [15-18] analyzed postoperative swelling percentage at different time intervals after surgical extraction. The swelling wasevaluated by measuring the distances from the tragus to the soft tissue pogonion in three studies [15, 17, 18]. The 3dMD system (it uses a synchronized digital multicamera configuration, with three cameras on each side to capture 180° facial images from ear to ear) was only used in a study by Asutay et al., [16] where the preoperative image was taken immediately before the surgery and postoperative images were taken on 2nd and 7th days. A favorable effect of PRF (P<0.05) was presented in three articles [15, 17, 18]. A study by Kapse et al. [18] established that the facial swelling percentage was significantly higher on the control group at 3rd postoperative day (8.80 ± 0.51 and 5.16 ± 0.32 respectively). Dar et al. [15] reported a gradual reduction in swelling in both groups at all points of time but the mean scores were lower in the PRF group, and a highly significant difference (P<0.001) was observed. A degree of swelling was measured by Jeyaraj et al. [17] only on the 3rd day after surgery and it was established that 19 patients out of 30 evaluated the postoperative swelling as a nil in the PRF group while 14 patients out of 30 evaluated it as a moderate in the control group and it was statistically significant. Interesting that statistical analysis of Asutay et al. study [16] showed no significant difference for postoperative swelling (P>0.05) between both groups on 2nd (P=0.94) and on 7th (P=0.27) days.
Trismus
Only two articles [16, 17] analyzed postoperative trismus. The methods of measuring the trismus were not mentioned in Jeyaraj et al. [17] study, and it was evaluated only on the 3rd postoperative day. The number of patients who indicated a postoperative trismus on the PRF and control groups were 6 and 21 respectively out of 30 in each group and a statistically significant difference was observed. The other research was conducted by Asutay et al. [16] in Turkey and it evaluated the difference of the measurements of the maximal inter-incisor opening distance preoperatively and on 2nd and 7th postoperative days but there was no statistically significant difference in mouth opening comparing PRF and control groups.
Bone healing
Four researches [6, 17-19] used an intraoral periapical radiograph (IOPAR), Revathy et al. [14] used an orthopantomogram (OPG) while Dar et al. [16] used both methods of measurement to evaluate the postoperative bone regeneration.
The score of bone density was assessed in six studies [6, 14-19]. Two studies showed a highly significant increase in bone density: Dar et al. [15] revealed a favorable effect of PRF in 25 patients out of 30 in the PRF group and only in 4 patients of 30 in the control group on the 4th week, and a study by Kapse et al. [18] indicated higher bone density score in the PRF group on the 16th postoperative week (1.83±0.07 and 0.63±0.09 respectively) compared with the 8th week (1.23±0.09 and 0.27±0.08 respectively). The new bone formation observed by Doiphode et al. [6] was encouraged by PRF when compared with control group on 2 (120±8.42 and 75.87±8.38 respectively), 4 (133.7±9.30 and 99.94±14.91 respectively), 6 months postoperative (141.4±11.41 and 127.80±11.87 respectively) and it was statistically significant (P<0.05). In a study by Revathy et al. [14] more radio density was obtained on the PRF group at all points of time. A highly significant difference was noted only on the 3rd and 6th postoperative months (P=0.000). Moreover, the regions of newly formed bone were evaluated on 1st, 4th, and 16th weeks and represented in a study by Varghese et al. [19] The mean values were significantly higher (P<0.05) in the PRF group compared with the non- PRF group (64.73±24.411 and 53.67±16.528 respectively). A study by Jeyaraj et al. [17] evaluated the overall bone density score at the end of 8 weeks and a statistically significant difference was obtained in the PRF group.
Assessing postoperative bone healing by the score of trabecular pattern, Kapse et al. [18] established a highly significant difference (P<0.001) comparing the PRF and control groups on both 8th (1.20±0.11 and 0.30±0.09 respectively) and 16th (1.87±0.06 and 0.50±0.09 respectively) weeks. A statistically significant difference (P<0.001) in trabecular pattern score in the study by Dar et al. [15] was obtained in 28 patients out of 30 in the PRF group and in 10 of 30 patients in the non-PRF group on week 4. Jeyaraj et al. [17] compared and evaluated the trabecular pattern score at the end of 8th week and a favorable effect of PRF was noticed (2.43±0.626 on the PRF and 0.8±0.61 on the control groups).
