Intraprosthetic Polyethylene Liner Dislocation of a Dual Mobility Mega-Prosthesis in an Osteosarcoma Patient: A Case Report and Literature Review
Received: 17-Feb-2020 / Accepted Date: 02-Mar-2020 / Published Date: 09-Mar-2020 DOI: 10.4172/2472-016X.1000131
Abstract
Osteosarcomas affecting the pelvic region often require extensive resections, resulting in the loss essential structures, which are required for hip joint stability. Dual mobility (tripolar) cup prostheses were created to address the issue of joint instability and have even become very popular for hip joint reconstruction following hemipelvectomies. Despite their increased stability, dislocations will still inevitably occur and need to be managed. In these cases, a closed reduction must be executed diligently as excessive levering may cause the “bottle opener” effect and dislocation of the polyethylene liner, an event also known as intraprosthetic dislocation. To our knowledge, this is the first reported case of an intraprosthetic dislocation by the “bottle opener” effect following an attempted closed reduction of a dual mobility system in an orthopedic oncology patient. In this case report and brief review of the current literature, we want to create awareness about the possible problems of dual mobility cups in oncology patients and suggest a type of management should these problems arise.
Keywords: Osteosarcomas; Intraprosthetic dislocation
Introduction
Primary malignant bone tumors affect the pelvic region in 10% to 15% of patients [1]. Currently, wide resection surgery is the standard of care for primary tumors [2]. Reaching a wide resection margin often entails sacrificing important structures such as the joint capsule, the abductor muscles, and the lesser trochanter with the insertion of the iliopsoas muscle [2-4]. The loss of such important structures often results in a loss of joint stability. In fact, it has been reported that the dislocation rate for oncological patients who have undergone hip reconstruction ranges from 10% to 40%, which is far greater than that of primary implants, attested between 2% and 8% [2].
Dual mobility (tripolar) cup prostheses are used in cases that are at high risk of joint instability and have even become the standard for the majority of the reconstructions in many centers [5]. Due to their intrinsic stability and lower dislocation rates, they are considered a good option for cancer patients, since dislocation can interfere with the beginning of medical therapy [2,5]. Biomechanically, these systems have a favorable head-neck ratio, which allows a greater range of motion while avoiding early femoral neck impingement with a fixed polyethylene (PE) liner or metal cup [6].
Despite their lower rates of dislocation, dual mobility cup systems present an additional and unique failure mechanism known as an intraprosthetic dislocation (IPD), in which the inner prosthetic femoral head disengages from the outer PE liner [7]. Late IPD (>24 months) is mainly related to the wear of the PE liner at the articulation of the femoral neck, also known as the “third joint” [8]. On the other hand, early IPD (<24 months), are caused during attempted closed reduction by the “bottle-opener” effect-engagement of the outer PE liner on the rim of the metal cup or pelvic bony prominences, with subsequent dissociation [9]. This mechanism is thought to be responsible for up to 79% of early IPD cases [7]. Once an IPD occurs, it is irreducible by any closed means and requires surgical management [7]. There have been many cases of IPD reported in primary total hip arthroplasty (THA) literature; however, very few (<2) have been reported in oncological orthopedic surgery [9].
In this case report, we present a patient with an IPD resulting from an attempted reduction, 12 months after undergoing a total right proximal femur and pelvic resection and reconstruction using the Modular Universal Tumour And Revision System (MUTARS®) and LUMiC® prostheses (implantcast, Buxtehude, Germany), in the treatment of a primary stage for osteosarcoma. We summarize the current literature about this complication to create awareness and suggest an appropriate method of management.
