Image Guided Needle Biopsies for Musculoskeletal Soft Tissue Lesions: A 9-year analysis of Non-Diagnostic Biopsies
Received: 02-Apr-2022 / Manuscript No. joo-22-59346 / Editor assigned: 04-Apr-2022 / PreQC No. joo-22-59346 (PQ) / Reviewed: 21-Apr-2022 / QC No. joo-22-59346 / Revised: 26-Apr-2022 / Manuscript No. joo-22-59346 (R) / Published Date: 03-May-2022 DOI: 10.4172/2472-016X.1000168
Abstract
Background: Non-diagnostic (ND) musculoskeletal biopsies of soft tissue lesions can increase patient anxiety and delay definitive diagnosis and treatment. It is thought the specific histotype of the lesion may influence accuracy of the biopsy. This study aims to assess if ND musculoskeletal biopsies are more likely to represent benign or malignant conditions, and whether specific diseases are more likely to result in a non-diagnostic biopsy result.
Material and methods: This was a retrospective study of patients in a regional bone and soft tissue tumour unit between March 2010 and September 2019. Biopsies were done using clinical guidance by the surgical team (performed using clinical landmarks instead of image-guidance), or image-guidance (ultrasound or CT) by a musculoskeletal radiologist. Non-diagnostic biopsies were identified, and the final diagnosis was categorised as benign or malignant; the final tissue diagnosis was recorded.
Results: A total of 1,561 cases underwent biopsy of soft tissue lesions, mean age 57. Further biopsies were done in 30 cases (2%). Benign diagnoses were more commonly identified in non-diagnostic biopsies (23 cases (77%)). Vascularised, cystic and myxoid lesions appeared most frequently, and haematomas/ arteriovenous malformation were significantly more likely to need two biopsies. Over half (16 cases) of non-diagnostic biopsies were done without imageguidance.
Conclusion: This study shows that, for non-diagnostic musculoskeletal biopsies, a benign diagnosis is more common than malignant. The most frequent lesions with non-diagnostic biopsies were mainly myxoid, cystic and vascular lesions, and in these cases, we feel image-guidance may improve accuracy.
Keywords
Introduction
Despite modern imaging techniques having a good predictive value in the differential diagnosis of musculoskeletal soft tissue lesions, an accurate biopsy and histology remains essential to confirm the diagnosis and plan management [1- 3]. Image-guided biopsies have become the first-line method in diagnosing musculoskeletal tumours and confer several advantages over traditional open surgical biopsy techniques [4]. These include the reduced cost and complication rates [4], improved recovery [2], and improved accuracy in some cases [5].
However, non-diagnostic (ND) biopsies can lead to a diagnostic conundrum for clinicians [6]. They can increase patient anxiety [4], and delay definitive diagnosis and treatment, which may further impact on outcomes and survival [6]. Furthermore, a ND biopsy may necessitate further image-guided or open biopsy, which increases both patient risk and healthcare costs [7].
ND biopsies can be related to several factors, including inadequate technique [7,8],or a specific pathological process that is difficult to diagnose due to a small amount of tissue [7]. Technical factors include failure to biopsy the lesion, or obtain sufficient material for definitive diagnosis [8], and tissue damage during biopsy can contribute to necrosis or crush artefact [8]. Several authors have analysed the diagnostic yield for musculoskeletal lesions and technical factors associated with it, such as number of samples taken [2, 9] and length of sample taken [9].
However, the specific histotype of the lesion is also thought to influence the accuracy of the needle biopsy [1]. Pathological conditions difficult to diagnose in the literature include vascularised lesions [10] or cystic lesions [7]. Vascularised lesions may result in haemorrhagic tissue, which poses a challenging diagnostic question [10], and, previous authors have commented on the difficulty in obtaining solid material for diagnosis for cystic bone lesions [7]. Similarly, soft tissue lesion biopsies containing myxoid stroma have been shown to be less informative than non-myxoid lesions [11]. The hypocellular myxoid tissue can represent benign (intramuscular myxoma) or malignant tumours (myxoid sarcoma) making a definitive diagnosis potentially difficult [11].
This study aims to assess if ND musculoskeletal biopsies are more likely to represent benign or malignant conditions, and whether specific diseases are more likely to result in a non-diagnostic biopsy result. Further analysis will assess if the frequency of these diagnoses differs between cases needing multiple biopsies compared to those who required a single biopsy.
Methods
This was a retrospective study, using prospectively collected data on the tumour database for a regional bone and soft tissue tumour unit. The study is part of a larger project approved by the Health Research Authority (20/HRA/4857). All of the cases that underwent soft tissue biopsy between March 2010 and September 2019 (to allow for a follow up period of one year) were reviewed for possible inclusion in the study.
