Functioning and Physical Activity after Spinal Cord Injury.
Received: 06-Sep-2017 / Accepted Date: 14-Sep-2017 / Published Date: 25-Sep-2017 DOI: 10.4172/2329-6879.1000265
Abstract
Background: Spinal cord injury (SCI) causes medical disorders and loss of functions, independence and physical activity in daily and social life. Primary inpatient rehabilitation after SCI onset is more focused on improving the physical state, physical capacity or developing functional independence and mobility skills. In long-term periods the functioning and socialization processes of people with SCI are improving each year naturally engaging and participating in various areas of everyday life.
Objectives: The functioning and physical activity of people with SCI in different period of life: during inpatient SCI rehabilitation, after discharge in the long-term context (1–24 years after SCI on set).
Material and Methods: A total of 194 people with SCI were participated in the research during 2007–2015. The study was carried out during inpatient rehabilitation in the Centre of Rehabilitation, Physical and Sports Medicine and during independent life skills and recreation camps in the Landscape Therapy and Recreation Centre (Palanga). Functional problems were assessed by the Comprehensive ICF Core Set for SCI. Socio-demographic characteristics, physical activity in everyday life in different periods after SCI onset were collected by a brief form of the Life Situation Questionnaire-revised.
Results: SCI more often experienced young men, up to 34 years of age unmarried and having special or higher education. Prevailed traumatic, in thoracic level and AIS A type SCI. People with SCI actively participated in labour market: during 1–5 years after SCI employed participants increased from 17.8% to 30.2% and in subsequence periods increased significantly to 35.8% (p<0.05). In different period prevailed jobs at home, works to order and shortterm jobs. The comprehensive inpatient rehabilitation statistically significant improved activities and participation skills, especially in solving problems, mobility and self-care, but physical activity in everyday life more increased in 1–5 years period: participants more spent time in a wheelchair, actively participated in sports and household chores, more often went outside of the house and went out to manage social matters or to entertain.
Conclusion: During inpatient rehabilitation precisely solved problems, favourable social conditions, promoted physically active lifestyle, assurance of social support and state policy could ensures successful functioning and better physical activity in everyday life and community in long-term context of people with SCI.
Keywords: Spinal cord injury; Functioning; Physical activity; Employment; Participation in daily life
Background
According to the data of Lithuanian Department of Statistics there are 140 new cases of spinal cord injury (SCI) every year in Lithuania [1]. SCI mainly occur for active, independent young people (34.18 ± 14.19), about 75% were male. The most common causes of SCI in Lithuania are: car and motorcycle accidents (40.1%), falls from height (20%), diving in shallow water (12.8%), especially in the wormer time of the year, and diseases or medical complications causing spinal cord injuries (39.1%) [2].
SCI cause enormous changes in biopsychosocial life: physical, psychological and social functioning is determined by the interaction between health conditions and factors related to personal and environmental aspects. Personal aspects include features of health condition, physical and functional state. Environmental aspects include physical, social and attitudinal factors that can facilitate or hinder an individual's performance [3,4]. SCI induce health condition changes related injury: severity of the lesion reduced physical capacity and activity due to body dysfunctions [5,6]. Changes of physical and functional state cause the functional problems leaded activities limitations and participation restrictions typically related to mobility, self-care, household and leisure activities, employment difficulties, maintaining social relationships and being active members of the community [7,8]. Activity in daily life and community reintegration has a positive effect on quality of life of people with SCI and their families: providing financial security, environment for social interaction, selfesteem, confidence and independence [9,10].
Functional outcomes of people with SCI are essential to formulating a rehabilitation plan, which are determined based on the level of SCI, age, sex, medical comorbidities, motivation and family support. Rehabilitation begins in the intensive care setting and includes addressing the SCI – specific needs to help each person meet his/her potential in terms of medical, physical, social, emotional, recreational, vocational, and functional recovery. But one of the primary goals of the early recovery period of rehabilitation is to convey that life with an SCI can be fulfilling and ensure the further functioning in daily life after discharge and in long-term context. Functional goals expected for a person with SCI during rehabilitation and after discharge also depend of biopsychosocial variables: functioning restriction, activity limitations in daily life caused the medical comorbidities, recourses of physical and social environment, family support, occupations opportunities [11-13]. The prevalence of many functional problems associated with SCI may verify within the phase of treatment, rehabilitation period and the time after SCI onset [14,15]. That is very important to identify the impaired functioning and activity limitations during inpatient rehabilitation, after discharge and in long-term context for assessing personal functional problems and disability, vocational rehabilitation expectations and occupations opportunities [10,16].
Numerous physical status measures are used to assess the functional limitations associated with SCI. However, most of these measures cover only selected aspects of the whole SCI health experience and considerably regarding their content and psychometric characteristics. Mostly during inpatient rehabilitation for assessing rehabilitation outcomes and effectiveness were used mobility and daily activities assessing [2,3,17], but none of them can be considered as a standard and none of them covers all aspects of functioning and physical activity in long-term context [4,18,19]. It is very important comprehensively assess functioning and disability, to identify the prototypical spectrum of functional problems associated with personal daily and social life, occupations and activities issues that people with SCI could experience in real life after rehabilitation in 1, 5, 10 and more years [10,20].
The objective of this cross-sectional study was to evaluate the prevalence of problems in functioning and daily life activity experienced by people with SCI during inpatient rehabilitation and after discharge in a long-term context (1–24 years after SCI).
Material And Methods
Study design
The study was performed during multidisciplinary inpatient rehabilitation at the Rehabilitation, Physical and Sports Medicine Centre, Vilnius University Hospital Santaros Clinic during 2011–2015. Also, in cooperation with the Lithuanian Paraplegics Association people with SCI in a long-term context (from 1 to 24 years after SCI onset) were included in the research. The research data were collected by rehabilitation team members (occupational therapists and physiotherapists).
The research is one of the first in Lithuania investigating functioning, activity in daily life and occupations of people with SCI in different life periods (inpatient rehabilitation and after discharge from rehabilitation in a long-term context 1–24 years after SCI). To obtain more detailed data about socio-demographic characteristics and occupations of people with SCI, Life Situation Questionnaire-revised (LSQ-r, JS Krause) were used [6,18,21,22]. For evaluation of functional problems, activities and participation in daily life, ICF Core Sets for Spinal Cord Injury were used [3,4,8,14]. The study was based on ethical, privacy and confidentiality principles.
Study population
In total, 194 people with SCI participated in the research study:
1) 56 (28.9%) people after SCI onset were involved in the research during a multidisciplinary inpatient rehabilitation: in the acute period of rehabilitation (2–4 weeks post-injury); the recovery period (2 weeks to 6 months post-injury); the chronic period (6 months to 1 year’s post-injury). The biopsychosocial variables were evaluated twice: at the admission to rehabilitation and at discharge.
2) 138 (71.1%) people with SCI in the long-term context (from 1 to 24 years after SCI onset) were involved in the research during independent life skills and recreation camps in the Landscape Therapy and Recreation Centre (Palanga).