Case History
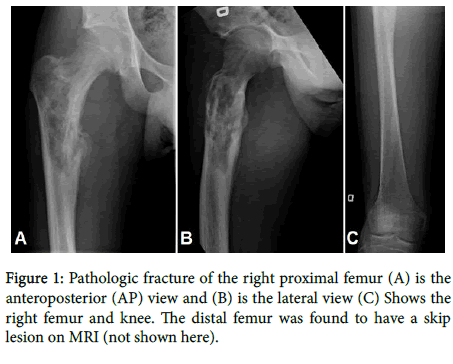
A 17-year-old Caucasian boy began having right hip pain and difficulty ambulating in the fall of 2017. The pain had been on and off but increasing in severity over the past three months. During that same timespan, the patient also reported having lost approximately 15 pounds and experienced intermittent fever, chills and night sweats. He first sought help from a physiotherapist, but after six physiotherapy treatments and worsening pain, he was referred for medical attention. A plain radiograph of the right hip ordered by an outside physician was done and showed a lytic lesion of the proximal femur. He was then referred to our academic hospital center where he presented with a pathologic fracture of the right proximal femur (Figure 1). A biopsy later revealed a primary osteosarcoma of the right proximal femur with periacetabular involvement.
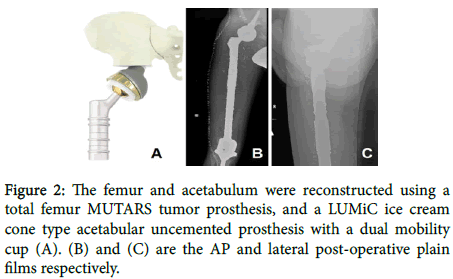
The patient underwent a wide en-bloc extra-articular resection and right total femur and acetabulum reconstruction. Unfortunately, the following muscles had tumor involvement and had to be resected: gluteus maximus, gluteus medius and minimus, psoas and the short external rotators. The right femur was reconstructed using a MUTARS tumor prosthesis, while the acetabulum required reconstruction using a LUMiC ice cream cone type acetabular uncemented prosthesis with a dual mobility cup (Figure 2). The final reduced construct proved to have good stability intraoperatively with only very mild instability at a point of maximal flexion, abduction and internal rotation. The right hip capsule was then reconstructed with a Trevira (polyethylene terephthalate) synthetic mesh to improve the stability and augment the soft tissue reconstruction. At this point in the surgery, the stability was satisfactory, especially with regards to pistoning, and there was no concern of dislocation. The previously sectioned muscles were attached to the new synthetic capsule, thereby providing additional stability and full muscular coverage of the implant. The patient’s recovery was uneventful and there were no immediate postoperative complications. He was discharged on postoperative day 7.
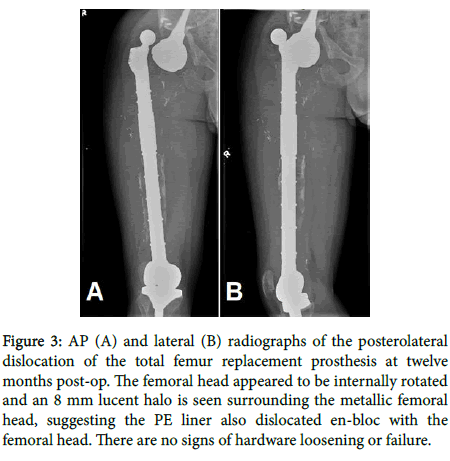
Twelve months later, the patient came to the Emergency Room (ER) with acute right hip pain and inability impossible to weight bear on the right leg. He reported a feeling of instability in the right hip. The pain occurred after the patient reported having done a squatting movement while attempting to kneel down at home. Objective physical findings included a significant leg length discrepancy (right leg 7 cm shorter), and a normal distal neurovascular exam. There were no prior episodes of dislocation or signs of infection.
X-rays were done and revealed a posterolateral dislocation of the femoral head (Figure 3). The LUMiC acetabular component remained well seated and in intact position, while the femoral head component appeared to be internally rotated. A subtle 8 mm rim of a lucent halo was seen surrounding the metallic femoral head, suggesting the interposed polyethylene (PE) liner had also dislocated en-bloc along with the femoral head of the implant. Distally, the total femur and the hinged knee arthroplasty appeared intact with no signs of hardware loosening or failure.
