Nurse Practitioner Confidence and Attitudes towards Brief Motivational Interventions to Improve Compliance with Health and Wellness Recommendations
Received: 09-Feb-2018 / Accepted Date: 21-Feb-2018 / Published Date: 28-Feb-2018 DOI: 10.4172/2471-9846.1000212
Abstract
Background: Health behavior risks prevail in older patients and can include unhealthy diet and nutrition, sedentary lifestyle and physical inactivity, alcohol use and abuse and poor oral hygiene. According to the Centers for Disease Control (CDC), most of the sickness, dependency, disability, use of resources, institutionalization and premature morbidity and mortality associated with chronic disease can be avoided through preventive measures and risk reduction. Preventive care is more effective in improving health than routine health care, yet research indicates that many patients do not seem to receive preventive strategies due to provider barriers. Evidence supports that training and education significantly improve practitioner knowledge, their decision to use strategies for behavior change and increases confidence.
The emerging body of evidence supports brief motivational interventions as effective strategies that can help patients change health behaviors and affect outcomes. The purpose of this study was to assess nurse practitioner student confidence and attitudes in using a brief motivational intervention. A secondary aim was to assess the degree of completion of each patient’s selected behavioral plan.
Methods: This investigator-initiated pilot study examined relationships among 15 nurse practitioner student confidence and attitudes toward delivery and implementation of a Brief Action Planning (BAP) intervention to 104 older adults. Nurse practitioner students received a BAP educational program and delivered BAP to older adults in an inter-professional collaborative practice that addresses the oral health, health promotion, clinical prevention and social services needs of community-dwelling older adults.
Results: Findings showed a significant change (p<0.05) in NP effectiveness, confidence, belief in and the ease of learning and incorporating BAP and the value of adding BAP to care. Forty two percent of patients fully completed, 35% partially completed and 23% did not complete their selected plan to change a health behavior.
Conclusion: An educational program increased NP confidence, effectiveness and belief in value and use of a brief motivational technique to change a health behavior. Provider training helps decrease barriers to implementing motivational techniques and prevention strategies. BAP shifts thinking about how to help motivate patients toward change, is easy to learn and feasible.
Keywords: Health behavior risk; Health behavior; Behavior change; Brief motivational interventions; Brief action planning; Motivational interviewing; Older adult
Introduction
Community based, brief motivational interventions presents an innovative approach for vulnerable older adult communities where prevention of healthcare risks is critical. Health behavior risks among older adults can include unhealthy diet and nutrition [1-5], sedentary lifestyle and physical inactivity [1,6-9], alcohol use and abuse [6,10,11] and poor oral hygiene [1,12]. These risks can compromise patient outcomes increasing the likelihood of developing or worsening chronic disease [2-4,7,8,13]. At least 75% of health care dollars are expended on chronic disease [14,15]. According to the Centers for Disease Control (CDC), most of the sickness, dependency, disability, use of resources, institutionalization and premature morbidity and mortality associated with chronic disease can be avoided through preventive measures [16]. Significant correlations have been noted between strategies that promote health behavior change and improvements in chronic disease prevention and self-management [17-21]. Various individual-level factors have been identified as determinants of health behavior change including knowledge; skills [22,23]; perceived: barriers; benefits; self-efficacy; health status; locus of control; and, interpersonal and situational influences [24-26]. Health behavior risk factors pose a significant problem to the elderly patient, especially those that are community dwelling.Efforts that promote health behavior change have the potential to improve outcomes. Brief motivational techniques have demonstrated efficacy in several conditions. The extent to which nurse practitioners engage in an are confident in brief motivational interventions is not known nor how confidence and attitudes towards BAP influence patient uptake of this intervention.
The extent to which NP’s engagement and confidence in brief motivational interventions is not known nor how confidence and attitudes toward BAP influences patient uptake of this intervention.
Langer et al. [27] reported that patients with COPD found motivational interventions very empowering and described them as having “enduring motivational benefits” in helping patients engage in self-management. In busy clinical practices, brief interventions can be effective “in less than 10 min” for encouraging women to exercise which exceeded those of traditional methods [28]. Dermen et al. [12] reported improvements in patient dental care and indicated that delivery is feasible by providers and implementation may encourage improved dental maintenance. In fact, addressing one health risk behavior may prompt other positive health behaviors [3]. Motivational coaching programs for behavior change are feasible and acceptable in a variety of healthcare settings [29].
An essential role of nurse practitioners is utilizing effective approaches to help individuals modify health behaviors. However, many nurses report minimal effectiveness and expertise in their ability to prevent and treat health risk behaviors. Preventive care is more effective in improving health than routine health care, yet research indicates that many patients do not seem to receive preventive strategies due to provider barriers [16,30]. Previously established approaches for motivating patients relied on advice, encouragement, education and persuasion, but these methods may not be effective as many patients do not heed recommendations or are not motivated to change [15,31,32]. Among older adults, education is less effective than counseling and counseling interventions are not generally employed [33,34]. This can result in frustration for professionals and patients alike.
Barriers To Implementation Of Brief Motivational Techniques
Several barriers interfere with provider, which includes NP’s, implementation of prevention and risk reduction strategies. Practitioners do not generally engage in prevention and risk reduction and they cite that barriers such as provider lack of time [11,35-40], inadequate and /or ineffective training and education [11,36-41], viewing patients as being opposed to change or resistant [35,37,38], lack of a sense of effectiveness [37,38,40,42]. lack of confidence [40], the impact on provider-patient relationships/relationship anxiety [11,37,40] and provider discomfort, avoidance and frustration [38], contributed to decreased use of motivational interventions. Katz (2016), found that nurses reported resistance from patients, inadequate time, lack of knowledge, perceived lack of skill in their effectiveness in behavioral counseling, skepticism regarding the effectiveness of counseling interventions and that lack of understand ing of the most effective intervention determined whether or not they provided behavioral change counseling. Some nurses expressed a sense of futility with regard to behavioral counseling [38].
