Helicobacter pylori Infection and Gallbladder Diseases: A Mini-Review
Received: 08-Oct-2021 / Accepted Date: 22-Oct-2021 / Published Date: 29-Oct-2021
Abstract
Helicobacter pylori (H. pylori) are recognized as one of the most common chronic bacterial infections worldwide. It’s proved to be the main pathogenic agent in chronic gastritis, peptic ulcer, and gastric cancer, as well as the proposed etiology in diseases of the organs other than the stomach and duodenum like liver, biliary system, heart and vascular system, and skin. Different studies have suggested bacterial infection with H. pylori can also be involved in the pathogenesis of gallbladder diseases. If such association is proven, the incidence of gallbladder diseases and their consequent morbidity and mortality can be reduced significantly following the treatment of H. pylori infection. Therefore, in this mini-review, we aimed to discuss shortly about the association of H. pylori infection in gallbladder diseases, such as chronic cholecystitis, cholelithiasis and gall bladder cancer. Our study shows that H. pylori infection in the gallbladder may be one of the etiological factors leading to the gallbladder diseases. The precise mechanism requires further verifications.
Keywords: Helicobacter pylori; Gallbladder; Chronic cholecystitis; Cholelithiasis; Gallbladder cancer
Abbreviations
ALT: Alanine Aminotransferase; ALP: Alkaline Phosphatase; AST: Aspartate Aminotransferase; CHD: Coronary Heart Disease; MALT: Mucosa-Associated Lymphoid Tissue; GERD: Gastro Esophageal Reflux Disease; GTP: Glutamyltransferase; H. Canis: Helicobacter canis; H. Pylori: Helicobacter pylori; HCV: Hepatitis C Virus; PCR: Polymerase Chain Reaction.
Introduction
Helicobacter pylori (H. pylori) is a spiral shaped, gram-negative, microaerophilic rod with 4-7 flagella [1]. It is recognized as one of the most common chronic bacterial infections worldwide, infecting approximately half of the global population [2]. The discovery of H. pylori by histological examination of gastric biopsies and its isolation by Warren and Marshall in 1983 have opened new horizons in the management of various gastro-duodenal disorders [3]. Since its discovery, it’s proved to be the main pathogenic agent in various gastric pathologies such as chronic gastritis, gastric ulcer, duodenal ulcer, chronic atrophic gastritis, gastric Mucosa-Associated Lymphoid Tissue (MALT) lymphoma, gastric adenocarcinoma, non-ulcer dyspepsia and Gastro Esophageal Reflux Disease(GERD) [1,4].
Literature Review
Helicobacter species and H. pylori have been isolated from sites other than the stomach such as oral cavity, liver and biliary tree of animals and humans. The association between some Helicobacter species infections with certain diseases of the liver in some animals such as Helicobacter canis (H. canis) in dogs, and Helicobacter hepaticus and Helicobacter bilis in mice have been studied [3]. By the way, the relationship of H. pylori with diseases of organs other than the stomach and duodenum (extra gastric or extra duodenal) has also been investigated and reported [4,5]. H. pylori antibody was detected in liver in patients with chronic liver diseases, non-alcoholic fatty liver diseases, non-alcoholic steatohepatitis, liver fibrosis, primary sclerosing cholangitis, primary biliary cirrhosis, intrahepatic stones, hepatic encephalopathy in patients with cirrhosis and hepatic carcinoma [1,6-9], in biliary tract and gallbladder in biliary epithelial inflammation [1] and cholelithiasis [10,11], in heart and vessels in atherosclerosis, acute coronary ischemia (biopsies from aorta and internal mammary artery), Coronary Heart Disease (CHD) and atheroma [1,12,13] and in the skin in acne rosacea, chronic urticarial and Sweet’s Syndrome [1]. To add more, H. pylori are associated with iron deficiency anemia in children, coalmine deficiency, Vitamin B-12 deficiency and megaloblastic anemia [1].
Helicobacter species DNA can be detected in the bile by Polymerase Chain Reaction (PCR) through the DNA sequencing that sequences specific to H. pylori (16S rRNA, cagA), and this can be found at a high frequency in the bile samples, although isolation of the bacterium in the culture medium, cannot be easily reached. To explain this finding, there are different reasons. One reason could be due to the fact that the bacterium could convert from a viable helical form to a non-viable coccid in the bile. Another possibility is the few numbers of bacterium which suppressed by the unfavorable environment in the bile [3].