Figure 3: AP (A) and lateral (B) radiographs of the posterolateral dislocation of the total femur replacement prosthesis at twelve months post-op. The femoral head appeared to be internally rotated and an 8 mm lucent halo is seen surrounding the metallic femoral head, suggesting the PE liner also dislocated en-bloc with the femoral head. There are no signs of hardware loosening or failure.
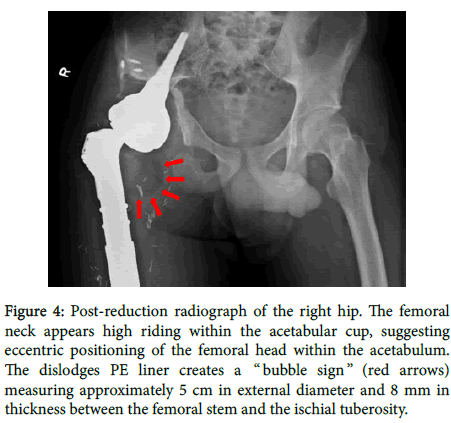
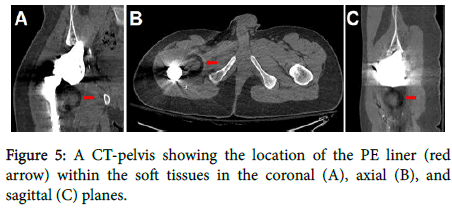
A closed reduction was attempted under conscious sedation. Postreduction radiographs showed that the femur replacing implant had been reduced into the acetabular portion, but the femoral neck appeared high riding within the acetabular cup, suggesting eccentric positioning of the femoral head within the acetabulum. Furthermore, a new semicircular lucency (“bubble sign”) measuring approximately 5 cm in external diameter and 8 mm in thickness were noted between the femoral stem and the ischial tuberosity (Figure 4). This was proved that the PE liner previously surrounding the metallic femoral head was medially dislodged during the attempted reduction. A CT-pelvis was obtained to confirm the location of the PE liner within the soft tissues (Figure 5) and the patient was booked for an open reduction with or without reconstruction.
Figure 4: Post-reduction radiograph of the right hip. The femoral neck appears high riding within the acetabular cup, suggesting eccentric positioning of the femoral head within the acetabulum. The dislodges PE liner creates a “ bubble sign ” (red arrows) measuring approximately 5 cm in external diameter and 8 mm in thickness between the femoral stem and the ischial tuberosity.
During the open procedure, a layer of black discoloration was noticed over the Trevira mesh and over the medial tissues, which was thought to be a possible metallosis reaction. The curettage and removal of all black debris and tissue were performed. The dislodged PE liner was then found in the medial soft tissues and taken out. Upon inspection, no significant damage was seen on the PE liner or the metallic prosthetic head. The MUTARS and LUMiC prostheses were inspected and found to be stable. The same PE liner was then reinserted and impacted over the prosthetic metallic femoral head. A trial reduction was attempted, and stability of the hip was confirmed with flexion of up to 90°, 10° of adduction, internal rotation of up to 45°, and external rotation of up to 45°. The synthetic Trevira capsule was then tightly closed.
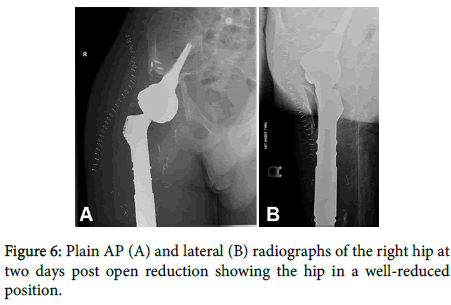
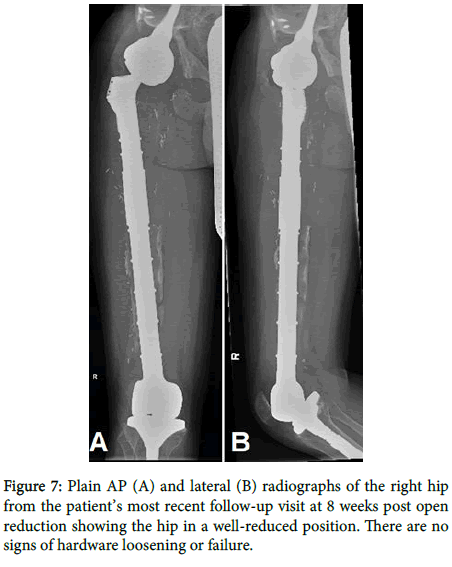
Two days post-surgery, his x-ray showed a hip in a well-reduced position (Figure 6). The patient was given strict limitations with regards to physiotherapy of no hip flexion >70°, no adduction passed midline and no internal or external rotation >30°. He was discharged on the second day post-operation after receiving clearance from the physiotherapy team. At the nine-month follow-up mark, the patient had not suffered any other episodes of dislocation, nor did his latest plain films show any sign of hardware loosening or failure (Figure 7).