The inclusion criteria were: (I) age of 18–59 years, (II) traumatic or non-traumatic SCI, (III) AIS A, B and C SCI level, (IV) stable health status, and (V) voluntary participation, confirmed by a signature in the informed consent.
The exclusion criteria were as follows: (I) age of more than 60 years, (II) the high SCI level – cervical C1-C4 level and/or above it, (III) AIS D and E SCI level, (IV) oncological diseases, and (V) unstable health status.
For evaluation of biopsychosocial variables and identification the main functional problems, the participants were divided into groups according the type of SCI lesion:
(A) Participants during the inpatient rehabilitation (n=56): tetraplegia–23 (41.1%), paraplegia–33 (58.9%): 16 (48.5%) of them were injured in the Thoracic level, 17 (51.5%) in the Sacral/Lumbar level.
(B) Participants in the long-term context (n=138): tetraplegia–68 (42.3%), paraplegia–70 (50.7%): 43 (61.4%) of them were injured in the Thoracic level, 27 (38.6%) in the Sacral/Lumbar level.
For analyses of functional outcomes and physical activity in different periods of life, the participants were divided into groups according to time since SCI onset (Table 1): Group I represents data of participants during an inpatient rehabilitation period; Group II represents data of participants in a long-term context 1–5 years after SCI; Group III represents data of participants in a long-term context 5–10 years after SCI; Group IV represents data of participants more than 10 years after SCI. Participants in Group I significantly differed from the groups of long-term context regarding age, SCI severity, setting, time since SCI onset, non-traumatic etiology, functional problems, activities and participation in daily and social life.
| SCI level | Group I | Group II | Group III | Group IV |
|---|---|---|---|---|
| Inpatient rehabilitation (n=56) | 1–5 years after SCI (n=51) |
5–10 years after SCI (n=40) |
>10 years after SCI (n=47) |
|
| Tetraplegia | 23 (41.1%) | 34 (66.7%) | 16 (40.1%) | 16 (34.1%) |
| Paraplegia | 33 (58.9%) | 17 (33.4%) | 24 (59.9%) | 31 (65.9%) |
Table 1: Participants distribution in groups according to time since SCI onset (n=194).
Ethical issues
Ethical approval was obtained from the Lithuanian Bioethics Committee (protocol No. 1.17/3/2011). All the participants provided written informed consent at initial assessment. Participants were required to consent to complete the questionnaire and undergo a brief examination of functional status as well as evaluation of functional problems and functioning level in activities of daily living.
Instruments
In order to analyze the functional problems, activities and participation in daily life of people with SCI during inpatient rehabilitation and after discharge from rehabilitation in long-term context, a research protocol was prepared. This protocol included the assessment of the data collected on the participant’s clinical state, socio-demographic characteristics, functioning and activity in daily life.
Clinical state: Clinical state was assessed in accordance to the SCI neurological level, localization and type. The participant’s spinal cord motions and sensory function was assessed according to the American Spinal Injury Association (AIS) Classification. According to the SCI level the participants were divided into 3 groups: 1) SCI in the cervical level (C4-C8 spinal segment); 2) SCI in thoracic level (Th1-Th12 spinal segment); 3) SCI in the lumbar level (L1-L5 spinal segment).
In order to determine the main functional problems, activities and participation limitations in daily life of people with SCI during different periods of life, biopsychosocial functions were evaluated during inpatient rehabilitation and in the long-term context during independent life skills camps, the participants were evaluated once.
Socio-demographic characteristics and activity in daily life: We analyzed the socio-demographic characteristics, social data, and physical activity in everyday life in different periods after SCI. Also we assessed the participant’s subjective opinion about the extent of the different areas or activities in which there are more problems. We used a brief form of the Life Situation Questionnaire-revised (LSQ-r) – the electronic version and official permission was received from PhD James S. Krause, The Department of Rehabilitation Sciences, Medical University South Carolina), which included information about participants’ socio-demographic characteristics – age, sex, living place adaptation, education, participation in study, employment state (work load, duration and intensity), interest in vocational rehabilitation, engagement and activity in daily living, occupations, community and social activities. The survey was carried out individually with each subject during direct interviews.
Comprehensive ICF Core Set for SCI: In clinical practice together with ICF qualifiers can be used to identify the level of activities limitations and participation restrictions of people with SCI in different periods of life. In order to identify functioning of participants during the inpatient rehabilitation the Brief ICF Core Set for Spinal Cord Injury in post-acute context were used. For evaluation of functioning problems of participants in the long-term context, the Comprehensive ICF Core Set for Spinal Cord Injury in long-term context was used. We have divided our participants according to whether they were having or not having the functional problems (Table 2).
| Body functions | |
| The Functional problems (having/not having) | Assessment classification |
| Unidentified dysfunction–body dysfunction is absent or very slight | 0–no dysfunction (0–4%) 1-slight dysfunction (5–24%) |
| Identified dysfunction–severe (moderate, high and complete) body dysfunction | 2–moderate dysfunction (25–49%) 3–high dysfunction (50–95%) 4–complete dysfunction (96–100%) |
| Activity and Participation | |
| Unidentified limitation of activity–the difficulty of participating in activities is absent or very slight | 0–no difficulty (0–4% ) 1–slight difficulty (5–24% ) |
| Identified limitation of activity–severe (moderate, high and complete) difficulty of participating in activities | 2–moderate difficulty (25–49%) 3–high difficulty (50–95%) 4–complete difficulty (96–100%) |
Table 2: Participants distribution according to functional problems.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 computer software statistical package. Descriptive statistics was used for the calculation of the numerical characteristics of a variety of demographic, medical and sociodemographic indicators. The chi-square (χ2) criterion was used for the comparison of qualitative variable frequency, expressed as a percentage. For the ICF categories assigned to the components Activities and Participation absolute frequencies and relative frequencies (prevalence) of impairment/limitation in the research sample were reported along with their 95% CI. To clarify, missing values, as well as the response options ‘not applicable’ ‘not definable’ and ‘comorbidity’ were not taken into account. We inspected the distribution of all study variables to ensure that they met the assumptions of the statistical tests performed. All scales met conditions for normality and hence parametric tests were used. Mean of variables, standard deviation (SD) were calculated. The Student t test for independent samples was applied to compare the means of independent variables. For the comparison of independent samples when variables were measured on an ordinal scale, the Kruskal & Wallis H-test criteria were used. The one-way analysis (ANOVA) was used to determine whether there were any significant differences between the means of three or more independent groups and the difference between these groups was established by the Bonferroni test. All tests were two-tailed and statistical significance was set at p<0.05, significant difference between subgroups (p<0.05, Kruskal &Wallis H-test or CI).
Results
Socio-demographic and SCI-related characteristics
194 people with SCI participated in this research: 153 (78.9%) male, 41 (21.1%) female. Mean age of participants when they experienced SCI was 39.57 ± 11.8 years (SD ± 11.58 years, min-max=18–63 years, CI 95% from 29.57 to 46.45 years). Men and women were the same age and the average age difference – not significant (p=0.625). The majority of the participants belonged to the 18–34 years age group.