Cases in which more than one biopsy was needed for a definitive diagnosis were included for analysis. A biopsy was defined as diagnostic if it provided a clear histological diagnosis, or was clinically useful for guiding patient management e.g. tissue sample was adequate for the multi-disciplinary team (MDT) to confidently exclude features of malignancy. Following identification of relevant cases, demographic and clinical details were collected for all cases. All histology reports and MDT notes were reviewed to ascertain technical reasons for a ND biopsy.
Technical Aspects
Biopsies were done either in clinic, using clinical guidance (performed using clinical landmarks instead of image-guidance) by the surgical team using Bard Care-Max-Core® biopsy instruments, or under ultrasound or CT guidance by an MSK radiologist with local anaesthesia. Using image guidance, the needles used were typically 14-gauge soft tissue core biopsy needles, such as those supplied by Temno™. On individual choice, an automatic spring-loaded core biopsy needle was sometimes used, such as those supplied by Achieve®.
All biopsy specimens were dual reported by two consultant histopathologists with specialist expertise in musculoskeletal tumours and sarcomas. Further discussion took place in the MDT meeting, and the final diagnosis was prospectively recorded in the departmental database. In cases where there was suspicion of a haematological disease the specimen was sent for specialist hematopathologic review.
Statistical Analysis
Data was extracted from the database and collated. Analysis was performed using R statistical software (R Foundation, Vienna, Austria). Categorical outcomes were evaluated using Chi-squared tests. Fisher’s exact test was used to compare frequency of diagnoses between cases needing multiple biopsies, and those needing a single biopsy. A p-value of less than 0.05 was deemed statistically significant.
Results
A total of 1,561 cases underwent biopsy during the study period in the unit, mean age 56.6 (range 4-99). The mean follow-up was 1.1 years. Overall, 30 patients (2%) required more than one biopsy. The definitive diagnosis was benign in 23 cases (77%). A summary of the final diagnosis is provided in Table 1.
| Diagnosis | Frequency (%) |
|---|---|
| Haematoma/AVM | 5(17) |
| Sarcoma* | 5(17) |
| Myxoma | 2(17) |
| Tenosynovial GCT(TSGCT) | 2(17) |
| Ganglion | 2(17) |
| Other malignancies** | 2(7) |
| Other benign processes*** | 8(27) |
| Non-diagnostic**** | 4(14) |
| * 2 low grade fibromyxoid sarcoma, 2 pleomorphic sarcoma, 1 myxofibrosarcoma | |
| ** lymphomproliferative, 1 metastatic melanoma | |
| *** I heteropic ossification, 1 lipoma, 1 nodular fasciitis, 1 nuchal fibroma, 1 Schwannoma, 1 Synovial osteochondromatosis, 1 synovitis, 1 degenerative change | |
| **** No definitive histological diagnosis could be made on the original or subsequent biopsy. Clinical and imaging follow-up for mean of 1.1 years for soft tissue biopsies revealed no adverse cahnge in the imaging and clinical characteristics, supporting a benign diagnosis. | |