Discussion
Wide excision of pelvic tumors is one of the most technically challenging procedures in orthopedic oncology. As instability is a common concern in pelvic resections, proper reconstruction requires the use of modern surgical techniques and orthopedic implant technology.
In 2017, Zoccali et al. proposed a classification of the indications for dual mobility cup reconstruction based on the anatomic structures involved in the oncological disease. As per their method of classification, our patient was a Type IV which is a strong indication for the use of a dual mobility cup as there is significant instability associated with a wide resection of the acetabulum and a higher risk of dislocation [2]. Furthermore, in an earlier 2011 study on 27 reconstructions with an ‘‘ice-cream cone prosthesis’’ similar to ours, it was noted that four dislocations (15%) which occurred were after Enneking Type 2 or 3 pelvic resections [10]. However, it is important to note that this group used bipolar cups rather than dual mobility cups (tripolar). Despite the difference, it is clear that just by virtue of the nature and location of the disease in our patient (Enneking Type 2), he was considered to be in a high-risk category for dislocation from the beginning.
The musculature impacted by the resection has also shown to influence the rates of dislocation. Fisher et al. attributed the higher risk of dislocation of Enneking Type 2 or 3 pelvic resections to the fact that virtually all muscles that attached the leg to the pelvis had been resected (only the glutei and psoas remained) [10]. In 2009, when analyzing the use of a dual mobility cup in preventing dislocation following tumor resection (primary and metastatic), Philippeau et al. found that dislocation risk depended primarily on the surgical management of the abductor system [9]. With a sample size of 71 patients, and an overall rate of dislocation of 9.8% (5.2% in bone metastasis and 15% in primary bone tumor), the rates of dislocation for specific subgroups were the following: 3.5% in the case of abductor conservation, 9.5% in the case of abductor sectioning/reinsertion, and 18% in case of gluteus medius muscle or nerve resection [9]. By comparison, during our patient’s first operation, the gluteus maximus, abductors, psoas, external rotators were all sectioned and reinserted, thereby putting him in the 9.5% chance of dislocation category. The massive extent of soft tissue resection, particularly the abductors, can profoundly impair muscular function and joint stability, thereby further adding to our patient’s risk of postoperative dislocation.
Our patient presented to the ER 12 months postoperatively with acute hip pain after having done a deep squatting movement. The initial plain films showed that the PE liner had dislocated en bloc along with the femoral head of the implant. After an attempted closed reduction under conscious sedation, the repeat X-rays showed the characteristic “bubble sign” described in the literature, suggestive of an intraprosthetic dislocations of the PE liner [11].
Due to the low amount of reported cases of IPD reported in oncological patients, no one has yet to offer a mechanism of IPD in this population. However, due to the similarities in dual mobility systems used THA, an inference can be drawn from the data available on this subject. In other words, the mechanism of IPD seen in our case is likely to be the one described by Loubignac and Boissier called the “ bottle opener ” effect, which occurs during an attempted closed reduction. A systematic review from 2016 on the early (<24 months) intraprosthetic dislocation in dual-mobility implants for THA, found that the “bottle opener” effect was responsible for 79% of IPD [7]. This is further supported by the fact that the dislodged PE liner in our patient was thoroughly examined and found to have no evidence of wear.