The traumatic SCI were more frequent than non-traumatic SCI (respectively 76.3% (n=148) and 23.7% (n=46) of participants) and was similar in both men and women (p>0.05). The most common causes of traumatic SCI were traffic accidents (42.8%), sports or diving into water injuries (24.2%) and household injuries and falls from height (18.6%). Non-traumatic SCI causes were related with medical, surgical interventions or complications and other specific causes (suicide attempt, abscesses and infections).
According to the SCI localization 105 (54.1%) participants had paraplegia, 89 (45.8%) participants had tetraplegia. The heaviest AIS A (59.3%) SCI types were prevailed.
The analyses of social state shows, that after SCI the most of participants were unmarried (40.2%). 33.5% of participants had a special education, 23.7% – higher education and 19.6% – college education (Table 3).
| Characteristics | Category | Proportion, n=194 (%) |
| Sex | Female Male |
41 (21.1%) 153 (78.9%) |
| SCI level | Tetraplegia Paraplegia |
89 (45.9%) 105 (54.1%) |
| SCI type | AIS A AIS B AIS C |
115 (59.3) 55 (28.4) 24 (12.3) |
| SCI ethology | Traumatic Non-traumatic |
148 (76.3) 46 (23.7) |
| Cause of SCI | Traffic accident Fall Sports/diving in shallow water Medical/surgical complications Victims of violence Other |
83 (42.8%) 36 (18.6%) 47 (24.2%) 13 (6.7%) 2 (1.5%) 13 (6.7%) |
| Marital status | Single Currently married Divorced Separated Living out of wedlock |
78 (40.2%) 64 (32.9%) 26 (13.4%) 12 (6.2%) 14 (7.2%) |
| Educational state | Higher (University) education College education Special education Secondary education Primary education Student currently |
46 (23.7%) 38 (19.6%) 65 (33.5%) 12 (6.2 %) 5 (2.6%) 28 (14.4%) |
| Participation in rehabilitation programs | Medical rehabilitation Participated Non-participated |
153 (78.8%) 41 (21.2%) |
| Vocational rehabilitation Participated Non-participants |
59 (30.4%) 135 (69.6%) |
|
| Employment state | Permanent job Private business Short-term jobs (<4 months/year) Work to order Job at home/home-works Not working |
12 (6.2%) 10 (5.1%) 38 (18.5%) 10 (5.1%) 36 (18.5%) 88 (45.36%) |
| Living residence | Town/city Country/village Flats Private house |
128 (65.9%) 66 (34.1%) 134 (69.1%) 60 (30.9%) |
Table 3: General Characteristics of population (n=194).
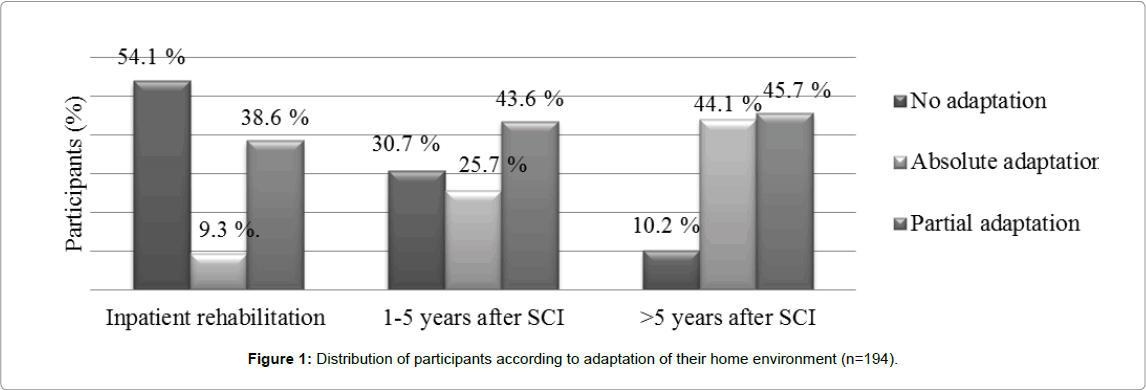
In different periods of life after SCI the most of participants have lived in the city (65.9%) in the flats houses (69.1%). At the end of the primary inpatient rehabilitation only for 9.3% of participants had the absolutely home environment adaptation: main entrance to the house, elevator/stairs, living rooms, kitchen and toilet/bathrooms. During first 5 years after SCI the number of participants having full adaptation of home environment increased from 9.3% to 25.7% (p<0.001) and in long-term period increased to 44.1% of participants (p<0.001) (Figure 1).
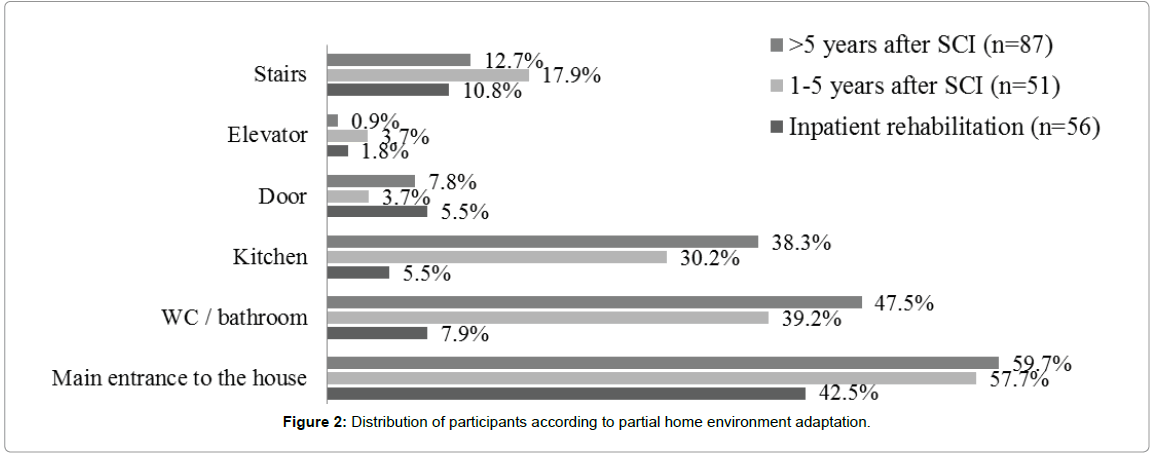
In different periods after SCI the partial home environment adaptation prevailed from 38.6% to 45.7%. Most often were adapted the main entrance to the house (42.5–59.7%), toilet/bathroom (7.9%– 47.5%) and living rooms/kitchen (5.5–38.3%) (Figure 2). These results of research show that in Lithuania attention to environment adaptation to individual needs is paid only after discharge from inpatient rehabilitation programs and it takes more than a few years.
