Neuralgic and Nociceptive Pain in the Knee as a Cause of the Treatment Failure after Cartilage Repair Surgery: Two Case Reports
Received: 11-Jun-2018 / Accepted Date: 18-Jun-2018 / Published Date: 25-Jun-2018 DOI: 10.4172/2167-0846.1000325
Abstract
Objective: Cartilage injuries are one of the most frequent causes of knee pain. Other causes such as meniscus tears, synovial plica, synovitis, partial and total ligament ruptures are rather easy to identify by standard diagnostic methods and diagnostic arthroscopy. In this study we are describing two other clinical states, which could be the cause of the knee pain and should be addressed before a decision for operative treatment of cartilage injury has been made by a surgeon. Materials and Methods: Two patients with isolated focal defects due to previous trauma to the knee were diagnosed both using magnetic resonance imaging preoperatively and intraoperatively during arthroscopy. These were operated arthroscopically with standard procedure for microfracture. Both patients had treatment failure without a sign of significant improvement after six and twelve months. Results: Second look arthroscopy was performed in both cases due to the treatment failure and close to normal cartilage was found in the patella in first case and both in trochlea and medial femoral condyle in other case. No other cause of pain could be identified both with second look arthroscopy and magnetic resonance imaging done 6-12 months postoperatively. The patients were diagnosed with neuralgic pain in one case, and nociceptive pain in other case. Conclusion: These states are rare, but have to be addressed by the surgeon before making the decision about the operative treatment. By doing so, one could avoid eventual treatment failure and exposition of the patient to an unnecessary risk of complications during the surgery.
Keywords: Cartilage; Pain; Extra-articular
Introduction
Cartilage injuries is one of the most frequent causes of knee pain [1,2]. Other causes such as meniscus tears, synovial plica, synovitis, partial and total ligament ruptures are rather easy to identify by standard diagnostic methods and diagnostic arthroscopy [3,4]. In this study we are describing two other clinical states, which could be the cause of the knee pain and should be addressed before a decision for operative treatment of cartilage injury has been made by a surgeon.
Case 1
41 year-old woman of good general health, working as an assistant nurse. The patient had a trauma/distortion to the knee in 2013. Arthroscopy was done within a short period of time after the trauma and no damage to the knee was diagnosed. Magnetic resonance imaging (MRI) was also done and showed contusion to the lateral femoral condyle. The patient has experienced clinical improvement, but 6 months after the pain was back without new trauma.
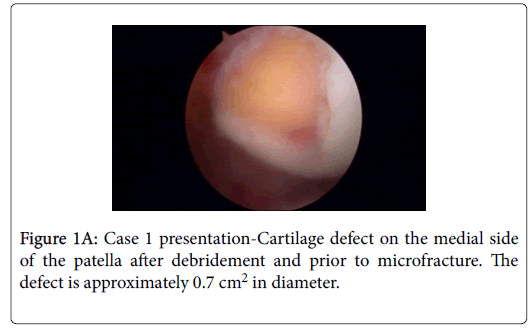
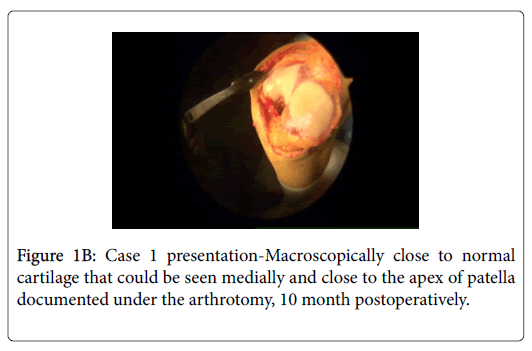
The patient experienced extension defect of 15 degrees, no defect with passive movement and consistent pain in the knee. 1 year after initial trauma she experienced swelling and pain, instability in the knee and limping gait. New arthroscopy was performed in April 2015 and a small rift was seen in the patellar cartilage, as well as a partial rupture of the ACL. Postoperatively, the patient has experienced pain, mechanical locking in the knee and has been sent to a physiotherapist. In January 2016 she has felt retropatellar pain, crepitation behind the kneecap, especially during stair walk and cycling. MRI in March 2016 showed a cartilage defect in the lateral facet of the patella when the authors of this article were presented with this case for the first time. A decision was made to do a new arthroscopy in June 2016 and a cartilage defect was identified most caudally and medially in the medial facet (not lateral as judged by the radiologist previously). The size of the defect was 0.7cm2-1cm2 (Figure 1A) and according to outer bridge classified as grade III-IV [5]. A micro fracture was performed arthroscopically [6], as well as lateral release by open technique, because of previous subluxations of the patella and laterally positioning of the kneecap, as judged by MRI preoperatively.