Table 1: Non-diagnostic soft tissue biopsy results.
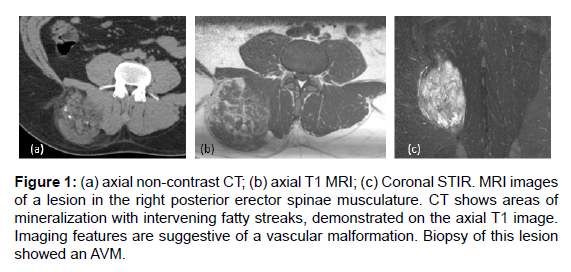
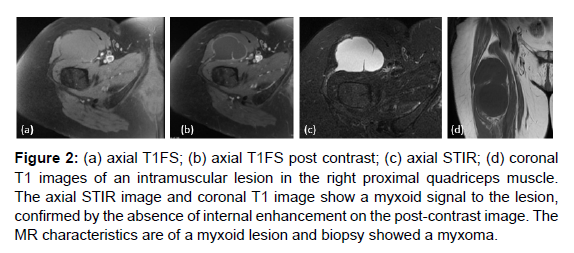
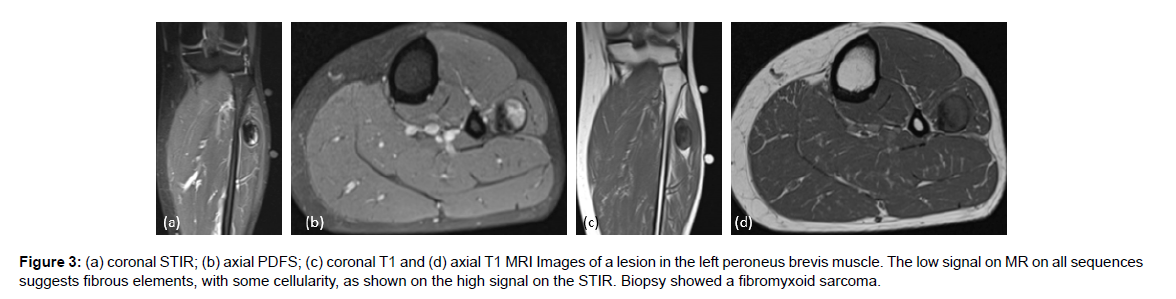
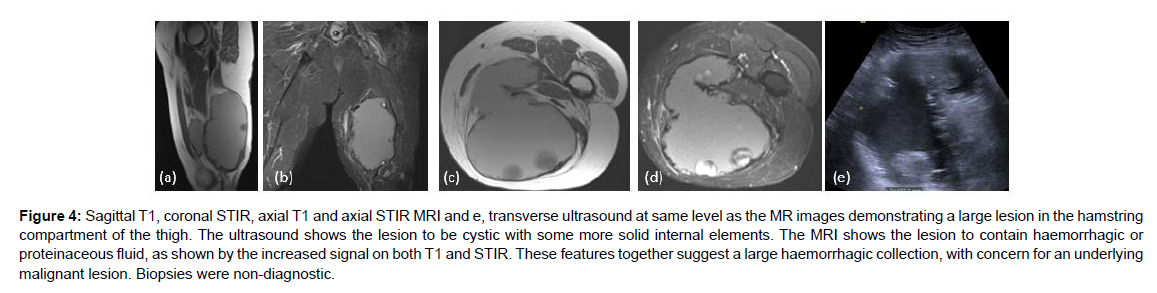
A further analysis was made, comparing frequency of diagnosis in patients requiring multiple biopsies, to a single biopsy and is summarised in Table 2. For soft tissue lesions, haematoma/AVM and ganglia were more likely to require a second biopsy. Examples of imaging are shown in Figures 1-4.
| Diagnosis | Number in multiple biopsy group | Number in single biopsy group | p-value (Fisher’s exact test) |
|---|---|---|---|
| Haematoma/ AVM | 5 | 49 | 0.03 |
| Sarcoma | 5 | 310 | 0.819 |
| Myxoma | 2 | 45 | 0.228 |
| TSGCT | 2 | 52 | 0.278 |
| Ganglion | 2 | 12 | 0.028 |
| Other malignancies | 2 | 195 | 0.575 |
| Other benign processes | 8 | 868 | 0.001 |
| Non-diagnostic | 4 | ||
| Total | 30 | 1531 |
Table 2: Soft tissue results for cases requiring multiple versus a single biopsy.
Figure 1: (a) axial non-contrast CT; (b) axial T1 MRI; (c) Coronal STIR. MRI images of a lesion in the right posterior erector spinae musculature. CT shows areas of mineralization with intervening fatty streaks, demonstrated on the axial T1 image. Imaging features are suggestive of a vascular malformation. Biopsy of this lesion showed an AVM.
Figure 2: (a) axial T1FS; (b) axial T1FS post contrast; (c) axial STIR; (d) coronal T1 images of an intramuscular lesion in the right proximal quadriceps muscle. The axial STIR image and coronal T1 image show a myxoid signal to the lesion, confirmed by the absence of internal enhancement on the post-contrast image. The MR characteristics are of a myxoid lesion and biopsy showed a myxoma.
Modes of biopsy are summarised in Table 3. In soft tissue cases no documented reasons for need for re-biopsy were seen in the primary histology reports or MDT discussion notes.
Figure 3: (a) coronal STIR; (b) axial PDFS; (c) coronal T1 and (d) axial T1 MRI Images of a lesion in the left peroneus brevis muscle. The low signal on MR on all sequences suggests fibrous elements, with some cellularity, as shown on the high signal on the STIR. Biopsy showed a fibromyxoid sarcoma.
Figure 4: Sagittal T1, coronal STIR, axial T1 and axial STIR MRI and e, transverse ultrasound at same level as the MR images demonstrating a large lesion in the hamstring compartment of the thigh. The ultrasound shows the lesion to be cystic with some more solid internal elements. The MRI shows the lesion to contain haemorrhagic or proteinaceous fluid, as shown by the increased signal on both T1 and STIR. These features together suggest a large haemorrhagic collection, with concern for an underlying malignant lesion. Biopsies were non-diagnostic.
| Technique | Frequency of ND soft tissue biopsy |
|---|---|
| US (external) | 1(3) |
| CT | 3(10) |
| US | 10 (33) |
| Visual | 16 (53) |
| Total | 30 |
Table 3: Mode of ND soft tissue biopsy.