The comparison of home environment adaptation between participants with different level of SCI shows that in different periods of life fully adapted home environment were prevailed between participants with paraplegia (68.9–75.3%), while in home environment of participants with tetraplegia prevailed partial adaptation: the main entrance to the house (42.5–69.7%), toilet/bathroom (89.6–91.1%) and kitchen (22.1–58.7%). It is important to note, that participants with tetraplegia very often had a small environmental adaptation elements: armrests, extended handles, electric hoist, adjustable height furniture, and etc.
The participants’ social life activities were analysed from an employment perspective. At the time of the research 88 (45.3%) of the participants were not working, of whom 56 (63.6%) participated in the rehabilitation program (Group I). During research the permanent employment had 12 (6.2%) participants, of whom 9 (75.0%) had paraplegia and 3 (25.0%) tetraplegia; a private business had 10 (5.1%) participants (8 (80.0%) paraplegics, 2 (20.0%) tetraplegics); short-term but fixed works (1–4 month) were employed 38 (18.5%) participants (28 (73.7%) paraplegics, 10 (26.3%) tetraplegics); and 10 (5.1%) participants (6 (60.0%) paraplegics, 4 (40.0%) tetraplegics) had works to order (events manager, camp instructor, driving course instructor, project member, etc.). All employed participants had workplace and work-environment adaptations, especially participants with tetraplegia (shorter working hours, assistive techniques, adapted working equipment, assistant/helper, and etc.). It is important to note, that during research were prevailed a home-works (crafts, needle work, wood works, translation, computer’s repairing, management, consulting, and etc.) – jobs at home had 28 (14.4%) participants (19 (67.9%) paraplegics, 9 (32.1%) tetraplegics). All employed participants belonged to the long-term context groups; the average age was 38 ± 7.8 years, time period since SCI onset was 11.35 ± 6.26 years. 65 (75.5%) employed participants lived in a town and had a partly adapted house (main entrance to the house, adapted elevator, bathing/toilet room). 42 (64.6%) of employed were driving a special hand-controlled car and were independently arriving to the job, of whom 32 (76.2%) participants had paraplegia.
The analyses of employment changes in long-term period, shows that during first years after SCI onset were employed 10 (17.8%) participants (Group I), of whom 6 (60.0%, 4(66.7%) paraplegics, 2(33.3%) tetraplegics) participants returned to their permanent workplace, where had worked before SCI (banker, accountant, lawyer, doctor, translator, officer); 3 (25.0%) participants with paraplegia had private business; 1 (8.3%) participant had a short-term works. In 1–5 years after SCI period (Group II) significantly increased employed participants to 30.2% – were prevailed a home-works (19.6%), also significantly increased works to order (10.6%) and short-term but fixed 1–4 month works (7.9%). In 5–10 years after SCI period (Group III) amount of employed participants increased to 35.8% and were still prevailed different home-works (25.2%), also increased works to order (11.1%). More than 10 years after SCI (Group IV) prevailed homeworks (37.2%) and short-term jobs (20.3%).
The analyses of work intensity and duration shows, that in different period after SCI prevailed slight intensity jobs, although in a period 1–5, 5–10 and more than 10 years after SCI decreased light/very light intensity jobs from 88.9% to 62.7% of participants and increased middle intensity jobs from 11.1% to 28.8% (Table 4). Also was found that number of full-time works (6–7 hours working day) significantly decreased in long-term period from 50.0% to 27.1% and prevailed of half working day (3–4 hours working day) works (33.3–30.5). It is important to note, that participants with paraplegia often worked light or middle intensity full-time works, while participants with tetraplegia more often had light intensity and half working day jobs.
| Nature of work | <5 years after SCI, n=107 |
5–10 years after SCI, n=40 |
>10 years after SCI, n=47 |
| Work intensity | |||
| Light and very light intensity | 66.7% | 82.1% | 62.7% |
| Middle intensity | 33.3% | 17.9% | 28.8% |
| Severe/very severe intensity | – | – | 8.5% |
| Work duration (hour/day) | |||
| Full working day (6–7 h/d) | 50.0% | 35.7% | 27.1% |
| Half working day (3–4 h/d) | 33.3% | 25.0% | 30.5% |
| Few working hours per day | 27.7% | 28.5% | 25.4% |
| According to the need | – | 10.7% | 16.9% |
| p value | 0,001 | ||
| <0,001 | |||
Table 4: Distribution of participants according to work intensity and duration (hour/day).
Activities and participation in daily life
In order to determine the participants’ activities and participation in different life situations the Comprehensive International Classification of Functioning (ICF) Core set for SCI was applied and assessed: basic and complex action, learning and communication, mobility, self-care, household activities, the general living area and community. In the Table 5 shown, that the common participation restriction in learning and communication activities were found in group I – 49.8% of participants have limitations in solving the problems and overcoming stress and other psychological problems, than in subsequent periods more less of participants experienced these activities limitations. Analyses of participants’ mobility skills showed, that I group main limitations were in changing and maintaining basic body position (62.5%), transferring oneself (64.6%) and moving around (68.8–88.5%), but in groups II– IV these activities limitations were decreased and participants were more independent. Limitations in self-care activities were significantly more frequently reported in group I and group II than in groups III–IV (Table 5).
| ICF category | Described as a functional problem (n=194) | |||||
| group I (n=56) |
group II (n=51) | group III (n=40) | group IV (n=47) | |||
| Learning and communication d155 Acquiring skills d175b Solving problems d240 Overcoming stress and other psychological problems d345a Writing messages Mobility d410a Changing basic body position d415a Maintaining a body position d420a Transferring oneself d430a Lifting and carrying objects d440a Fine hand use d455 Moving around d460b Moving around in different locations d475b Driving Self- Care d510b Washing oneself d520b Caring for body parts d530b Toileting d540b Dressing d550 Eating d560 Drinking d570 Looking after one’s health d630b Preparing meals d640b Doing housework d650 Caring for household objects d660 Assisting others Interpersonal interactions and relationships d770 Intimate relationships Basic life skills d840b Preparing for a job d850b Remunerative employment d870 Economic self-sufficiency d d920b Recreation and leisure |
n (%) | |||||
| 8 (14.3) 28 (49.8) 24 (42.8) 20 (38.6) 31 (62.5) 28 (50.4) 33 (64.6) 29 (51.7) 24 (42.8) 36 (68.8) 46 (88.5) 51 (90.4) 36 (64.5) 29 (56.4) 31 (61.5) 35 (67.5) 24 (42.8) 21 (40.6) 18 (35.4) 45 (88.2) 48 (93.5) 50 (97.9) 25 (55.4) 15 (30.5) 41 (82.7) 48 (90.9) 49 (96.5) 37 (69.8) |
6 (13.3) 15 (29.4) 10 (19.6) 13 (24.6) 26 (48.1) 29 (49.9) 36 (51.3) 34 (65.3) 39 (71.1) 35 (66.7) 39 (71.1) 34 (65.3) 34 (65.5) 28 (45.6) 24 (45.1) 25 (49.1) 20 (39.1) 10 (19.6) 8 (15.7) 28 (54.9) 30 (58.8) 28 (54.9) 16 (31.3) 18 (35.3) 31 (60.5) 30 (58.8) 29 (57.9) 24 (47) |
4 (10.1) 11 (27.4) 11 (27.5) 6 (15.1) 13 (32.5) 11 (30.4) 15 (36.9) 16 (38) 16 (38) 14 (33.6) 17 (37.3) 10 (28.8) 18 (45) 18 (45) 17 (41.5) 15 (37.5) 5 (12.5) 4 (10) 14 (35.6) 16 (40) 17 (42.5) 17 (42.5) 11 (27.5) 12 (30) 22 (50.1) 15 (37.7) 18 (45.5) 13 (32.5) |
5 (11.7) 9 (19.1) 10 (21.2) 5 (11.3) 9 (19.1) 12 (24.4) 18 (28.2) 16 (24.5) 16 (24.5) 13 (20.2) 15 (23.1) 8 (17.6) 16 (34.1) 16 (34.1) 14 (29.7) 15 (31.9) 5 (10.6) 5 (10.6) 9 (19.1) 14 (29.7) 16 (34.1) 26 (34.1) 9 (19.1) 9 (19.1) 12 (26.7) 12 (26.7) 15 (32.4) 10 (21.2) |
|||
a Significant difference between groups (p< 0.05. Kruskal &Wallis H-test or confidence interval).