In April 2017, because of the lack of the improvement a new arthroscopy was performed, and patellar cartilage surface was judged as close to normal (Figure 1B). Because of inflamed synovia, as seen by arthroscopy, we have converted the operation to arthrotomy (Figure 1B) and performed partial synovectomy and suprapatellar bursa removal. However, the patient hasn`t experienced any improvement, she still had locking in the knee, hobbling with gait and constant pain. In September 2017 the patient was remitted to an anesthesiologist specialized in the therapy of pain at our hospital, and he noted constant pain, burning in the knee, hyperalgesia for the nail stick, pain over the kneecap with palpation and hypoesthesia for warm and cold stimuli. In summary, the condition was judged as a neuropathic component in patients pain sensation, she was diagnosed with Complex Regional Pain Syndrome (CRPS), TENS therapy and recommendation for medical therapy with Gabapentin was given [7].
Case 2
49 year-old woman, working as a machinist and of good general health, operated previously for goiter and at the present on substitution therapy with Levaxin. The patient was even operated for cartilage damage in right knee with good result. The patient had a distortion in the knee, this time on the left side in September 2015. She experienced pain and instability at the time of the injury, and a meniscal tear was suspected initially. The patient showed clinical improvement but unfortunately injured herself in the same way few months after. She felt locking in the knee, pain, had to do a special maneuver to unlock the knee. Painful palpation medially in the knee, Apley’s test was positive for medial meniscus tear.
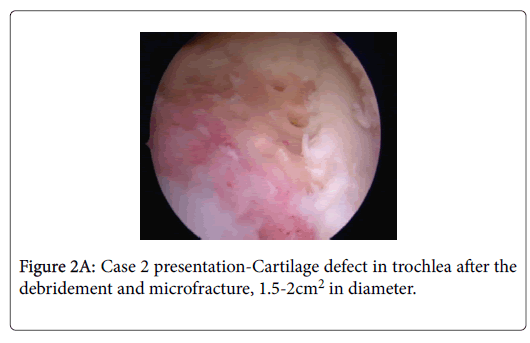
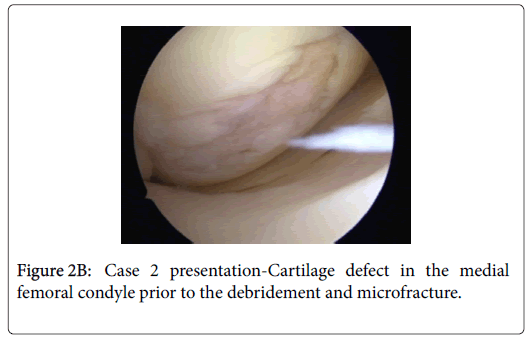
Diagnostic arthroscopy was performed in March 2016. Small cartilage damage in the patellar ridge was observed, chondral injuries in the trochlea and medial femoral condyle and a smaller radial rupture in the medial meniscus anterior horn, which was shaved during arthroscopy. The patient was operated again in November 2016 when the authors of this article were presented with the case for the first time. The finding on the patellar lateral facet was confirmed but not treated because the patient had experienced exclusively medial pain the knee, as well as because of the fact that the cartilage injury was classified according to Outer bridge as grade I-II. We have identified smaller cartilage damage in the lateral femoral condyle but it wasn’t treated for the same reason as the one mentioned above, it has been evaluated as asymptomatic [8]. We performed however micro fracture arthroscopically on cartilage injuries in trochlea (Figure 2A) and medial femoral condyle (Figure 2B), the first one was approximately 2cm2 in diameter and the other one 1 cm2.