Two studies evaluated the score of lamina dura. Kapse et al. [18] observed an increased number of bone healing parameters in the PRF group compared with the control group on both 8th (1.23±0.10 and 0.40±0.09) and 16th (1.80±0.07 and 0.90±0.12) weeks (P<0.001). Evaluating the efficacy of PRF on lamina dura score in a study by Dar et al. [15] a significant increase (P<0.001) was reported in the study group on week 4 compared to the week 12.
The results of the alveolar bone height (ABH) were analyzed in a study by Doiphode et al. [6]. A significant decrease (P<0.05) of ABH was observed in the PRF group compared with the control group on 4th (1.93±0.23 and 3.20±0.33 respectively) and 6th (1.29±0.33 and 2.99±0.34 respectively) months
Discussion
Pain, swelling, and trismus are commonly reported symptoms negatively affecting patients’ quality of life during the postoperative period after third molar extraction [20]. Therefore, many attempts have been made to reduce consequences after surgical removal. The extensive use of platelet concentrates to promote healing containing high quantities of growth factors is observed in oral and maxillofacial surgery [13]. PRF, being a rich source of growth factors, is a potential biomaterial for enhancing soft tissue healing and bone regeneration. PRF is obtained with a simplified preparation using no anticoagulants or bovine thrombin and providing a sustained release of growth factors, such as platelet derived growth factors, vascular endothelial growth factor, epidermal growth factor, transforming growth factor – beta, thrombospondin–1 [21].
The influence of PRF to postoperative pain, swelling, trismus, and bone healing after impacted mandibular third molar extraction was observed in the present review. Kumar et al. [22] indicated results claiming that pain was significantly higher on control group on the first postoperative day, whereas 20% complained of severe pain, 40% slight pain, and 40% mild pain. These data match the findings of Dar et al. [15] and Kapse et al. [18] who presented statistically significant reduction of pain in PRF group compared with the control group (P < 0.01) on postoperative day 1.
A clinical trial published in 2018 by Daugela et al. [23] showed statistically higher results of postoperative swelling values in the group with naturally healing socket during the first postoperative week compared with a L-PRF group. Previously discussed studies by Dar et al. [15], Jeyaraj et al. [17], and Kapse et al. [18] indicated a favorable effect of PRF application in the extraction socket of mandibular third molars resulting in less postoperative swelling compared with the control group. Furthermore, Torul et al. [24] analyzed the effect of CGF and advanced platelet-rich fibrin (A-PRF) on pain, swelling, and trismus after third molar surgery. These biomaterials are considered more advanced comparing with PRF due to higher bioactive potential, releasing more growth factors, including a greater number of white blood cells, obtaining softer fibrin clot using low-speed centrifugation. The results of a study by Torul et al. [24] showed that CGF and A-PRF negatively affect postoperative outcomes after extraction due to increased amount of white blood cells. Various difficulty levels of surgeries or lack of accuracy may be a cause for controversial results.
Unfortunately, the effect of PRF on postoperative morbidities of the impacted third molar extraction can be controversial. Oral and Maxillofacial surgeries may cause the spam of some muscles, especially masseter [16]. A study by Uyanik et al. [25] reported that a local application of PRF has no positive effect on mouth opening compared with a natural healing following the surgical extraction of impacted third molars. In the present study, a clinical trial published in 2018 by Asutay et al. [16] also did not find a significant effect of PRF on postoperative trismus after wisdom teeth removal. Both studies evaluated trismus by measuring the distance between the mesial incisal corners of the upper and lower right incisors during maximum mouth opening on 2nd and 7th postoperative days. According to the findings of these studies, there was no statistically significant differences on trismus scores among both PRF and control groups.
In 2019 a study by Areewong et al. [26] stated that less new bone formation in the extraction socket was observed in the control group 8 weeks after tooth extraction compared with a PRF group. However, in this review Kapse et al. [18] revealed higher bone healing scores in the PRF group on the 8th postoperative week (P < 0.001). Sustained and extensive release of growth factors is responsible for increased quality of newly formed bone.