Different studies have suggested bacterial infection with Helicobacter pylori can also be involved in the pathogenesis of gallbladder diseases. If such association is proven, the incidence of gallbladder diseases and their consequent morbidity and mortality can be reduced significantly following the treatment of H. pylori infection. Therefore, in this mini-review, we aimed to discuss shortly about the association of H. pylori infection in gallbladder diseases, such as chronic cholecystitis, cholelithiasis and gall bladder cancer.
Chronic cholecystitis: Chronic cholecystitis or symptomatic gallbladder is a prolonged mechanical or functional disorder of abnormal gallbladder emptying or biliary dyskinesia [14]. Sabbaghian suggest that biliary dyskinesia should be considered as part of the spectrum of symptomatic gallbladder disease that can be successfully treated with cholecystectomy and that the biliary dyskinesia is associated with GERD and gastritis [15].
Bile reflux and regurgitation are associated with chronic cholecystitis. H. pylori are sensitive to bile salts, because the bile salts have toxic effect on H. pylori. H. pylori were present in the stomachs of the patients with chronic lithic cholecystitis and a bile reflux. It shows that a high incidence rate of H. pylori infection existed in the stomach in the presence of a bile reflux, so H. pylori could live in the basic condition and even aggravate gastritis, this could suggest the existence of a kind of resistant H. pylori to bile salts. Bile reflux and regurgitation may play a role in selecting the kind of H. pylori so that the H. pylori resistant to bile salts could survive and, in combination with the bile, aggravate the injury of gastric mucosa. Resistant H. pylori could survive under basic circumstances and could enter the gallbladder via a reverse route [16].
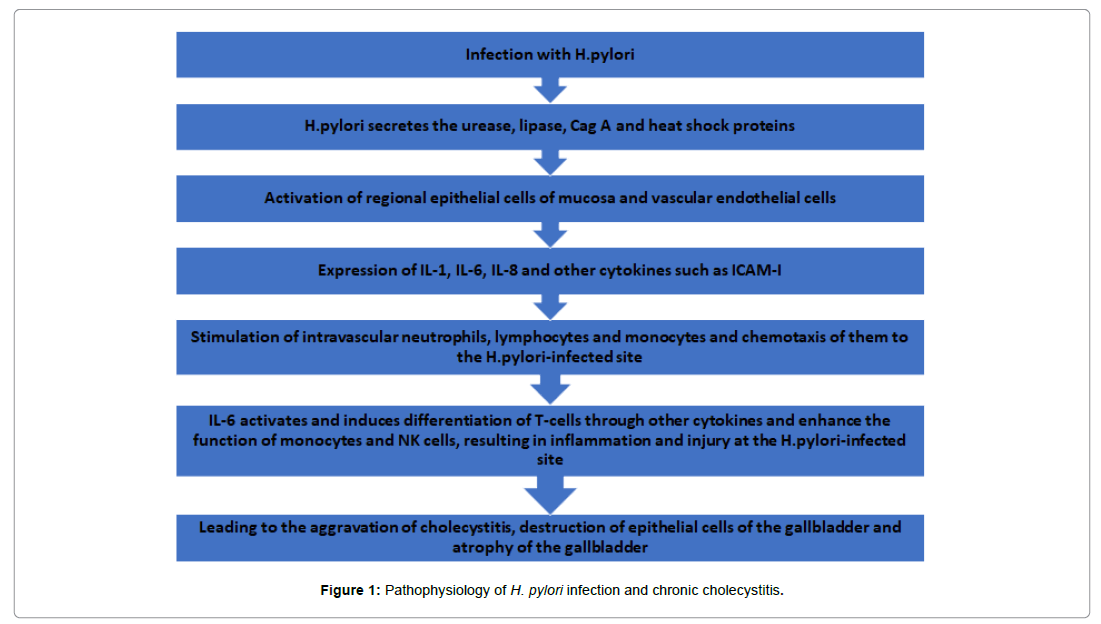
Colonization of the gallbladder with H. pylori would be the cause of chronic inflammation similar to the association of H. pylori in chronic gastric inflammation. Moricz found that there is a high prevalence of Helicobacter species in patients with chronic cholecystitis and cholecystolithiasis and proposed that the bacterial infection may be associated with a pathological mechanism [17]. Chen showed the association of gastric metaplasia of gallbladder mucosa with chronic cholecystitis which this might be related to the H. pylori infection in the gallbladder. H. pylori can harm the gallbladder mucosa epithelial cells through mediating inflammation and immunoreaction [16]. Figure 1 shows the pathophysiology of H. pylori infection and chronic cholecystitis.