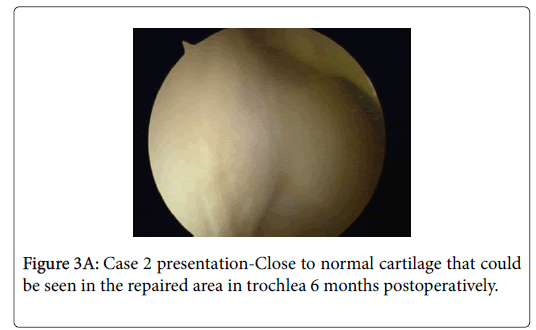
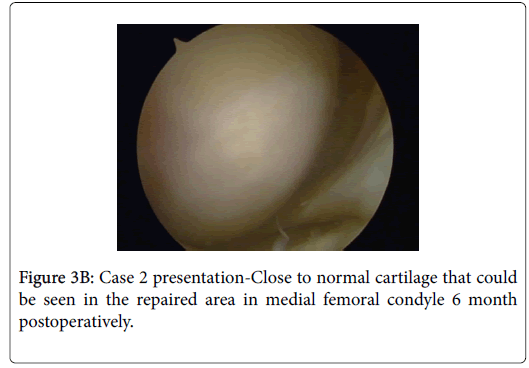
The patient didn’t experience any improvement after the surgery and a second look arthroscopy was scheduled for May 2017. Close to normal cartilage was found in both areas that were repaired (Figure 3A and 3B) and no new pathology in the knee was identified. Three months later the patient had an appointment at our open clinic and anserine bursa inflammation was suspected. She was treated with cortisone injection locally but unfortunately her condition remained unchanged.
The patient was remitted to our unit for the treatment of pain and examined by an anesthesiologist specialized in this area in October 2017. She still had a pain medially with gait, as well as locking phenomenon occasionally. With clinical investigation a broad muscular hyperalgesia was found by the anesthesiologist, in an area of approximately 12 × 12 cm2 around the knee medially, nociceptive pain was suspected, and pain located as extra-articular. Anserine bursa inflammation was proposed as a diagnosis by the anesthesiologist and the treatment was conducted in this direction. Unfortunately, the conservative treatment has failed, and the patient has been scheduled for the operation. The patient has been significantly improved after the pes anserine bursa removal.
Discussion
Cartilage injuries in the knee, and in general, is still a condition very difficult to treat [9-12]. The pain mechanism in isolated cartilage injuries is not well understood. The authors of this text couldn’t find a single article about this topic when searching on PubMed. What we have found is a certain number of articles dealing with pain mechanism in osteoarthritis (OA) [13]. Since articular cartilage is both aneural and avascular tissue it is incapable of directly generating pain or inflammation, some of the most important symptoms experienced by OA patients [14]. However, the structures like subchondral bone, periosteum, periarticular ligaments, synovium, joint capsule and conditions like periarticular muscle spasm may all be the sources of nociception in OA. The general consent is that cartilage injuries grade I-II according to Outer bridge shouldn’t been treated, in opposite to those of grade III-IV that should be repaired. The rationale for this decision is assumedly that grade I-II injuries are not usually associated with subchondral bone pathology and therefore probably asymptomatic. Our personal experience is however that this doesn’t need to be the case, since we have seen some at least grade II injuries in our practice that were symptomatic. In the same time, as described in our second case, a grade IV injury in the lateral femoral condyle has been left untreated since it was judged as asymptomatic.
The main issue of concern here could be again subchondral pathology, more precisely bone marrow lesions and sub-articular bone attrition, both have been related to knee pain [15-17] and even synovial activation and joint effusion related to that [18] MRI done preoperatively could be very useful diagnostic tool in terms of deciding whether the cartilage injury might be symptomatic or not and therefore repaired or remained untreated, since both types of subchondral pathologies named previously could be diagnosed with it. There are other bone-related causes of pain in OA that could be probably applied also to cartilage injuries such as: Periosteum inflammation, subchondral micro fractures and bone angina [19-21]. According to our personal clinical experience, meniscal tears, Hoffa’s fat pad impingement, synovial plica and OA all can mimic the pain that may be seen in the knee cartilage injuries. It is therefore necessary to address all these eventual pathologies before taking definitive care of cartilage defects. Decision from the surgeon to treat operatively cartilage defects should be very well balanced with the expected improvement, and the time for the surgery should be chosen carefully when all other causes of knee pain have been excluded or treated first, intraarticular but extra-articular as well. In our two cases, it seems that we have failed to set the right diagnosis from the beginning.