The results of the articles may be affected not only by the biomaterials with which the alveolus is filled, but also by the surgical process. For instance, different flap designs play an important role in the Citation: Pliatkute I, Petronis Z, Gervickas A (2022) Evaluation of the Efficacy of Platelet-Rich Fibrin after Removal of Impacted Mandibular Third Molars: A Systematic Review. J Oral Hyg Health 10: 299. Page 6 of 6
J Oral Hyg Health, an open access journal Volume 10 • Issue 2 • 1000299 postoperative outcomes after wisdom tooth removal. Hassan et al. [27] noted that the pain score was significantly lower on the lingual-based four-cornered flap group compared with the conventional triangular flap group (P<0.05). Different flap design was used in previously discussed studies [15-18] which may cause a reduction of accuracy comparing the results.
PRF is successfully used as a healing agent inside the alveolar socket, but the main limitations are related to the small sample sizes, different scales of measurement, different surgical protocols, and different periods of follow up visits. In addition, this systematic review did not include non-English language studies, any formulations of PRF and animal experiments. In the future, further well-design studies with a larger sample size are required to prove the efficacy of biological materials to alveolar socket healing after impacted mandibular third molar extraction.
Conclusions
The local application of autologous PRF in the alveolar socket after impacted mandibular third molar extraction has a beneficial effect on postoperative outcomes. It significantly relieved pain, reduced swelling. The increase of growth factors enhanced bone healing. Unfortunately, no significant positive effect on postoperative trismus between PRF and control groups was observed in this review
Running head
PRF effect after third molar extraction.
Funding sources
None declared.
Conflict of interests
None declared.
References
- KalaiSelvan S, Ganesh SKN, Natesh P, Moorthy MS, Niazi TM, et al. (2020) Prevalence and pattern of impacted mandibular third molar: An institution-based retrospective study. J Pharm Bioallied Sci 12: 462.
- Zhang Y, Chen X, Zhou Z, Hao Y, Li H, et al. (2021) Effects of impacted lower third molar extraction on periodontal tissue of the adjacent second molar. Ther Clin Risk Manag 17: 235-247.
- Haddad Z, Khorasani M, Bakhshi M, Tofangchiha M, Shalli Z (2021) Radiographic position of impacted mandibular third molars and their association with pathological conditions. Int J Dent 2021:1-11
- Ruiz-Roca JA, Donoso-Martínez B, Ameneiros-Serantes S, Martínez-Beneyto Y, Salmerón-Martínez D, et al. (2020) Influence of operator’s professional experience in the postoperative course after surgical extrac-tion of the impacted lower third molar: A pilot study. J Clin Exp Dent 12: e805-e812.
- Chen YW, Chi LY, Lee OKS (2021) Revisit incidence of complications after impacted mandibular third molar extraction: A nationwide population-based cohort study. PloS one 16: e0246625.
- Doiphode AM, Hegde P, Mahindra U, Kumar SS, Tenglikar PD, et al. (2016) Evaluation of the efficacy of platelet-rich plasma and platelet-rich fibrin in alveolar defects after removal of impacted bilateral mandibular third molars. J Int Soc Prev Community Dent 6: 47-52.
- Özveri Koyuncu B, Isik G, Özden Yüce M, Günbay S, Günbay T (2020) Effect of concentrated growth factors on frequency of alveolar Osteitis following partially-erupted mandibular third molar surgery: a randomized controlled clinical study. BMC Oral Health 20: 1-8.
- González-Serrano J, López-Pintor RM, Cecilia-Murga R, Torres J, Hernández G, et al. (2021) Application of propolis extract, nanovitamin C and nanovitamin E to prevent alveolar osteitis after impacted lower third molar surgery. A randomized, double-blind, split-mouth, pilot study. Med Oral Patol Oral Cir Bucal 26: e118-e125.
- Sánchez-Labrador L, Martín-Ares M, Ortega-Aranegui R, López-Quiles J, Martínez-González JM (2020) Autogenous dentin graft in bone defects after lower third molar extraction: A split-mouth clinical trial. Materials 13: 3090.
- Panday V, Upadhyaya V, Berwal V, Jain K, Sah N, et al. (2015) Comparative evalution of G bone (hydroxyapatite) and G-graft (hydroxyapatite with collagen) as bone graft material in mandibular III molar extraction socket. J Clin Diagn 9: ZC48- ZC52.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, et al. (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: e37-e44.
