Research Article Open Access
Idiopathic Granulomatous Mastitis, a Clinicopathological Review of 22 Cases
Fariba Binesh1, Saied Kargar2, Shokouh Taghipour Zahir1, Nasim Behniafard3*, Hossein Navabi4 and Saied Arefanian41Department of Pathology, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2Department of Surgery Shahid Sadoughi University of medical sciences, Yazd, Iran
3Researcher of Research and development Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
4General practitioner, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
- *Corresponding Author:
- Nasim Behniafard
Research and development Center
Shahid Sadoughi Hospital, Avicenna Blv
Safaeeh, Yazd, Iran
Tel: +983518113368
Fax: +983518224100
E-mail: nbehniafard@gmail.com
Received Date: January 04, 2014; Accepted Date: January 29, 2014; Published Date: January 31, 2014
Citation: Binesh F, Kargar S, Zahir ST, Behniafard N, Navabi H, et al. (2014) Idiopathic Granulomatous Mastitis, a Clinicopathological Review of 22 Cases. J Clin Exp Pathol 4:157. doi: 10.4172/2161-0681.1000157
Copyright: © 2014 Binesh F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Background: Idiopathic granulomatous mastitis is a rare chronic inflammatory disease and typically occurs in women at the reproductive life. The etiology, clinical course, and optimal treatment of this disorder remain obscure. The most common clinical presentation is a unilateral, firm, discrete breast mass, often associated with inflammation of the overlying skin. Because clinically the lesion can simulate carcinoma, definitive diagnosis is made using histopathology. The main purpose of this study was to present the clinicopathological features of patients with idiopathic granulomatous mastitis, as well as the authors’ experience with surgical treatment of these patients.
Methodology: The unit’s pathology database and clinic letters for the time period from January 2005 to May 2010 were used to identify patients who had presented with idiopathic granulomatous mastitis. Results: 22 female patients with a mean age of 35.14 ± 6.07 were included. The patients ranged in age from 24 to 44 years. All patients were parous, the median number of their pregnancies was 2 (ranging from 2 to 6) and the median duration of the last delivery was 4 years (ranging from 1.4 to 14 years).19 patients had a history of breast feeding. 8 patients (36.4%) had used hormonal contraception. The right breast was involved in 8 (36.4%) cases and in 12 (54.5%) patients; the left breast was affected. Erythema was the most common presenting symptom. Surgery was the definitive procedure in all patients. 13 patients (61.9%) presented with recurrence.
Conclusion: Increased recognition of this disease will improve its understanding and management of it. Longterm follow-up is necessary.
Keywords
Idiopathic; Granulomatous Mastitis; Breast disease
Introduction
Idiopathic Granulomatous Mastitis(IGM) is a rare and benign disease, except few cases were reported in men [1] is usually seen during pregnancy or lactation period [2]. The cause of this uncommon lesion is obscure [3]. It usually presents as a mass. Clinically the lesion can simulate carcinoma. This lesion is characterized histologically by primary lobulocentric granulomas which often contain neutrophils. Foci of necrosis may be present within the granuloma, but true caseous necrosis is not seen. Although the lobulocentricity of the granulomas and the presence of neutrophils should raise the possibility of IGM, other causes of granulomatous inflammation (such as infection, sarcoidosis and reaction to foreign materials) should always be excluded. The aim of this study was to review the clinical presentation of IGM, its histopathological features and to outline the diagnostic and therapeutic considerations in the management of this potentially recurrent nonmalignant breast disease.