Overall, there have been few reported cases of dual mobility hip dislocation in oncology patients, and even fewer reported cases of IPD. In their 2009 study, Philippeau et al. reported seven cases (9.8%) of dislocation out of 71 dual mobility systems; two that were in the metastatic group (2/38 or 5%) and were treated with closed reduction under general anesthesia, and five that were in the primary tumor group (5/33 or 15%) and were all reduced surgically. There is no mention, however, whether there was an attempted closed reduction in the primary tumor group. Also, of those five cases, two had additional IPD which was associated with PE wear; one which occurred before 12 months and the other after 12 months [9]. In a 2017 multicenter review, Bus et al. reported a single case (1/24 or 4%) of dual mobility hip dislocation with a LUMiC prosthesis. However, there is no mention of the time postoperatively at which the dislocation occurred, the presence of IPD, or the method of reduction [5]. More recently in 2018, another group studying pelvic reconstructions following periacetabular bone tumour resections using a cementless ice-cream cone prosthesis with dual mobility cup, reported dislocations in four (17%) of 24 patients [1]. Of these four, one was in a patient with metastatic bone tumor and occurred late (55 months). The other three were in primary tumor patients, of which two occurred within the first month and one at 7 months. All were reduced by closed reduction, and therefore could not have had IPD. There is no mention of the type of anesthesia used to perform these closed reductions [1]. There are therefore a total of 12 cases of dual mobility hip dislocations reported in the orthopedic oncology literature, and only two of which had IPD. It is important to note that those two reported cases of IPD were due to PE liner wear (seen intraoperatively) rather than the “bottle opener” effect as seen in our case.
During the open reduction, the presence of a layer of black discoloration was noted over the Trevira mesh and over the medial tissues. This was thought to be a possible metallosis reaction. There are no reported cases of metallosis in oncology patients, but there have been several cases of IPD with metallosis in dual mobility systems in THA. In all of these cases, IPD occurred first (due to wear of the PE liner) thereby putting the femoral metal head in contact with the metal socket, resulting in subsequent metallosis [11-15]. Therefore, it is unlikely that the black discoloration seen in our patient was a true metallosis reaction. One way to confirm this would have been via histopathological analysis of the tissues [15], but no such samples were taken on the day of the open reduction.
The reason why our closed reduction failed is unclear. As previously stated, there are at least six reported incidents of successful closed reductions in dual mobility systems, two of which were performed under general anesthesia [1-16]. A possible explanation is that the use of conscious sedation may have resulted in insufficient muscle relaxation. A 2011 report on dual mobility dislocations in THA, states that conscious sedation, although most commonly used in the ER setting, may not provide satisfactory muscle relaxation [13]. Therefore, in the future, it may be warranted to consider performing a closed reduction under general or even neuraxial anesthesia. In fact, as the latter leads to lower extremity muscle paralysis, it has been proposed as a safer and more efficient anesthetic option for reduction of dual mobility dislocation and potentially reduces the risk of iatrogenic IPD [14]. Finally, it has also been suggested that the reduction maneuver may be best performed under fluoroscopic guidance, with gentle reduction maneuvers rather than forceful levering, thereby reducing the risk of “bottle opener” effect [15].
Conclusion
With this case report and short review of current literature, we want to create awareness about the possible problems of dual mobility cups in oncology patients. Given the increase in baseline risk of dislocation in hemipelvectomies with massive soft tissue resection, dual mobility cups seem to be an appropriate choice for joint reconstruction. However, dislocations will still inevitably occur and will need to be managed. Closed reduction must be executed diligently and under the appropriate conditions, as excessive force or levering may cause the “ bottle opener ” effect and subsequent intraprosthetic dislocation. Should the latter arise, the only option remaining is open reduction, which puts the patient at risk of additional operative complications and comorbidities and constitutes a greater cost to the healthcare system. This is why we firmly believe it is imperative to only attempt closed reduction with the use of appropriate anesthesia (general or neuraxial), fluoroscopic guidance, and extreme caution.