b Significant different problem frequency in 1 group versus groups in long-term context (no overlap of CIs).
Table 5: Activities and participation – detected performance problems of participants (95% CI).
Activity in daily life
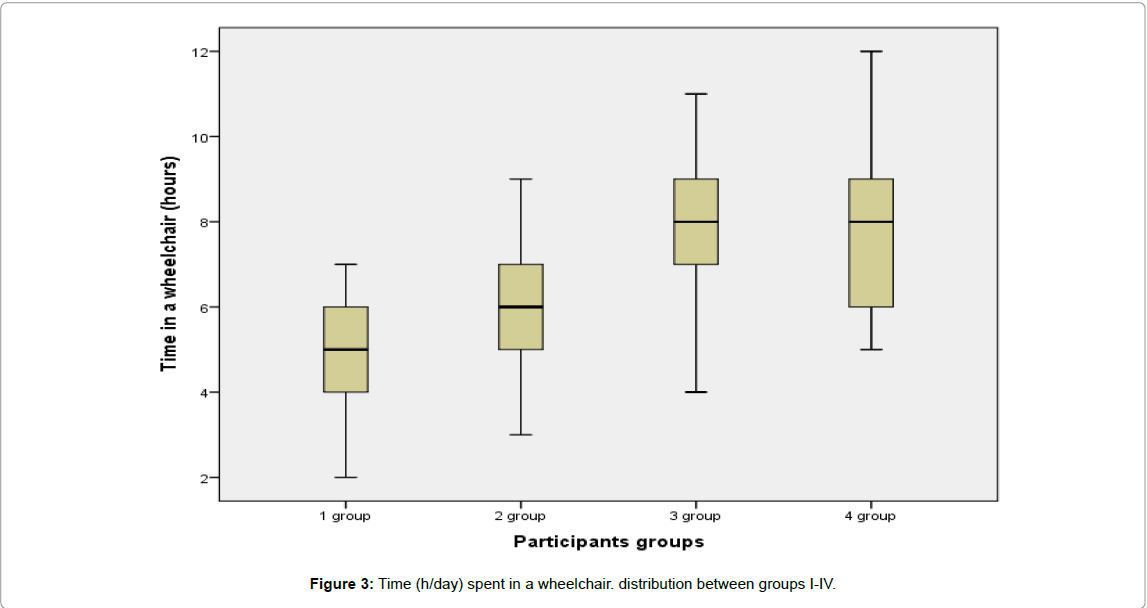
In order to analyse the activity in everyday life in different periods after SCI onset and to assess the subjective opinion of participants about the extent of the different areas or activities in which there are more problems a brief form of the Life Situation Questionnaire-revised (LSQ-r) were used. During primary inpatient rehabilitation the time, spent by participants in wheelchair was significantly lower than in longterm periods (respectively 4.62 ± 0.86 and 7.18 ± 1.80 h/d, p<0.001). Since the abdominal muscles are available to support the body, it was considered that patients during the inpatient rehabilitation could maintain the sitting position in a wheelchair. A prolongation of time spent in a wheelchair was observed: in the beginning of rehabilitation 3.51±2.09 h/d, at the end of rehabilitation 4.68 ± 1.13 h/d (p<0.001). A tendency to prolongation of wheelchair-time was observed also in the long-term context groups (Figure 3): time in a wheelchair of group II was 5.86 ± 1.72 h/d, not significantly different from group I (p=0.03), but significantly different (p=0.001) from groups III and IV. The time in a wheelchair was not significantly different (p>0.001) between group III (7.85 ± 1.57 h/d) and group IV (7.53 ± 1.39 h/d).
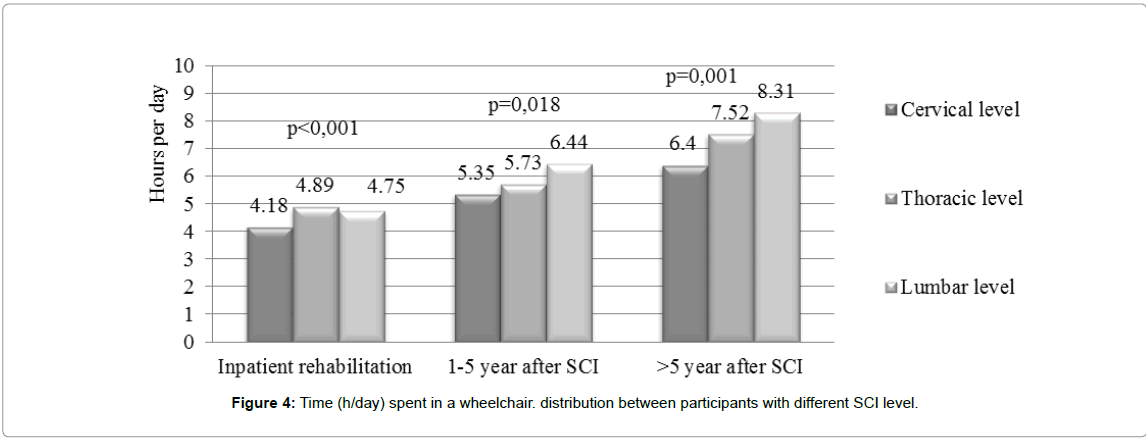
Participants with SCI in cervical level spend significantly less time in wheelchair than participants with SCI in thoracic or lumbar level (p<0.05) (Figure 4).