Cholelithiasis: Gallstone is a major public health concern worldwide, and is one of the most prevalent digestive disorders needing hospitalization. The etiology and pathogenesis of gallstone formation is unclear. Gallstone formation may be related to a collaboration of genetic and environmental aspects like female sex, family history, and ethnicity. Gallbladder movement disorder (biliary dyskinesia), hyperlipidemia (high cholesterol due to high-cholesterol diet), and medications (e.g., ceftriaxone, and Clofibrate), affect gallstone formation through the increasing in the activity of β-Hydroxyl Methyl Glut aryl-CoA (HMG-CoA) reeducates enzyme or increase in the liver absorption of cholesterol from the blood [18]. Some other conditions and diseases such as obesity, pregnancy, nutrition, Crohn’s disease, terminal ileum resection, stomach surgery, hereditary spherocytosis, sickle cell anemia, thalassemia, Hepatitis C Virus (HCV) infection and gallbladder polyps may affect gallstone formation [18,19]. Several liver enzymes like aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), Alkaline Phosphatase (ALP), and γ-Glut Amyl Transferase (GTP) are associated with gallstone formation [19].
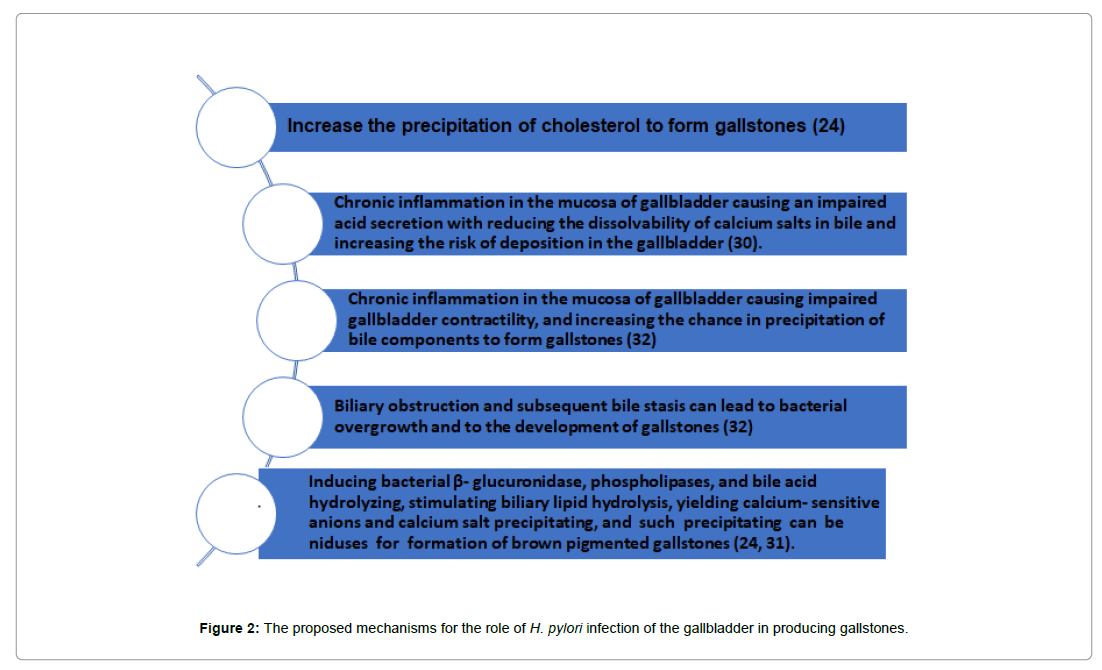
Gastro duodenal environment has an important role in the presence of gallstones and H. pylori are believed to be an arbitrating factor for gastric and extra gastric disease. The gallbladder and bile duct may be two of the targets of chronic H. pylori infection. Kawaguchi first detected H. pylori in the gallbladder’s mucosa of a patient with gallstones and cholecystitis who underwent cholecystectomy in 1996 for the first time [19,20]. There are controversial results from different studies, showing in favor of [21-24] or against [11,25-30] the theory of role of H. pylori in gallstone formation. Several potential mechanisms may account for the association of H. pylori infection and gallstones [31]. Figure 2 shows the proposed mechanisms for the role of H. pylori infection of the gallbladder in producing gallstones [32,33].