Methodology
This work was carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association and was approved ethically by the university ethics committee. This retrospective study included 22 patients who were pathologically diagnosed as IGM from 2005 to 2010 in two private hospitals – Mojibian Hospital and Mortaz Hospital – and a private surgical clinic in Yazd, Iran. Presenting patients were diagnosed either after biopsy study with suspicion of malignancy, or pathologic study after a no complete response to antibiotic treatment due to a breast abscess suspicion. Pathologic diagnosis of IGM and ruling out the other possible causes of granuloma formation were considered as inclusion criteria. Definitive diagnosis was based on excisional biopsy from the affected breast. We consider open biopsy to be the safest method to rule out malignancy. The histological diagnosis of granulomatous mastitis was made when noncaseating, nonvasculitic granulomatous inflammatory reaction, composed of epithelioid cells, lymphocytes, and foreign body type of giant cells, centered mainly on breast lobules. Microabscess formation was noted in some of the cases. Special stains (Gram, Ziehl-Neelsen, and periodic acid-Schiff) for microorganisms were negative. Purified Protein Derivative (PPD) and cytoplasmic ANCA (C-ANCA) tests were performed for all patients. In this study, surgical excision and antibiotics were the primary treatment modalities. Patients with inflammatory findings, but without abscess findings were initially received antibiotic regimen of metronidazole and ciprofloxacin for at least one month. In case of no regression and negative culture (with probability of fastidious nature of certain microbes), the treatment would be changed to Cefuroxime and Clindamycin. Ultrasonography-assisted aspiration or surgical drainage was performed in patients with abscess findings at the time of diagnosis and in whom the diagnosis of abscess was confirmed by ultrasonographic examination. Wide local excision to obtain diseasefree margins was performed in patients with an isolated mass without the presence of skin changes. In cases with limited disease, this approach was sufficient .However in patients with locally advanced disease; the patients subsequently underwent reconstructive surgery. No patient received corticosteroids or methotrexate in this study. Posttreatment response was monitored both clinically and radio logically with a breast ultrasound every month.
Patients’ data for age, number of parity, the time interval between the last pregnancy and presentation of the signs and symptoms, presenting symptoms, involved side of the disease and recurrence were collected from the patients’ medical files. Patients’ age is presented as mean and Standard Deviation (SD). The data is shown as median and range for variables that violated the assumption of normality. Statistical analysis included frequency table (for descriptive analysis) and Fischer exact test (for analytical analysis). The level of significance was defined at P<0.05. Statistical analysis was performed using SPSS software, version 16 (SPSS Inc., Chicago, IL).
Results
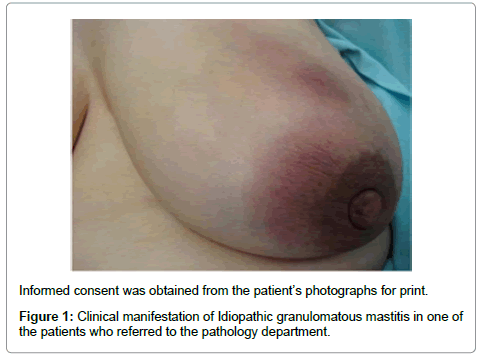
Complete information for 21 patients diagnosed with IGM with regard to the clinical presentation (Figure 1), histology report, and management was obtained .In one case no history regarding breastfeeding was available. One case gave a history of hypothyroidism and another patient suffered from rheumatoid arthritis. The patients ranged in age from 24 to 44 years. The mean age was 35.14 ± 6.07 years. All patients were parous, the median number of their pregnancies was 2 (ranging from 2 to 6) and the median duration from the last delivery was 4 years (ranging from 1.4 to 14 years) .19(86.4%) patients gave a history of breast feeding of variable duration.8 patients (36.4%) had a history of hormonal contraception consumption. The right breast was involved in 8 cases and in 12 cases, the left breast was affected. 2 of patients had bilateral disease. Erythema was the most common presenting symptom .Six of the patients had pain, Erythema and bulging, and three patients presented with all four symptoms of pain, Erythema, mass, and bulging. Purified Protein Derivative (PPD) and cytoplasmic ANCA (C-ANCA) tests were negative in all of our patients. In addition there were no radiological findings suggestive of sarcoidosis, Wegener’s granulomatosis or tuberculosis. 13 patients (61.9%) had recurrence in their follow up course. The median time for recurrence was 4 months after treatment (ranging from 1 to 16 months). In the age group over 35 years, recurrence was more than the age group under 35 years but this difference was not significant(PV=0.187).Patients who did not take oral contraceptive pills (OCP) had more recurrence than those who were taking pill but the difference failed to reach statistical significance (PV=0.052). Regarding parity and recurrence rate, there was no significant difference between group with 2 pregnancies and group with more than 2 pregnancies (PV=1.000) (Table 1).