The analysis of participant’s physical activity (intensive training, exercising, participation in sports, active leisure) shoved, that training/ exercising were more observed in group I (everyday including weekends, approximately 3–4 h/d) than in the other groups (p<0.001) (Table 6) – at the end of inpatient rehabilitation participants more often exercised – 87.5% of participants exercised 5 times a week, approximately 2.5 hours per day (89.9% tetraplegics, 85.8% paraplegics). In group II the intensity of exercising significantly not decreased compared with group I (p>0.05) – 78.4% of participants still exercised 5 times a week, though we found that more participants with tetraplegia (73.5%) exercised, than participants with paraplegia (57.1%). In subsequent periods (groups III-IV) was found that every year after SCI observed a decreasing training/exercising intensity to twice a week, from 30 minutes to 1.5 hours per day. Also we found that participants with tetraplegia exercised often (1–2 times per week, 30–45 min per day) compared to participants with paraplegia, which rate of exercising decreased to few times per month (p<0.001). However, participants of group IIIIV more frequently participated in sports and active leisure activities compared with participants of groups I-II (p<0.001) – participation in sports increased from 8.9% to 34.1% (p<0.05). It is important to note, that participants with paraplegia more actively participated in sports (84.8%) than participants with tetraplegia (15.2%).
| Frequency of exercising | Inpatient rehabilitation (the end). n (%) | 1-5 years after SCI. n (%) |
5-10 years after SCI. n (%) | >10 years after SCI. n (%) |
| Rarely | - | - | - | 8 (17.1) |
| 1 times per mounth | - | - | 2 (1.8) | 11 (23.4) |
| 2–3 times per mounth | - | 1 (1.9) | 10 (25.0) | 10 (21.3) |
| 1–2 times per week | - | 2 (3.9) | 17 (42.5) | 18 (38.3) |
| 3–4 times per week | 2 (3.5) | 4 (7.8) | 8 (20.0) | - |
| ≥ 5 times per week | 49 (87.5) | 40 (78.4) | 3 (7.5) | - |
| Everyday | 5 (8.9) | 4 (7.8) | - | - |
| Participation in sports | ||||
| 5 (8.9) | 8 (15.7) | 11 (27.5) | 16 (34.1) | |
| p value | 0.059 | |||
| <0.001 | ||||
Table 6: Distribution of participants according to exercising frequency (95% CI).
The analysis of participant’s physical activity related with household chores, visits by relatives, friends or neighbours and social/ community life activities shoved, that the lowest average of hours a week participants devoted to was assessed in group I – during primary inpatient rehabilitation compared with significantly prolonged time in group II, III and IV – time spent on household chores increased from 1.98 ± 1.10 h/d to 4.41 ± 2.24 h/d (p<0.001). Statistically significant positive correlation between the change of time spent on household chores and the time until long-term periods (r=0.282, p=0.003) showed, that the more time has passed after SCI, the bigger increase in time spent on household chores was. The major part of group I participants at the end of inpatient rehabilitation indicated that they were visited by relatives, friends or neighbours 3–5 times a week (79.9%), they went outside on average 1–2 times a week and very rarely went out to manage social matters or to entertain (80.3%). Many of group II participants indicated that while being at home they went outside more often than during inpatient rehabilitation, but the most of participants went out at least a few times a month (73.5%). It should be noted that in group III and IV significantly more participants at least once a week and more often went out to manage social matters or to entertain (p<0.001), they were going outside on average of 2–5 times a week, but the number of participants going outside only a few times a month also increased (p=0.003) but they were significantly less frequently visited by relatives than during inpatient rehabilitation, on average, only a few times a month (p<0.001) (Table 7). Significant differences between participants with different SCI level according to time spent on household chores, frequency of going out to manage social matters and visits by relatives was not found (p>0.05) – participants had a very similar these activities.
| Going out to manage social matters or outside | Inpatient rehabilitation (the end). n (%) | 1-5 years after SCI. n (%) | 5-10 years after SCI. n (%) | >10 years after SCI. n (%) | |
| Rarely | 45 (80.3) | 1 (1.9) | - | 1 (2.1) | |
| 1 times per mounth | 5 (8.9) | 10 (19.6) | 1 (2.5) | 8 (18.1) | |
| 2–3 times per mounth | 5 (8.9) | 37 (73.5) | 6 (15.0) | 17 (36.1) | |
| 1–2 times per week | 1 (1.7) | 2 (3.9) | 20 (50.0) | 13 (27.5) | |
| 3–4 times per week | - | 1 (1.9) | 9 (22.5) | 7 (15.6) | |
| ≥ 5 times per week | - | - | 4 (10.0) | 1 (2.1) | |
| Everyday | - | - | - | ||
| P value | <0.001 | ||||
| <0.001 | |||||
Table 7: Distribution of participants according to frequency of going out to manage social matters or outside (to the garden. etc.) (95% CI).
Discussion
The analyses of socio-demographic characteristics of our participants showed, that SCI occur mostly young 34 years of age and unmarried men. In the literature, presented a similar findings that up to 55% of all people after SCI onset were unmarried (single) men [3,5]. The results show that people with SCI studied and actively participated in labour market and sought to gain better education level. At the time when SCI occurred, the most of participants had a college, special (advanced vocational) and higher education, however in long-term period increased the number of participants with thirty educations from 43.3% to 51.5%. A similar data indicate M.W.G. Brinkhof with other researchers, stating that SCI often experienced at a young age, and actively achieve restore their social status and integration [3]. During first 5 years after SCI onset our participants actively participated in labour market and in long-term period over 2 times more participants were employed (form 17.8% to 30.2%). In lo period 5–10 and >10 years after SCI prevailed jobs at home (home-works), increased the amount of short-term works under fixed-term contracts and works to order. We found that in labor market more participated participants with paraplegia, also prevailed full day mild intensity works, though the number of jobs of average intensity increased in long-term period (p<0.001). In scientific literature of different countries dominated the lack of consistent data about the changes of employment state of people with SCI. Ottomanelli et al. [23,24] state, that employment rate of people with SCI can range from 12% to 35% and increase to 64%, other authors found that during 20 years period after SCI employment rates increasing to 41% [17,25] or reached to 58% [18]. Also these authors state that more than 85% of employed were paraplegics. Regardless of the inconsistency of different countries research data, we can accept the fact that people with SCI were actively trying to participate in the labour market. While taking into account the overall Lithuanian people with disabilities situation in the labour market [15,26,27], other authors Lithuania conducted studies [2,15] and based on our research results, we suggest that possibility of employment of this population is limited, while the prevailing socio-economic situation in the country, the relatively low vacancies of job for disabled people, due is dominated short-term, fixed-term and home-based works. Similar findings to our research stated other authors.
Our data showed, that in different periods of life after SCI onset the most of people with SCI have lived in the city in the apartments and their home environment was least adapted at the end of the primary inpatient rehabilitation (9.3% absolutely adaptation). During first 5 years after SCI onset full adaptation of home environment increased from 9.3% to 25.7% of participants (p<0.001) and in subsequence periods increased to 44.1% (p<0.001). In different periods of life more adapted home environment had participants with paraplegia, while in home environment of participants with tetraplegia prevailed partial adaptation and small environmental adaptation elements. These results of research show that in Lithuania attention to environment adaptation to individual needs is paid only after discharge from inpatient rehabilitation programs and it takes more than a few years. These our research data contradicts to the results of developed countries, Krause et al. [22] and Leeuwen et al. [10] claim that during primary rehabilitation program must be carried out the complete home environment adaptation, to which the person has to return after discharge from medical rehabilitation, in order to ensure the independence, physical activity and well-being.