Gallbladder cancer: Risk factors for the development of gallbladder cancer are patient demographics, gallbladder abnormality, patient exposure, and Salmonella and Helicobacter infections [30]. The association between H. pylori infection and biliary tract carcinoma (gallbladder cancer, and cholangiocarcinoma) is still controversial [34- 36].
There are high prevalence rates for H. pylori in accordance with high incidence rates for biliary tract carcinoma in Japan, Chile, and in Native American Indians. Though, like gastric carcinoma, some regions of the world, for example, the Africa have very high rates for H. Figure 2: The proposed mechanisms for the role of H. pylori infection of the gallbladder in producing gallstones. pylori infection but low rates for biliary tract carcinoma (the mystery of Africa) [21].
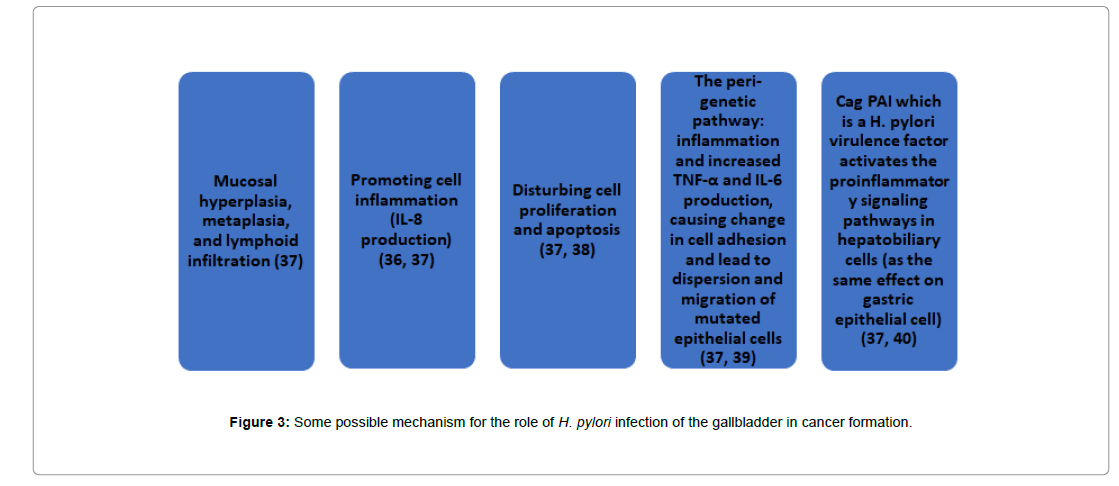
Hassan showed that the H. pylori infection could aggravate gallbladder mucosal lesions which are potentially precancerous (mucosal hyperplasia, metaplasia, and lymphoid infiltration) [37]. There are multiple possible mechanisms explaining the association of H. pylori infection and gallbladder cancer. Figure 3 shows some possible mechanism for the role of H. pylori infection of the gallbladder in cancer formation [38-40].
Conclusion
Two-thirds of the world population is infected with H. pylori. H. pylori infection in the gallbladder may be one of the etiological factors leading to the gallbladder diseases, and gastric or intestinal colonization could be a source for gallbladder infection. The mechanism through which these bacteria contribute to the pathophysiology of gallbladder diseases is unclear at this time.
In order to support the relationship between Helicobacter spp. and gallbladder diseases, some measurements should be considered: To develop the experimental models, some further detailed, controlled and multi-centered studies involving more patients with different Hepatobiliary diseases (preferably including both non-neoplastic and neoplastic diseases) must be performed; The conditions for the growth and cultivation of Helicobacter species from the biliary tree should be improved; Some animal models should be improved to elucidate the pathogenesis and the precise molecular mechanisms by which Helicobacter could affect the genesis of Hepatobiliary diseases and their clinical outcome.
References
- Lacy BE, Rosemore J (2001) Helicobacter pylori: Ulcers and more: The Beginning of an era. J Nutr 131: 2789S-2793S
- Shah SC, Iyer PG, Moss SF (2021) AGA clinical practice update on the management of refractory Helicobacter pylori infection: Expert review. Gastroenterology 160:1831-1841.
- Tiwari SK, Khan AA, Ibrahim M, Habeeb MA, Habibullah CM (2006) Helicobacter pylori and other Helicobacter species DNA in human bile samples from patients with various hepato-biliary diseases. World J Gastroenterol 12: 2181-2186.
- Wang L, Chen J, Jiang W, Cen L, Pan J, et al. (2021) The Relationship between Helicobacter pylori infection of the gallbladder and chronic cholecystitis and cholelithiasis: A Systematic review and meta-analysis. Can J Gastroenterol Hepatol 2021: 1-11.