In our article, we have focused especially on extra-articular causes of knee pain that can mimic those seen in cartilage injuries. The authors of this text have an impression that these extra-articular causes of pain such as neuralgic and nociceptive pain could be easily missed during clinical evaluation. Indeed, there are reports postulating that as a consequence of the knee joint ligaments injury, the nerves which reinnervate the healing soft tissues contain an overabundance of analgesic chemicals such as substance P and calcitonin gene-related peptide [22,23]. One can speculate that injured joints may develop neuropathic pain post-traumatically [24]. Another interesting observation is that during the inflammation/trauma, the receptive field of joint receptors can expand into adjacent areas such that mechanical stimuli in non-articular tissues such as the surrounding muscle can suddenly become activated. Otherwise, joint nociceptors are typically localized within specific articular structures and their receptive field is normally restricted to the joint. That would mean for example that a typical neuron in the spinal cord with a receptive field in the joint may respond to physical stimuli of extra-articular muscle [25,26]. We would like to stress at this moment that both of our patients had a trauma to the joint before they have become symptomatic. According to Hunter et al. tissue injury activates the nociceptive system, which generates the subjective pain experience.
One should be also aware that certain patients have a combination of several pathologies that can complicate even more our judgment and final decision about the treatment. That’s why we should be very careful in not exposing the patients to an unnecessary risk of operation until we haven’t excluded all possible causes of pain, extra-articular are easy to be missed as we have seen here. This is also important when it comes to the evaluation of the results after cartilage repair surgery. We can namely see in our work that even though we got very good cartilage repair the treatment has failed. That is why we can speculate that at least a part of the treatment failures in large clinical studies could be related to other causes such as neuralgic and nociceptive pain, i.e. extra-articular causes of the treatment failures. The treatment failure in our first case could be also due to the possibility that the right diagnosis was not made initially and that several operations could have induced the final state of CRPS, despite the pain specialist judgment about the cause and the time of CRPS development. Unfortunately, there are no studies done or reports written on this topic, which is also the main reason why we have decided to point out to this problem in our article.
In summary, a certain number of articles could be found addressing this issue in knee OA but not cartilage injuries and its repair. These conditions are not many, but a surgeon must keep them in mind when making his clinical evaluation of the causes of pain and making the final decision to continue with operative treatment. The same caution should be taken when evaluating the results after cartilage repair. By doing that, a certain number of results misinterpretation could be avoided after cartilage repair surgery failures and some patients wouldn’t be exposed to the unnecessary risk of operation, when the cause of pain is other than cartilage injury.
Funding Acknowledgement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interest in preparing this article.
References
- Erickson BJ, Campbell K, Cvetanovich GL, Harris JD, Bach BR Jr, et al. (2016) Nonligamentous soft tissue pathology about the knee: A review. Orthopedics 39: 32-42.
- Asano H, Muneta T, Shinomiya K (2002) Evaluation of clinical factors affecting knee pain after anterior cruciate ligament reconstruction. J Knee Surg 15: 23-28.
- Simecek K, Latal P, Duda J, Simecek M (2017) Comparison of the arthroscopic finding in the knee joint and the MRI- Retrospective study. Acta Chir Orthop Traumatol Cech 84: 285-291.
- Bin Abd Razak HR, Sayampanathan AA, Koh TH, Tan HC (2015) Diagnosis of ligamentous and meniscal pathologies in patients with anterior cruciate ligament injury: Comparison of magnetic resonance imaging and arthroscopic findings. Ann Transl Med 3: 243.
- Lasmar NP, Lasmar RC, Vieira RB, de Oliveira JR, Scarpa AC (2015) Assessment of the reproducibility of the outer bridge and FSA classifications for chondral lesions of the knee. Rev Bras Ortop 46: 266-269.
