Misdiagnosis of Intestinal Tuberculosis as Crohn's Disease: A Case Report and Literature Review of Parametric Predictive Models
Abstract
In recent years, the incidence of Crohn's disease (CD) has been increasing worldwide, especially in areas where tuberculosis (TB) is prevalent. Due to similar manifestations, distinguishing between Crohn’s disease (CD) and intestinal tuberculosis (ITB) is quite challenging. Herein, we report the case of a 25 year old man who presented with recurrent partial bowrl obstruction, whose initial diagnostic work up suggested stenosing Crohn disease 3 years ago. He had been previously treated with mesalazine and corticosteroids. After undergoing surgical treatment, histopathological findings revealed the diagnoses of intestinal tuberculosis instead. We combined our case report with parametric predictive models reviewed in the literature to evaluate their diagnostic accuracy for our case. We found that using these models could lead to a better differentiation between these two entities.
Keywords: Crohn's Disease; Intestinal tuberculosis; Parametric predictive models
Background
Crohn’s disease (CD) and intestinal tuberculosis (ITB), although they have different etiology, pathogenesis, and therapeutic options, they can exhibit similar clinical, endoscopic, morphological, and histological manifestations [1-3]. Therefore, differentiating these two entities is challenging for the clinician and can sometimes lead to misdiagnosis [4,5]. Here, we report a case whereby a male patient was diagnosed with ITB presenting with recurrent partial bowel obstruction, whose initial diagnostic work up suggested CD. We compared our case with the results of the literature review using multiple multi parametric predictive models.
Patients and Methods
A 25 year old man was brought to the Emergency Room presenting with a 4 month history of recurrent partial bowel obstruction, accentuated during the last 24 hours associated with right lower abdominal quadrant pain.
The patient had been diagnosed 3 years ago with stenosing Crohn’s disease and had previously been treated with mesalazine and occasionally with corticosteroids during flare up. A surgery was proposed at that time due to short and symptomatic small intestine stenosis, but the patient refused and was lost to follow up. During the past 3 years, he hasn't received any treatment and reported recurrent partial bowel obstruction.
At the time of admission, the patient didn't complain of diarrhoea, fever or night sweats. The physical examination revealed tenderness at the right lower abdominal quadrant. The rest of examination was normal. Laboratory blood exams were in the normal range and QuantiFERON-TB test was positive.
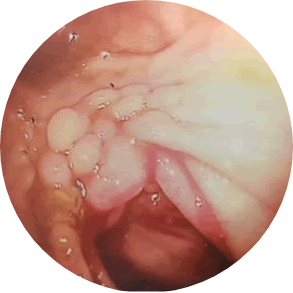
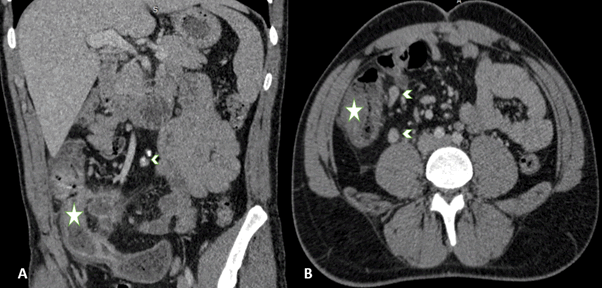
An abdominal CT scan was performed to exclude surgical emergency, displaying parietal circumferential thickening of the last small intestine loop and the cecum, extending over 76 mm. The chest X-ray was normal. The patient had undergone a colonoscopy showing ileal stenosis and a pseudopolypoid ileocaecal valve (Figure 1). The decision was to opt for surgical treatment and azathiopurine intake to prevent post-operative relapse. The patient underwent a 21 cm terminal ileum resection.
The histopathological findings of the surgical specimen revealed the presence of numerous granulomas with necrotizing and calcified lymph node involvement. This led to reconsideration of TB as a differential diagnosis.