Discussion
This study suggests, in ND musculoskeletal biopsies, a benign diagnosis is more common for soft tissue lesions. Paucicellular lesions such as haematoma/ AVM and ganglia were more difficult to diagnose.
Previous studies have shown ND biopsies were more likely to represent benign diagnoses than malignant [4,6-9]. In one recent study of over 900 CT-guided musculoskeletal biopsies (bone and soft tissue), 67% of ND biopsies yielded a benign diagnosis [4], which is broadly similar to our rate of 77% for soft tissue lesions. Other authors have commented that benign lesions may be inherently difficult to distinguish, because concerns regarding sampling error must always be considered [8]. This, we feel, is linked to the confidence of the team in a benign diagnosis, and, on occasions, a repeat biopsy may be done to confirm a benign diagnosis.
Although several previous studies on musculoskeletal biopsies have compared diagnostic yields for different types of lesion [1,8,9,12-14] e.g. sclerotic versus lytic in bone lesions, and technical aspects such as failure to obtain adequate material or tissue damage [8] these features were not common in our results. In our study very few ND biopsies were attributable to sampling difficulties, with most demonstrating non-specific features. These may be linked to the underlying tissue diagnosis, and this is an area which has not been directly addressed in early studies [10,15-18].
However, more recent studies have assessed this key question [1,4, 7,10,12], and several interesting patterns are emerging. Authors have identified that lack of solid material from a biopsy is a problem [7], and makes definitive diagnosis from samples challenging. This has been demonstrated in our series with vascularised, cystic and myxoid lesions requiring multiple biopsies. Awareness of this is crucial for clinicians in this area to help reduce the risk of ND biopsies. One interesting series demonstrated biopsies from myxoid lesions were clinically useful in only 11% of cases, compared to those from non-myxoid lesions, which were useful in 80% of cases [11].
In our series over 50% of ND soft tissue biopsies were done visually using clinical examination, often in an outpatient setting. Previous authors have demonstrated significantly improved diagnostic accuracy for image-guided soft tissue tumour biopsies compared to those done using clinical landmarks (95% versus 78% respectively) [19]. It is known US guided biopsies can be invaluable in avoiding cystic or necrotic areas within soft tissue tumours, thereby increasing diagnostic accuracy image-guidance [20]. One recent meta-analysis of musculoskeletal biopsies even concluded accuracy was improved when biopsies were done by radiologists compared to surgeons [21].
Limitations
There are several limitations which should be considered when interpreting the results of our study. It is a retrospective, nonrandomised study from a specialist centre. We feel that given the low frequency of many of the conditions reviewed, a prospective randomised study would not have been feasible or practical. There is also a risk of selection bias in our case mix, being a regional bone and soft tissue tumour unit; which has been highlighted by other authors [6,9,12]. Furthermore, the biopsy technique and site may have varied slightly between cases, which may have impacted slightly on our ND biopsy rate.
Conclusion
Overall, this study shows that for ND musculoskeletal soft tissue biopsies a benign diagnosis is more common than malignant. Vascularised and myxoid lesions appeared most frequently, and haematomas/arteriovenous malformation were significantly more likely to need two biopsies.
Previous authors have suggested image-guidance for soft tissue biopsies to improve diagnostic accuracy and reduce complications [19,20] We strongly agree with this recommendation, and feel our data underlines the importance of this, in particular for soft tissue lesions with a significant myxoid or vascularised component.
References
- Rimondi E, Rossi G, Bartalena T, Ciminari R, Alberghini M, et al. (2011) Percutaneous CT-guided biopsy of the musculoskeletal system: Results of 2027 cases. Eur J Radiol 77: 31-42.
- Li Y, Du T, Luo TY, Yang HF, Yu JH, et al. (2014) Factors influencing diagnostic yield of CT-guided percutaneous core needle biopsy for bone lesions. Clin Radiol 69: e43-47.
- Bickels J, Jelinek J, Shmookler B et al. (2001) Biopsy of musculoskeletal tumors. Current concepts. Clin Orthop Relat Res 368: 212-9.
- Chang CY, Huang AJ, Bredella MA, Torriani M, Halperen EF, et al. (2015) Percutaneous CT-guided needle biopsies of musculoskeletal tumours; a 5-year analysis of non-diagnostic biopsies. Skeletal Radiol 44: 1795-1803.