References
- Issa SP, Biau D, Babinet A, Dumaine V, Le Hanneur M, et al. (2018) Pelvic reconstructions following peri-acetabular bone tumour resections using a cementless ice-cream cone prosthesis with dual mobility cup. Int Orthop. 1-11.
- Zoccali C, Attala D, di Uccio AS, Rossi B, Scotto G, et al. (2017) The dual mobility cup in muscular skeletal oncology: Rationale and indications. Int Orthop. 41(3): 447-453.
- Guo W, Sun X, Ji T, Tang X (2012) Outcome of surgical treatment of pelvic osteosarcoma. J Surg Oncol. 106(4): 406-410.
- Wirbel RJ, Schulte M, Mutschler WE (2001) Surgical treatment of pelvic sarcomas: Oncologic and functional outcome. Clin Orthop Relat Res. 390: 190-205.
- Bus MP, Szafranski A, Sellevold S, Goryn T, Jutte, PC Bramer, et al. (2017) LUMiC® endoprosthetic reconstruction after periacetabular tumor resection: Short-term results. Clin Orthop Relat Res. 475(3): 686-695.
- Grazioli A, Ek ETH, Rüdiger HA (2012) Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop. 36(12): 2411-2418.
- De Martino I, D'Apolito R, Waddell BS, McLawhorn AS, Sculco PK, et al. (2017) Early intraprosthetic dislocation in dual-mobility implants: a systematic review. Arthroplasty today. 3(3): 197-202.
- Noyer D, Gilles G (2003) La troisième articulation des prothèses de hanche à double mobilité. Maîtrise Orthopédique. 121: 20-22.
- Philippeau JM, Durand JM, Carret JP, Leclercq S, Waast D, et al. (2010) Dual mobility design socket use in preventing total hip replacement dislocation following tumor resection. Orthop Traumatol Surg Res. 96(1): 2-8.
- Fisher NE, Patton JT, Grimer RJ, Porter D, Jeys L, et al. (2011) Ice-cream cone reconstruction of the pelvis: A new type of pelvic replacement: early results. J Bone Joint Surg. British volume 93(5): 684-688.
- Waddell BS, De Martino I, Sculco T, Sculco P (2016) Total hip arthroplasty dislocations are more complex than they appear: A case report of intraprosthetic dislocation of an anatomic dual-mobility implant after closed reduction. Ochsner Journal. 16(2): 185-190.
- Mohammed R, Cnudde P (2012) Severe metallosis owing to intraprosthetic dislocation in a failed dual-mobility cup primary total hip arthroplasty. J Arthroplasty. 27(3): 493-e1.
- Stigbrand H, Ullmark G (2011) Component dissociation after closed reduction of dual mobility sockets: A report of three cases. Hip International. 21(2): 263-266.
- Cvetanovich GL, Fillingham YA, Della Valle CJ, Sporer SM (2015) Intraprosthetic dislocation of dual-mobility bearings associated with closed reduction: a report of two cases. JBJS case connector. 5(1): e26.
- Koper M, Verdijk R, Bos K (2019) Asymptomatic intraprosthetic dual mobility cup dislocation with increased metal ion levels. Arthroplasty Today.
- Philippeau JM, Durand JM, Carret JP, Leclercq S, Waast D, et al. (2010) Dual mobility design socket use in preventing total hip replacement dislocation following tumor resection. Orthop Traumatol Surg Res. 96(1): 2-8.
Citation: Slawaska-Eng D, AlAqeel M, Farii HA, Boulila C, AlAseem A, et al. (2020) Intraprosthetic Polyethylene Liner Dislocation of a Dual Mobility Mega-Prosthesis in an Osteosarcoma Patient: A Case Report and Literature Review. J Orthop Oncol 6: 131. DOI: 10.4172/2472-016X.1000131
Copyright: © 2020 Al Farii H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6510
- [From(publication date): 0-2020 - Dec 18, 2025]
- Breakdown by view type
- HTML page views: 5577
- PDF downloads: 933