- Naik B, Karunakar P, Jayadev M, Marshal VR (2013) Role of Platelet rich fibrin in wound healing: A critical review. J Conserv Dent 16: 284-293.
- Al-Hamed FS, Mahri M, Al-Waeli H, Torres J, Badran Z, et al. (2019) Regenerative effect of platelet concentrates in oral and craniofacial regeneration. Front Cardiovasc Med 6: 126.
- Revathy NS, Kannan R, Karthik RS, Kumar MS, Munshi MAI, et al. (2018) Comparative study on alveolar bone healing in postextraction socket versus healing aided with autologous platelet-rich fibrin following surgical removal of bilateral mandibular impacted third molar tooth: A radiographic evaluation. Natl J Maxillofac Surg 9: 140-146.
- Dar MM, Shah AA, Najar AL, Younis M, Kapoor M, et al. (2018) Healing potential of platelet rich fibrin in impacted mandibular third molar extraction sockets. Ann Maxillofac Surg 8: 206-213.
- Asutay F, Yolcu ÜMIT, Geçör O, Acar AH, Öztürk SA, et al. (2017) An evaluation of effects of platelet-rich-fibrin on postoperative morbidities after lower third molar surgery. Niger J Clin Pract 20:1531-1536.
- Jeyaraj PE, Chakranarayan A (2018) Soft tissue healing and bony regeneration of impacted mandibular third molar extraction sockets, following postoperative incorporation of platelet-rich fibrin. Ann Maxillofac Surg 8: 10-18.
- Kapse S, Surana S, Satish M, Hussain SE, Vyas S, et al. (2019) Autologous platelet-rich fibrin: can it secure a better healing? Oral Surg Oral Med Oral Pathol Oral Radiol 127: 8-18.
- Varghese MP, Manuel S, LK SK (2017) Potential for osseous regeneration of platelet-rich fibrin-A comparative study in mandibular third molar impaction sockets. J Oral Maxillofac Surg 75: 1322-1329.
- Gülsen U, Sentürk MF (2017) Effect of platelet rich fibrin on edema and pain following third molar surgery: a split mouth control study. BMC Oral Health 17: 1-6.
- Alzahrani AA, Murriky A, Shafik S (2017) Influence of platelet rich fibrin on post-extraction socket healing: A clinical and radiographic study. Saudi Dent J 29: 149-155.
- Kumar N, Prasad K, Ramanujam L, Ranganath K, Dexith J, et al. (2015) Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg 73: 1042-1049.
- Daugela P, Grimuta V, Sakavicius D, Jonaitis J, Juodzbalys G (2018) Influence of leukocyte-and platelet-rich fibrin (L-PRF) on the outcomes of impacted mandibular third molar removal surgery: A split-mouth randomized clinical trial. Quintessence Int 49: 377-388.
- Torul D, Omezli M M, Kahveci K (2020) Evaluation of the effects of concentrated growth factors or advanced platelet rich-fibrin on postoperative pain, edema, and trismus following lower third molar removal: A randomized controlled clinical trial. J Stomatol Oral Maxillofac Surg 12: 646-651.
- Uyanik LO, Bilginaylar K, Etikan I (2015) Effects of platelet-rich fibrin and piezosurgery on impacted mandibular third molar surgery outcomes. Head Face Med 11: 1-7.
- Areewong K, Chantaramungkorn M, Khongkhunthian P (2019) Platelet-rich fibrin to preserve alveolar bone sockets following tooth extraction: A randomized controlled trial. Clin Implant Dent Relat Res 21:1156-1163.
- Hassan B, Al-Khanati NM, Bahhah H (2020) Effect of lingual-based flap design on postoperative pain of impacted mandibular third molar surgery: Split-mouth randomized clinical trial. Med Oral Patol Oral Cir Bucal 25: e660-e667.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Pliatkute I, Petronis Z, Gervickas A (2022) Evaluation of the Efficacy of Platelet-Rich Fibrin after Removal of Impacted Mandibular Third Molars: A Systematic Review. J Oral Hyg Health 10: 299. DOI: 10.4172/2332-0702.1000299
Copyright: © 2022 Pliatkute I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7913
- [From(publication date): 0-2022 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 7104
- PDF downloads: 809