- Issakov J, Flusser G, Kollender Y, Merimsky O, Lifschitz-Mercer B, et al. (2003) CT-guided needle biopsy for bone and soft tissue tumours. Isr Med Assoc J 5: 28-30.
- Hwang S, Lefkowitz RA, Landa J, Zheng J, Moskowitz, et al. (2011) Percutaneous CT-guided bone biopsy: Diagnosis of malignancy in lesions with initially indeterminate biopsy results and CT features associated with diagnostic or indeterminate results. AJR Am J Roentgenol 197: 1417-1425.
- Didolkar MM, Anderson ME, Hochman MG, Rissmiller JG, Goldsmith JD, et al. (2013) Image guided core needle biopsy of musculoskeletal lesions: Are non-diagnostic results clinically useful? Clin Orthop RelatRes 471: 3601-9.
- Omura MC, Motamedi K, UyBico S, Nelson SD, Seeger LL (2017) Revisiting CT-guided percutaneous core needle biopsy of musculoskeletal lesions: Contributors to biopsy success. AJR Am J Roentgenol 197: 457-461.
- Wu JS, McMahon CJ, Lozano-Calderon S, Kung JW (2017) Utility of repeat core needle biopsy of musculoskeletal lesions with initially non-diagnostic findings. AJR Am J Roentgenol 208:609-616.
- Yang J, Frassica FJ, Fayad L, Douglas PC, Kristy LW (2010) Analysis of non-diagnostic results after image-guided needle biopsies of musculoskeletal lesions. Clin Orthop Relat Res 468: 3103-3111.
- Ogilvie C, Torbert JT, Finstein JL, Edward JF, Richard DL (2006) Clinical utility of percutaneous biopsies of musculoskeletal tumors. Clin Orthop Relat Res 450: 95-100.
- Nouh MR, Shadt HM (2014) Initial CT-guided needle biopsy of extremity skeletal lesions: Diagnostic performance and experience of a tertiary musculoskeletal center. Eur J Radiol 83: 360-5.
- Jelinek JS, Murphey MD, Welker JA, Henshaw MJ, Barry Mk, et al. (2002) Diagnosis of primary bone tumours with image-guided percutaneous biopsy: experience with 110 tumors. Radiology 223: 731-7.
- Vieillard MH, Boutry N, Chastanet P, Duquesory B, Cotton A, et al. (2005) Contribution of percutaneous biopsy to the definite diagnosis in patients with suspected bone tumor. Joint Bone Spine 72: 53-60.
- Oetgen ME, Grosser DM, Friedlaender GE, Lindskog DM (2008) Core needle biopsies of musculoskeletal tumours: potential pitfalls. Orthopedics 31: 1-6.
- Rekhi B, Gorad BD, Kakade AC, Chinoy RF (2007) Scope of FNAC in the diagnosis of soft-tissue tumours: a study from a tertiary centre in India. Cytojournal 4: 20: 1-10.
- Puri A, Shingade VU, Agarwal MG, Anchan C, Juvekar S, et al. (2006) CT-guided percutaneous core needle biopsy in deep seated musculoskeletal lesions: a prospective study of 128 cases. Skeletal Radiol 35: 138-143.
- Mitsuyoshi G, Naito N, Kawai A et al. (2006) Accurate diagnosis of musculoskeletal lesions by core needle biopsy. J Surg Oncol 94: 21-7.
- Narvani AA, Tsiridis E, Saifuddin A, Briggs T, Cannon S (2009) Does image guidance improve accuracy of core needle biopsy in diagnosis of soft tissue tumours? Acta Orthop Belg 75: 239-244.
- Traina F, Errani C, Toscano A, Pungetti C, Fabbri D, et al. (2015) Current concepts in the biopsy of Musculoskeletal tumors. J Bone J Surg Am 97: e7.
- Kubo T, Furuta T, Johan MP, Sakuda T, Ochi M, et al. (2018) A meta-analysis supports core needle biopsy by radiologists for better histological diagnosis in soft tissue and bone sarcomas. Medicine 97: 29(e11567).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Morris R, Winn N, Singh J, Tyrrell P, Kaur S, et al. (2022) Image Guided Needle Biopsies for Musculoskeletal Soft Tissue Lesions: A 9-year analysis of Non- Diagnostic Biopsies. J Orthop Oncol 8: 168. DOI: 10.4172/2472-016X.1000168
Copyright: © 2022 Morris R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3006
- [From(publication date): 0-2022 - Dec 03, 2025]
- Breakdown by view type
- HTML page views: 2367
- PDF downloads: 639