| Recurrence | Yes | No | Sum | P value | |
|---|---|---|---|---|---|
| Variant | N (%) | N (%) | N (%) | ||
| OCP | Yes | 2(28.6%) | 5(71.4%) | 7(100 %) | 0.052 |
| No | 12(80%) | 3(20%) | 15(100 %) | ||
| Age | <35 | 4(44.4 %) | 5(55.6%) | 9(100%) | 0.187 |
| >35 | 10(76.92%) | 3 (23.08%) | 13 (100%) | ||
| Parity | 2 | 8(66.7%) | 4(33.3%) | 12(100%) | 1 |
| >2 | 6(60%) | 4(40%) | 10(100%) | ||
Table 1: The association between recurrence and OCP consumption, age and parity. Fischer exact test.
Discussion
Breast granuloma is present in less than 1% of breast biopsies [4]. There are two types of granulomatous mastitis, specific and idiopathic. IGM was first described as a specific entity by Kessler and Wolloch in 1972 [3]. It was further elaborated by Cohen C in 1977 [5]. Approximately 200 cases of IGM have been reported in the literature during the past 3 decades, with most of them being reported in developing countries. Although no ethnic predisposition has been documented, prevalence of IGM in specific ethnic populations is observed; many reports come from Eastern countries. All of our patients were Iranian. IGM usually affects women of childbearing age. The mean age of our patients was 35.14 ± 6.07 years which was comparable to that in previous studies [2]. However we found reports of patients as young as 11 years-old [6] and as old as 80 years [7]. Although its etiology is still unknown, several mechanisms have been postulated including autoimmunity [8], infective process [9] and a local reaction to chemical secretions [10]. For example there are some reports which describe the association of granulomatous lobular mastitis with Erythema nodosum and polyarthritis, thus highlighting an autoimmune cause [11,12]. In our series one case had a history of hypothyroidism and another patient suffered from rheumatoid arthritis. However, serologic tests for antinuclear antibodies and rheumatic factor are usually negative [13]. Its association with the use of oral contraceptive pills, hyperprolactinaemia and α1-Antitrypsin deficiency has been suggested [14-16]. In the other word, some authors suggest that most of the patients were suffering from hormonal perturbation. Oral contraceptives induce hyperplasia in the lobular ductule, thus leading to the obstructive desquamation of the ductules, distention of the ductules and perilobular inflammatory reactions [17]. However most of the studies show conflicting data associating the role of oral contraceptive pills in patients diagnosed with IGM, ranging from 0% to 33% [14]. In addition IGM has also been reported to occur in patients who did not receive hormonal contraception [18]. In the current study 8 patients (36.4%) had a history of hormonal contraception consumption. Correlations between IGM, pregnancy and breastfeeding have all been postulated but never proven. Bani-Hani et al. [14] reported pregnancy in 17%, and nursing in a similar 17% at the time of diagnosis. In another series, none of the cases that were considered as IGM had a history of pregnancy or nursing [19]. In our study all patients were parous and the median number of their pregnancies was 2.19 of our patients gave a history of breast feeding of variable duration. The time between the last childbirth and first symptoms ranges from 2 months to 15 years [13]. All the cases described by Kessler and Wolloch and Fletcher occurred within 6 years of pregnancy. Most of our patients were diagnosed within 5 years of their last childbirth. This disease is usually unilateral but it has been known to occur in both breasts [20]. There were 2 cases with bilateral breasts involvement in our study.