- Attaallah W, Yener N, Ugurlu MU, Manukyan M, Asmaz E, et al. (2013) Gallstones and concomitant gastric Helicobacter pyloriinfection. Gastroenterol Res Pract 2013: 1-4.
- Waluga M, Kukla M, Żorniak M, Bacik A, Kotulski R (2015) From the stomach to other organs: Helicobacter pylori and the liver. World J Hepatol 7: 2136-2146.
- Avenaud P, Marais A, Monteiro L, Le Bail B, Bioulac Sage P, et al. (2000) Detection of Helicobacter species in the liver of patients with and without primary liver carcinoma. Cancer 89: 1431-1439.
- Nilsson I, Lindgren S, Eriksson S, Wadström T (2000) Serum antibodies to Helicobacter hepatic us and Helicobacter pylori in patients with chronic liver disease. Gut 46: 410-414.
- Lee JW, Lee DH, Lee JI, Jeong S, Kwon KS, et al. (2010) Identification of Helicobacter pylori in gallstone, bile and other Hepatobiliary tissues of patients with cholecystitis. Gut Liver 4: 60-67.
- Chen DF, Hu L, Yi P, Liu WW, Fang DC, et al. (2007) H. pylori exist in the gallbladder mucosa of patients with chronic cholecystitis. World J Gastroenterol 13: 1608-16011.
- Jahantab MB, Safaripour AA, Hassanzadeh S, Yavari Barhaghtalab MJ (2021) Demographic, chemical and Helicobacter pyloripositivity assessment in different types of gallstones and the bile in a random sample of cholecystectomied iranian patients with cholelithiasis. Can J Gastroenterol Hepatol 2021: 1-8.
- Iriz E, Cirak MY, Engin ED, Zor MH, Erer D, et al. (2008) Detection of Helicobacter pylori DNA in aortic and left internal mammary artery biopsies. Tex Heart Inst J 35: 130-135.
- Danesh J, Wong Y, Ward M, Muir J (1999 ) Chronic infection with Helicobacter pylori, chlamydia pneumonia, or cytomegalovirus: Population-based study of coronary heart disease. Heart 81: 245-247.
- Jahantab MB, Salehi V, Mehrabi S, Abedini L, Yavari Barhaghtalab MJ (2020) Cholecystomegaly: A case report and review of the literature. Case Rep Gastrointest Med 2020: 1-5.
- Sabbaghian MS, Rich BS, Rothberger GD, Cohen J, Batash S, Kramer E, et al. (2008) Â Evaluation of surgical outcomes and gallbladder characteristics in patients with biliary dyskinesia. J Gastrointest Surg 12: 1324-1330.
- Chen DF, Hu L, Yi P, Liu WW, Fang DC, et al. (2007) H. pylori are associated with chronic cholecystitis. World J Gastroenterol 13: 1119-1122.
- Moricz Ad, Melo M, Castro AM, Campos T, Silva RA, et al. (2010) Prevalence of Helicobacter spp in chronic cholecystitis and correlation with changes on the histological pattern of the gallbladder. Acta Cir Bras 25: 218-224.
- Motie M, Rezapanah A, Abbasi H, Memar B, Arianpoor A, et al. (2017) The Relationship between cholecystitis and presence of Helicobacter pylori in the gallbladder. Zahedan J Res Med Sci 19: e9621.
- Zhang FM, Yu CH, Chen HT, Shen Z, Hu FL, et al. (2015) Helicobacter pylori infection is associated with gallstones: Epidemiological survey in China. World J Gastroenterol 21: 8912-8919.
- Kawaguchi M, Saito T, Ohno H, Midorikawa S, Sanji T, et al. (1996) Bacteria closely resembling Helicobacter pylori detected immunohistologically and genetically in resected gallbladder mucosa. J Gastroenterol 31: 294-298
- Bulajic M, Maisonneuve P, Schneider-Brachert W, Müller P, Reischl U, et al. (2002) Helicobacter pylori and the risk of benign and malignant biliary tract disease. Cancer 95: 1946-1953.
- Abayli B, Colakoglu S, Serin M, Erdogan S, Isiksal YF, et al. (2005) Helicobacter pylori in the etiology of cholesterol gallstones. J Clin Gastroenterol 39: 134-137.