The prevalence of many functional problems and physical activity limitations associated with SCI may verify over the time since SCI onset. The interdisciplinary approach of the rehabilitation team (including the patient and family) and formulating of functional outcomes are very important in early period after SCI onset for ensuring be required for functional mobility and independence in daily living, recovery social activity and to convey that life after SCI can be fulfilling in long-term context [2,16]. Anton et al. [28] noted importance of rehabilitation program at early stage after SCI onset to reach improvement in the physical and functional state, mobility, physical activity in daily living, equipment needs, and adjustment issues after injury. We also detected, that SCI rehabilitation contributes to good physical state and increasing activities in daily living: participation in rehabilitation had a positive impact to decreasing difficulties in solving the problems, overcoming stress and other psychological problems, mobility and self-care skills (p=0.001) and in long-term period these difficulties significantly decreased. Authors [12,14,15,29] observed the changes of psychoemotional status during inpatient rehabilitation and after discharge in 5,10, 20 years these changes related with improving functional skills and adaptation to the another life. Although Crane et al. [30] notice that in long-term period the mobility and abilities to move around in wheelchair improves naturally engaging and participating in daily life activities. Based on our results of Ullrich et al. [31] conducted studies, we could suggest that during inpatient rehabilitation have purposefully been trained functional skills and after discharge at home environment naturally increases the need to move around in various locations, when naturally are improving the physical activity and capacity.
We found, that after SCI onset more than 90% of participants’ complete limitations in self-care, household activities and participation in leisure activities (sports, arts, culture and etc.). During primary rehabilitation we detected the biggest improvement of these skills (p<0.001) and at least limitations were in long-term period (p<0.05). However, the biggest improvement in household and leisure activities of our participants was determined after discharge from rehabilitation (p<0.001), also the biggest participation in sport and leisure activities of our participants was detected just in 5–10 and >10 years after SCI period – the difficulties in these activities decreased almost 4 times (p<0.001). In the literature, are low of research that analyzed the participation and activities in household of participants after SCI during medical rehabilitation programs. In most cases the authors [8,17,25,32] analyses the engagement in household activities in long-term period and notes, that participation level in domestic activities depends on the prevailing natural opportunities to engage in these activities and ability to use these skills. Van den Berg-Emons et al. [33] states, that it is necessary during primary rehabilitation started the improvement of household skills, to ensure independence and skills at home. The authors [28,30] state that the greatest improvement of self-care skills during primary rehabilitation associated to the purposeful trainings of functional skills and abilities. But references of Pelletier [34] presented data does not correspond to our study results, which suggest that at the end medical rehabilitation period decreased the participation in recreation and leisure activities and in subsequent periods remained at the same level. However, authors [20,35] participation and engagement in sports and recreational activities increased with every year after SCI onset, and too low participation in these activities related to the limited opportunities of people with disabilities in sports and employment, especially in smaller towns. Therefore, the authors claim that the even during inpatient rehabilitation, it is important to start encourage people after SCI participation in sport and active leisure, by engaging in nongovernmental, and employment of the disabled sports organizations.
The analyses of activity in everyday life in the different periods after SCI showed, that the time, spent in wheelchair, change from the primary rehabilitation up to 5 years after SCI onset was significantly lower than after 5–10 years and more years after SCI onset (p>0.05). We can state, that every year after SCI the people with SCI more time spent in a wheelchair. Participants with SCI in cervical level spend significantly less time in wheelchair than participants with SCI in thoracic or lumbar level (p<0.05). Our results do not coincide with Krause et al. [21,22,36] longitudinal studies to carry out in United States. The authors found that individuals after SCI onset the most time spent in a wheelchair at the primary rehabilitation, and after discharge from rehabilitation at home the time is falling dramatically, although in later periods some people in a wheelchair spent up to 8.5 h per day.
Analysing our participants physical activity in daily life related to exercising, we found that the highest exercise intensity was observed in the first 5 years after SCI period and not differ between participants with different SCI level: participants more often exercising than in subsequence periods (p<0.001). However, in long-term period significantly decreased intensity of exercising, especially between participants with paraplegia, however significantly increased their participation in sports (p<0.05). Such our study agrees with the results of Haas et al. [14] and Martin et al. [37] that, at the end of medical rehabilitation the training of people with SCI significantly decreased and during the subsequent periods about 70% people remained physically inactive. The author’s claim that would be appropriate during inpatient rehabilitation begins to form a physically active lifestyle. Our study confirms that during the primary rehabilitation program, housework skills training is given too little attention and people with SCI after discharge at home have a lot of problems. The authors [25,38] agrees with our study results, and state, that the activity in housework’s is improving with each year after SCI onset by naturally engaging in different life situations, and authors recommends that during inpatient rehabilitation currently pay more trainings and purposeful activities for housekeeping skills. Krause et al. [22] in the longitudinal studies confirm our findings, that people after SCI onset mostly in long-term period go to the field and going to handle social affairs. In the literature, there is a lack unified data on very individual changes and the authors [39,40] state that it is very difficult to identify social activity patterns, resulting in the family, community, and country-existing conditions.
Conclusions
The assessment of biopsychosocial variables could provide more detailed information about changes of physical state, functioning in daily living activities and social life of this population and could help identify the main factors influenced functioning in different period after SCI. we can state, that inpatient rehabilitation are effective and have a positive impact on patients after SCI onset: the severe biopsychosocial dysfunction were reduced and activity in everyday life were improved; in long-term period naturally engaging in different daily life areas are improving physical and functional state, functional skills and abilities, maintaining physical activity and capacity. The changes of employment needs, forms and possibilities of people with SCI in long-term period naturally involved in the life of the self-realization and integration observed the increase of participation in daily and social activities, and for performance of these activities is necessary improvement of functions, physical capacity and activity, skills and abilities.
Competing Interests
The authors have no competing interest concerning this study.
Acknowledgments
The research was funded by the Department of Rehabilitation, Physical and Sports medicine, the Medical faculty, Vilnius University and the Rehabilitation, Physical and Sports medicine center, Vilnius University hospital Santaros klinikos.
The research data in long-term context is based on work supported by Paraplegic Association of Lithuania, in ‘Landscape Therapy and Recreation Centre’ Palanga, Lithuania.
References
- Juocevicius A, Butenaite L (2010) SCI peculiarities in Lithuanian patients in 1994–2008. Gerontology 11: 95-102.
- Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A, et al. (2016) Swiss national community survey on functioning after spinal cord injury: Protocol, characteristics of participants and determinants of non-response. J Rehabil Med 48: 120-30.