IGM may manifest itself in two ways: as an abscess or mass. 27.27% of our patients had sign of abscess and 55% had breast mass. Mammography and sonography can aid in the diagnosis, but are not definitive. Focal asymmetry without a mass on mammography and heterogeneous echo pattern on sonography is the most common imaging finding in IGM [21]. MRI is not conclusive; it usually shows a heterogeneous enhancing area with ring-like enhancing abscesses [22]. As a result a definite diagnosis could not be made until examination of excisional biopsy. Various techniques of biopsy are used in the diagnosis of IGM. Fine needle aspiration biopsy is the least invasive method [23], but can yield confusing results which often necessitate confirmation by open biopsy. Core biopsy is used with a good success rate. We consider open biopsy to be the safest method to rule out malignancy. Breast carcinoma and abscess are the two main differential diagnoses of IGM. As a matter of fact the diagnosis of idiopathic granulomatous mastitis is one of exclusion. In the other word all known causes of granulomatous changes should be excluded before the diagnosis of IGM is made [21]. PPD was negative in all of our patients and there were no radiological findings suggestive of sarcoidosis or TB. There are a few evidences that suggest the probability that IGM could be a precursor for malignancy [22]. Recurrence is a well known complication of IGM. In the current study13 patients (61.9%) had recurrence in their follow up course. We have evaluated factors influencing the recurrence .We found patients who had not taken OCP had more recurrence than those who were taking pill but the difference failed to reach statistical significance (PV=0.052).This is perhaps due to their age, parity or some other factors which are unknown now. There was also a difference in recurrence rate based on patient’s age which was not statistically significant (PV=0.187). Little is known about the optimal therapy and there is no definite accepted treatment for IGM. Surgical excision can be therapeutic as well as useful in providing an exact diagnosis. Wilson, et al. [23,24] showed that the most commonly used approach in treatment of IGM is wide excision of the affected area with a success rate of 79%. Ocal et al. [2] treated 16 IGM patients with surgery. They revealed that 4 patients required quadrantectomy, and 75% of the patients needed reoperation either for completion of the excision after surgical drainage or for recurrence. Kok and Telisinghe [25] performed surgical therapy on 40 of 43 patients with IGM. 10 (23%) of the patients had recurrences which were again treated with surgery. The high incidence of recurrence necessitates extensive resection to obtain disease-free margins. Surgical complications include skin ulceration, abscess formation and recurrence. In 1980 short course of high dose prednisone (60 mg/day) was recommended [23]. However Akbulut et al. [26] retrospectively analysed 541 IGM cases treated with steroids between 1972 and 2010. They found a high recurrence rate in patients using steroids, and also the occurrence of adverse side effects such as steroid-induced diabetes mellitus. Other treatments have included use of methotrexate as a steroid sparing agent in patients who relapsed after tapering steroid [27]. But it should be noted that the natural history of IGM can be self limited and 50% of cases recover without complication [24,28]. A retrospective review of cases seen over 25 years by Al-Khaffaf et al. showed that regardless of therapeutic intervention, which included steroids, antibiotics, and surgical intervention alone or in combinations, the condition takes about 6 to 12 months to resolve completely [28]. In our experience 9 patients responded well to surgery while the others recurred. Our findings showed that surgery is not always effective and it is associated with a high recurrence rate.
Conclusion
IGM is a rare and benign inflammatory breast disease which is commonly mistaken for malignancy and other diseases. Correct diagnosis requires the exclusion of infection diseases and other causes of granulomatous mastitis. Recurrence is a well known complication of the IGM. Factors affecting recurrence is not well known. There is no consensus about appropriate treatment, but in our study surgery was associated with a high recurrence rate so corticosteroids and in refractory cases immunosuppressive drugs may be effective.
References
- Reddy KM, Meyer CE, Nakdjevani A, Shrotria S (2005) Idiopathic granulomatous mastitis in the male breast. Breast J 11: 73.
- Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, et al. (2010) Granulomatous mastitis: clinical, pathological features, and management. Breast J 16: 176-182.
- Kessler E, Wolloch Y (1972) Granulomatous mastitis: a lesion clinically simulating carcinoma. American journal of clinical pathology 58: 642-646.
- Elsiddig KE, Khalil EA, Elhag IA, Elsafi ME, Suleiman GM, et al. (2003) Granulomatous mammary disease: ten years' experience with fine needle aspiration cytology. The international journal of tuberculosis and lung disease: the official journal of the International Union against Tuberculosis and Lung Disease 7: 365-369.
- Cohen C (1977) Granulomastitis: a review of five cases. S Afr Med J 52: 15-16.
- Katz U, Molad Y, Ablin J, Ben-David D, Paran D, et al. (2007) Chronic idiopathic granulomatous mastitis. Ann N Y Acad Sci 1108: 603-608.
- Asoglu O, Ozmen V, Karanlik H, Tunaci M, Cabioglu N, et al. (2005) Feasibility of surgical management in patients with granulomatous mastitis. Breast J 11: 108-114.