- Figura N, Cetta F, Angelico M, Montalto G, Cetta D, et al. (1998) Most Helicobacter pylori-infected patients have specific antibodies, and some also have H. pylori antigens and genomic material in bile: Is it a risk factor for gallstone formation? Dig Dis Sci 43: 854-862.
- Kate V, Maroju NK, Ananthakrishnan N (2013) Helicobacter pyloriinfection and upper gastrointestinal disorders. Gastroenterol Res Pract 2013: 1-3.
- Méndez-Sánchez N, Pichardo R, González J, Sánchez H, Moreno M, et al. (2001) Lack of association between Helicobacter sp colonization and gallstone disease. J Clin Gastroenterol 32:138-141.
- Myung SJ, Kim MH, Shim KN, Kim YS, Kim EO, et al. (2000) Detection of Helicobacter pylori DNA in human biliary tree and its association with hepatolithiasis. Dig Dis Sci 45:1405-1412.
- Fallone CA, Tran S, Semret M, Discepola F, Behr M, et al. (2003) Helicobacter DNA in bile: Correlation with hepato-biliary diseases. Aliment Pharmacol Ther 17: 453-458.
- Yucebilgili K, MehmetoÄlu T, Gucin Z, Salih BA. (2009) Helicobacter pylori DNA in gallbladder tissue of patients with cholelithiasis and cholecystitis. J Infect Dev Ctries 3: 856-859.
- Roosendaal R, Kuipers EJ, Vandenbroucke-Grauls CM, Kusters JG (2002) Helicobacter species are not detectable by 16S rDNA PCR in bile from Dutch patients with common bile duct stones. Digestion 66: 89-91.
- Rudi J, Rudy A, Maiwald M, Stremmel W (1999) Helicobacter sp. are not detectable in bile from German patients with biliary disease. Gastroenterology 116: 1016-1017.
- Cen L, Pan J, Zhou B, Yu C, Li Y, et al. (2018) Helicobacter Pylori infection of the gallbladder and the risk of chronic cholecystitis and cholelithiasis: A systematic review and meta-analysis. Helicobacter. 2018 23: e12457.
- Sabbaghian MS, Ranaudo J, Zeng L, Alongi AP, Perez-Perez G, et al. (2010) Identification of Helicobacter spp. in bile and gallbladder tissue of patients with symptomatic gallbladder disease. HPB 12: 129-133.
- Kanthan R, Senger JL, Ahmed S, Kanthan SC (2015) Gallbladder cancer in the 21st century. J Oncol 2015: 1-26.
- De Martel C, Plummer M, Parsonnet J, Van Doorn LJ, Franceschi S (2009) Helicobacter species in cancers of the gallbladder and extrahepatic biliary tract. Br J Cancer 100: 194-199.
- Mishra RR, Tewari M, Shukla HS (2010) Helicobacter species and pathogenesis of gallbladder cancer. Hepatobiliary Pancreat Dis Int 9: 129-134.
- Cherif S, Bouriat K, Rais H, Elantri S, Amine S(https://doi.org/10.1155/2020/9287157) Helicobacter pylori and Biliary Tract Cancers: A Meta-analysis. Can J Infect Dis Med Microbiol 2020: 1-7.
- Hassan EH, Gerges SS, El-Atrebi KA, El-Bassyouni HT (2015) The role of H. pyloriinfection in gall bladder cancer: Clinicopathological study. Tumour Biol 36: 7093-7098.
- Boonyanugomol W, Chomvarin C, Baik SC, Song JY, Hahnvajanawong C, et al. (2011) Role of cagA-positive Helicobacter pylori on cell proliferation, apoptosis, and inflammation in biliary cells. Dig Dis Sci 56: 1682-1692.
- Zhou D, Guan WB, Wang JD, Zhang Y, Gong W, et al. (2013) A comparative study of clinicopathological features between chronic cholecystitis patients with and without Helicobacter pylori infection in gallbladder mucosa. PLoS One 8: e70265.
- Labigne A, Cussac V, Courcoux P (1991) Shuttle cloning and nucleotide sequences of Helicobacter pylori genes responsible for urease activity. J Bacteriol 173: 1920-1931.
Citation: Jahantab MB, Hosseinpour R, Iraji C, Safaripour AA, Yavari Barhaghtalab MJ (2021) Helicobacter pylori Infection and Gallbladder Diseases: A Mini- Review. J Oncol Res Treat S5: 005.
Copyright: © 2021 Jahantab MB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 4844
- [From(publication date): 0-2021 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 4085
- PDF downloads: 759