The key to diagnosis was performing a polymerase chain reaction (PCR) to identify Mycobacterium tuberculosis (MT) which came positive.
Ultimately, the diagnosis of ITB was confirmed and the patient began tuberculosis RIPE therapy with significant response.
Discussion
The positive rate of specific methods for the diagnosis of TB and CD is low. In hesitant situations, the diagnosis cannot be definite. In recent studies, multivariable prediction models have been established to distinguish between CD and ITB [2]. We combined our case report with some parametric predictive models reviewed in the literature to evaluate their diagnostic accuracy in our case.
Meta-analytic bayesian model
We assessed and used a Bayesian model that produces estimates of the probability of ITB and CD that are calibrated to local prevalence [6]. The score was available online. The prevalence of TB in patients with small bowel ulceration is low in Tunisia, estimated at 0.05 which is similar to the US we don’t have baseline prevalence in Tunisia, Our patient had a probability of ITB estimated at 68.62%.
Model based upon endoscopic features
A predictive model based upon endoscopic features was reported [3]. They included eight features. Our patient had only two features consisting of involvement of less than 4 segments and the presence of pseudopolyps meaning a score of 2 suggestive of ITB.
Computerized tomography based score
A predictive model published recently features computerized tomography results of ITB and CD [7]. Our patient presented with ileo-caecal region involvement, one lymph node ≥ 1 cm and long segment involvement, meaning a score of 1, suggestive of ITB (Figure 2).
Korean model
Recently, proposed a model with good performance based on the results of a large retrospective cohort in seven centers in Korea, but the model has not been valid outside of Korea [8]. The optimal cutoff value for a predictive diagnosis was 0.350 in both models. Our patient had a score of 0.21 suggestive of CD. In our case, most of the predictive models and scores mentioned in our review were suggestive of ITB except for the 7 marker risk score.
Conclusion
There have been till date many studies aiming to reach an ultimate equation capable of differentiating between CD/ITB. In the last few years, we have seen some new parameters on this aspect, including the latest Bayesian meta-analysis model, a model based upon endoscopic features, a CT based score, and the Korean model. Using these models could lead to a better differentiation between these two diseases.
References
- Mosquera-Klinger G, Andrea Ucroz B (2018) Crohn’s disease vs. Intestinal tuberculosis: A challenging differential diagnosis. Rev Colo de Gastro.33:423-30.
- Kedia S, Das P, Madhusudhan KS, Dattagupta S, Sharma R, et al. (2019) Differentiating Crohn’s disease from intestinal tuberculosis. W J of Gastro.25:418-32.
- Lee YJ, Yang SK, Byeon JS, Myung SJ, Chang HS, et al. (2006) Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn’s disease. Endoscopy.38:592-7.
- Wei JP, Wu XY, Gao SY, Chen QY, Liu T, et al. (2016) Misdiagnosis and mistherapy of Crohn’s disease as intestinal tuberculosis case report and literature review. Medicine.95:e2436.
- Akbar HO (2009) Intestinal tuberculosis and Crohn’s disease: The dilemma of similarities and misdiagnosis. BMJ Case Rep.2009:1729.
- Limsrivilai J, Shreiner AB, Pongpaibul A, Laohapand C, Boonanuwat R, et al. (2017) Meta-Analytic Bayesian Model for Differentiating Intestinal Tuberculosis from Crohn’s Disease. A J Gastro.112:415-27.
- Kedia S, Sharma R, Nagi B, Mouli VP, Aananthakrishnan A, et al. ( 2015) Computerized tomography-based predictive model for differentiation of Crohn’s disease from intestinal tuberculosis. Indian J Gastro.34:135-43.
- Jung Y, Hwangbo Y, Yoon SM, Koo HS, Shin HD, et al. (2016) Predictive factors for differentiating between Crohn’s disease and intestinal tuberculosis in Koreans. Am J Gastroenterol. 111:1156-64.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2703
- [From(publication date): 0-2021 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 1957
- PDF downloads: 746