- Erggelet C, Vavken P (2016) Microfracture for the treatment of cartilage defects in the knee joint- A golden standard? J Clin Orthop Trauma 7: 145-152.
- Carroll I, Curtin CM (2013) Management of chronic pain following nerve injuries/CRPS type II. Hand Clin 29: 401-408.
- Versier G, Dubrana F (2011) Treatment of knee cartilage defect in 2010. Orthop Traumatol Surg Res 97: S140-S153.
- Johnson CC, Johnson DJ, Garcia GH, Wang D, Pais M, et al. (2017) High short-term failure rate associated with decellularized osteochondral allograft for treatment of knee cartilage lesions. Arthroscopy 33: 2219-2227.
- Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T (2009) Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med 37: 902-908.
- Ogura T, Mosier BA, Bryant T, Minas T (2017) A 20-Year follow-up after first-generation autologous chondrocyte implantation. Am J Sports Med 45: 2751-2761.
- Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Ludvigsen TC, et al. (2016) A randomized multicenter trial comparing autologous chondrocyte implantation with microfracture: Long-Term follow-up at 14 to 15 years. J Bone Joint Surg Am 98: 1332-1339.
- Hunter DJ, McDougall JJ, Keefe FJ (2008) The symptoms of OA and the genesis of pain. Rheum Dis Clin North Am 34: 623-643.
- Felson D (2005) The sources of pain in knee osteoarthritis. Curr opin Rheumatol 17: 624-628.
- Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, et al. (2001) The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 134: 541-549.
- Hunter D, Gale D, Grainger G, Lo G, Conaghan P (2008) The reliability of a new scoring system for knee osteoarthritis MRI and the validity of bone marrow lesion assessment: BLOKS (Boston Leeds Osteoarthritis Knee Score). Ann rheum dis 67: 206-211.
- Torres L, Dunlop DD, Peterfy C, Guermazi A, Prasad P, et al. (2006) The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage 14: 1033-1040.
- Lo G, McAlindon T, Niu J, Zhang Y, Beals C, et al. (2008) Strong association of bone marrow lesions and effusion with pain in osteoarthritis. Arthritis Rheumatism 56: S790.
- Cicuttini FM, Baker J, Hart DJ, Spector TD (1996) Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthritis Cartilage 4: 143-147.
- Burr DB (2004) The importance of subchondral bone in the progression of osteoarthritis. J Rheumatol Supp 70: 77-80.
- Simkin P (2004) Bone pain and pressure in osteoarthritic joints. Novartis Found Symp 260: 179-186.
- McDougall JJ, Bray RC, Sharkey KA (1997) Morphological and immunohistochemical examination of nerves in normal and injured collateral ligaments of rat, rabbit, and human knee joints. Anatomical Record 248: 29-39.
- McDougall JJ, Yeung G, Leonard CA, Bray RC (2000) A role for calcitonin gene-related peptide in rabbit knee joint ligament healing. Can J Physiol Pharmacol 78: 535-540.
- Hanesch U, Pawlak M, McDougall JJ, Hanesch U, Pawlak M, et al. (2003) Gabapentin reduces the mechanosensitivity of fine afferent nerve fibres in normal and inflamed rat knee joints. Pain 104: 363-366.
- Schaible H, Schmelz M, Tegeder I (2006) Pathophysiology and treatment of pain in joint disease. Adv Drug Deliv Rev 58: 323-342.
- Konttinen YT, Kemppinen P, Segerberg M, Hukkanen M, Rees R, et al. (1994) Peripheral and spinal neural mechanisms in arthritis, with particular reference to treatment of inflammation and pain. Arthritis & Rheumatism 37: 965-982.
Citation: Andjelkov N, Riyadh H, Wretenberg P (2018) Neuralgic and Nociceptive Pain in the Knee as a Cause of the Treatment Failure after Cartilage Repair Surgery: Two Case Reports. J Pain Relief 7: 325. DOI: 10.4172/2167-0846.1000325
Copyright: © 2018 Andjelkov N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6659
- [From(publication date): 0-2018 - Oct 16, 2025]
- Breakdown by view type
- HTML page views: 5816
- PDF downloads: 843