- Brown KL, Tang PH (1979) Postlactational tumoral granulomatous mastitis: a localized immune phenomenon. Am J Surg 138: 326-329.
- Fletcher A, Magrath IM, Riddell RH, Talbot IC (1982) Granulomatous mastitis: a report of seven cases. J Clin Pathol 35: 941-945.
- Rowe PH (1984) Granulomatous mastitis associated with a pituitary prolactinoma. Br J Clin Pract 38: 32-34.
- Binesh F, Shiryazdi M, Bagher Owlia M, Azimi S (2013) Idiopathic granulomatous mastitis, erythema nodosum and bilateral ankle arthritis in an Iranian woman. BMJ Case Rep 2013.
- Olfatbakhsh A, Beheshtian T, Djavid GE (2008) Granulomatous mastitis, erythema nodosum, and oligoarthritis in a pregnant woman. Breast J 14: 588-590.
- Verfaillie G, Breucq C, Sacre R, Bourgain C, Lamote J (2006) Granulomatous lobular mastitis: a rare chronic inflammatory disease of the breast which can mimic breast carcinoma. Acta Chir Belg 106: 222-224.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ (2004) Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J 10: 318-322.
- Cserni G, Szajki K (1999) Granulomatous Lobular Mastitis Following Drug-Induced Galactorrhea and Blunt Trauma. Breast J 5: 398-403.
- Diesing D, Axt-Fliedner R, Hornung D, Weiss JM, Diedrich K, et al. (2004) Granulomatous mastitis. Arch Gynecol Obstet 269: 233-236.
- Jain DKlP, Pancholi M, Mishra H (2007) Diagnostic Dilemma of rapidly progressive ulcer of breast.
- Sato N, Yamashita H, Kozaki N, Watanabe Y, Ohtsuka T, et al. (1996) Granulomatous mastitis diagnosed and followed up by fine-needle aspiration cytology, and successfully treated by corticosteroid therapy: report of a case. Surgery today 26: 730-733.
- Elif Ülker Akyildiz FA, Sennur Ilvan, Zerrin Calay (2010) Idiopathic Granulomatous Mastitis. The Journal of Breast Health 6: 5-8.
- Yip CH, Jayaram G, Swain M (2000) The value of cytology in granulomatous mastitis: a report of 16 cases from Malaysia. Aust N Z J Surg 70: 103-105.
- Heer R, Shrimankar J, Griffith CD (2003) Granulomatous mastitis can mimic breast cancer on clinical, radiological or cytological examination: a cautionary tale. Breast 12: 283-286.
- Kocaoglu M, Somuncu I, Ors F, Bulakbasi N, Tayfun C, et al. (2004) Imaging findings in idiopathic granulomatous mastitis. A review with emphasis on magnetic resonance imaging. J Comput Assist Tomogr 28: 635-641.
- Agale SV, Momin YA, Khan WA (2009) Cytology of Idiopathic Granulomatous Mastitis: A Report of a Case Masquerading as Carcinoma. Bombay Hospital Journal 51: 105.
- Wilson JP, Massoll N, Marshall J, Foss RM, Copeland EM, et al. (2007) Idiopathic granulomatous mastitis: in search of a therapeutic paradigm. Am Surg 73: 798-802.
- Kok KY, Telisinghe PU (2010) Granulomatous mastitis: presentation, treatment and outcome in 43 patients. Surgeon 8: 197-201.
- Akbulut S, Arikanoglu Z, Senol A, Sogutcu N, Basbug M, et al. (2011) Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis? Arch Gynecol Obstet 284: 1189-1195.
- Kaur AC, Dal H, Müezzinoglu B, Paksoy N (1999) Idiopathic granulomatous mastitis. Report of a case diagnosed with fine needle aspiration cytology. Acta Cytol 43: 481-484.
- Mazlan L, Suhaimi SN, Jasmin SJ, Latar NH, Adzman S, et al. (2012) Breast carcinoma occurring from chronic granulomatous mastitis. Malays J Med Sci 19: 82-85.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 15244
- [From(publication date):
March-2014 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10536
- PDF downloads : 4708