- Wong AWK, Ng S, Dashner J, Baum MC, Hammel J, et al. (2017) Relationships between environmental factors and participation in adults with traumatic brain injury, stroke, and spinal cord injury: a cross-sectional multi-center study. Qual Life Res.
- Rahimi-Movaghar V, Sayyah MK, Akbari H, Khorramirouz R, Rasouli MR, et al. (2013) Epidemiology of traumatic spinal cord injury in developing countries: A systematic review. Neuroepidemiology 41: 65-85.
- Krause JS, Terza JV, Dismuke CE (2010) Factors Asociated with Labor Force participation after SCI. J Vocational Rehab 33: 89-99.
- National Spinal Cord Injury Statistical Center, Facts and Figures at a Glance (2016) Birmingham, AL: University of Alabama at Birmingham.
- van Leeuwen CM, Post MW, Westers P, van der Woude LH, de Groot S, et al. (2012) Relationships between activities, participation, personal factors, mental health, and life satisfaction in persons with spinal cord injury. Arch Phys Med Rehabil 93: 82-89.
- van Leeuwen CM, Post MW, van Asbeck FW, Bongers-Janssen HM, van der Woude LH, et al. (2012) Life satisfaction in people with spinal cord injury during the first five years after discharge from inpatient rehabilitation. Disabil Rehabil 34: 76-83.
- World Health Organization (WHO) – Media Centre: Spinal Cord Injury.
- Migliorini CE, New PW, Tonge BJ (2009) Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic post-acute spinal cord injury. Spinal Cord 47: 783-788.
- Widerstrom-Noga E, Anderson KD, Perez S, Hunter JP, Martinez-Arizala A, et al. (2017) Living With Chronic Pain After Spinal Cord Injury: A Mixed-Methods Study. Arch Phys Med Rehabil 98: 856-865.
- Haas B, Playford ED, Ahmad AQ, Yildiran T, Gibbon AJ, et al. (2016) Rehabilitation goals of people with spinal cord injuries can be classified against the International Classification of Functioning, Disability and Health Core Set for spinal cord injuries. Spinal Cord 54: 324-328.
- Butenaite L (2014) The mathematical model of evaluation of functional independence, body functions, activities and participation peculiarities of people with SCI. Vilnius, Lithuania: Vilnius University.
- Stillman MD, Barber J, Burns S, Williams S, Hoffman JM (2017) Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil 98: 1800–1805.
- Lim PA, Tow AM (2007) Recovery and regeneration after spinal cord injury: A review and summary of recent literature. Ann Acad Med Singapore 36: 49-57.
- Krause JS, Bozard JL (2012) Natural course of life changes after spinal cord injury: A 35-year longitudinal study. Spinal Cord 50: 227-231.
- Silver J, Ljungberg I, Libin A, Groah S (2012) Barriers for individuals with spinal cord injury returning to the community: A preliminary classification. Disabil Health J 5: 190-196.
- Barclay L, McDonald R, Lentin P (2015) Social and community participation following spinal cord injury: A critical review. Int J Rehabil Res 38: 1-19.
- Krause JS, Saunders LL (2011) Health, secondary conditions, and life expectancy after spinal cord injury. Arch Phys Med Rehabil 92: 1770-1775.
- Krause JS, Newman JC, Clark JMR, Dunn M (2017) The natural course of spinal cord injury: Changes over 40 years among those with exceptional survival. Spinal cord 55: 502-508.
- Ottomanelli L, Barnett SD, Goetz LL (2014) Effectiveness of supported employment for veterans with spinal cord injury: 2-year results. Arch Phys Med Rehabil 95: 784-790.
- Ottomanelli L, Lind L (2009) Review of critical factors related to employment after spinal cord injury: implications for research and vocational services. J Spinal Cord Med 32: 503-531.
- Lidal IB, Hjeltnes N, Røislien J, Stanghelle JK, Biering-Sørensen F (2009) Employment of persons with spinal cord lesions injured more than 20 years ago. Disabil Rehabil 31: 2174-2184.
- Skucas K, Mockeviciene D (2009) Factors influencing the quality of life of people with SCI. Spec Education 29: 35-42.
- Okuneviciute NL, Kavaliauskaite R, Žemaitaityte G (2012) Situation of the disabled on the labour market. Environmental Adaptation for Needs of Disabled. Vilnius, Lithuania.
- Anton HA, Miller WC, Townson AF, Imam B, Silverberg N, et al. (2017) The course of fatigue after acute spinal cord injury. Spinal cord 55: 94-97.
- Ginis KA, Hicks AL, Latimer AE, Warburton DE, Bourne C, et al. (2011) The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord 49: 1088-1096.
- Crane DA, Little JW, Burns SP (2011) Weight gain following spinal cord injury: A pilot study. J Spinal Cord Med 34: 227-232.
- Ullrich PM, Spungen AM, Atkinson D, Bombardier CH, Chen Y, et al. (2012) Activity and participation after spinal cord injury: State-of-the-art report. J Rehabil Res Dev 49: 155-174.
- Scheuringer M, Kirchberger I, Boldt C, Eriks-Hoogland I, Rauch A, et al. (2010) Identification of problems in individuals with spinal cord injury from the health professional perspective using the ICF: a worldwide expert survey. Spinal Cord 48: 529-536.
- van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, et al. (2008) A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil 89: 2094-2101.
- Pelletier CA (2014) Incorporating physical activity into the rehabilitation process after spinal cord injury. Appl Physiol Nutr Metab 39: 513.
- Lundström U, Lilja M, Petersson I, Lexell J, Isaksson G (2014) Leisure repertoire among persons with a spinal cord injury: Interests, performance, and well-being. J Spinal Cord Med 37: 186-192.
- Krause JS, Coker JL (2006) Aging after spinal cord injury: A 30-year longitudinal study. J Spinal Cord Med 29: 371-376.
- Martin Ginis KA, Jetha A, Mack DE, Hetz S (2010) Physical activity and subjective well-being among people with spinal cord injury: A meta-analysis. Spinal Cord 48: 65-72.
- de Groot S, van der Woude LH, Niezen A, Smit CA, Post MW (2010) Evaluation of the physical activity scale for individuals with physical disabilities in people with spinal cord injury. Spinal Cord 48: 542-547.
- Müller R, Peter C, Cieza A, Geyh S (2012) The role of social support and social skills in people with spinal cord injury-A systematic review of the literature. Spinal Cord 50: 94-106.
- Clark JMR, Krause JS (2017) Vocational Interests by gender and race 10 years after spinal cord injury. Rehabil Psychol.
Citation: Šidlauskienė A, Adomavičienė A, Burokienė S, Raistenskis J (2017) Functioning and Physical Activity after Spinal Cord Injury. Occup Med Health Aff 5:265. DOI: 10.4172/2329-6879.1000265
Copyright: © 2017 Šidlauskienė A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6326
- [From(publication date): 0-2017 - Aug 23, 2025]
- Breakdown by view type
- HTML page views: 5392
- PDF downloads: 934