Behavioral strategies may not be employed because providers are more comfortable with their role as educators [35]. But education and persuasion have not been very effective. In fact, communicating in a controlling way elicits opposition and evasion and is ineffectual, whereas the patient-centered approach elicits a positive reaction [40]. BAP discourages providers from giving advice or being confrontational with patients. In this way, BAP can be more effective in that it is less likely to create resistance and anger.
Training and education
Providers can benefit from education and training in the use of brief motivational techniques. Evidence supports that with training, there were significant improvements in practitioner knowledge, their decision to use strategies for behavior change and increased confidence [38,42,43]. A Web-based e-learning program for brief motivational techniques demonstrated that training was rated as highly acceptable, feasible and knowledge, skills and use in practice increased [36,44]. Nurses’ perception of power, or their ability to help change patient health outcomes, is directed by their values and knowledge and is an important part of clinical practice [45]. Approaches to increase nurses’ perception of power and confidence may contribute to changes in patient health status.
It is important to understand the influence of nurses’ confidence and attitudes in the implementation of a behavioral intervention, but to our knowledge, there are no studies assessing the relationship of provider factors to the delivery of this brief technique. There is a gap regarding the influence of provider confidence and attitudes on patient behavior change.
Motivational interviewing
Motivational Interviewing (MI), a client-centered counseling method, elicits and strengthens patient motivation to develop plans for positive behavior change [23,30,46]. Developed by Miller and Rollnick in 1983, MI helped alcoholics change their behavior [47] and has been studied for prevention and management of other diseases [17,23,32] and among older adults [32,48,49].
MI is not just a specific motivational technique but a counseling style and formal training and practice is essential for proficiency in the method, which can be very time consuming [30,50]. Delivery of MI may be time consuming as well, in fact, a systemic review showed that MI may take an extended period to deliver, sometimes 90-104 min per session [50].
Brief action planning
Brief adaptations of MI, founded on motivational techniques, have been developed. One specific brief motivational technique is Brief Action Planning (BAP) [22,50]. BAP, based on the foundation and spirit of MI, is a structured, patient self-management support tool providing the basis for behavioral change techniques within Comprehensive Motivational Interventions [5,51].
This evidence-based step-by-step approach facilitates goal-setting and behavioral action planning [52]. Developed by Cole in 2002, it integrates principles from MI regarding self-management, behavior change, action planning theory, psychology and self-efficacy [15]. The spirit of MI is collaboration, acceptance, evocation and compassion. Demonstrating the spirit of MI through patient-provider partnership is an essential component of BAP [15].
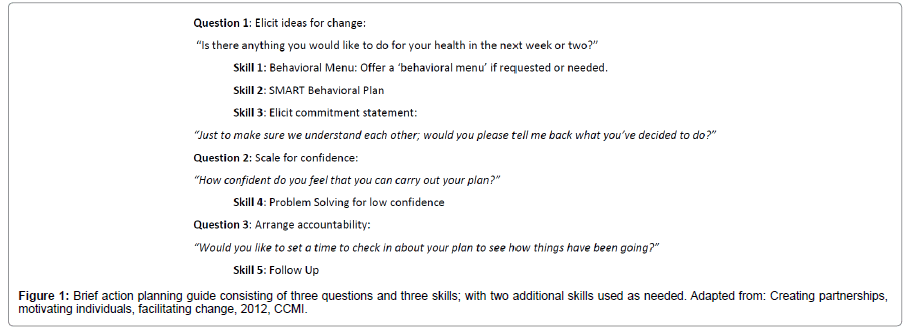
BAP includes three questions and three skills that are used during every BAP interaction and easily used in practice settings [52] (Figure 1). The overarching goal of BAP is to help the individual make a plan for health behavior change that they feel confident they can achieve [52]. The challenge for providers is to take time to learn the brief process and practice the strategies to help patients change unhealthy behaviors. BAP has the potential to impact many barriers and integrate evidence-based behavioral strategies into practice. Practitioners who wish to deliver BAP are encouraged to engage in on-line training at CMI http://www. comprehensivemi.com/about/brief-action-planning.
The purpose of this study is to determine relationships among nurse practitioner (NP) student confidence and attitudes towards delivering a BAP intervention to community-dwelling older adults presenting to an outpatient health and wellness center. A secondary aim is to assess the degree of completion of each patient’s selected behavioral plan.
Results from this study may have the potential to increase compliance of patients as a result of the increased confidence and attitudes of the nurses who have practiced BAP. And, because of the increase in confidence and attitudes, the patient may be more likely to complete a plan to change health behavior.
Methods
This pilot study examined relationships among nurse practitioner student confidence and attitudes toward delivery and implementation of a BAP intervention. The study was reviewed and approved by the institutional review board (IRB).
A BAP intervention was incorporated into the standard of care and implemented in a suburban health and wellness screening clinic of a large medical center with community-dwelling older adults identified as having modifiable health behaviors. Prior to the roll out of the BAP intervention, a comprehensive education program focusing on health behavior theory, the use of motivational techniques to change health behavior and protocol for the use of BAP was required of all NP students and faculty.
Setting
The study took place at an academic collaborative educational Senior Health and Wellness Center. This is an inter-professional collaborative practice that addresses oral health, health promotion, clinical prevention and social services needs of older adults.
Participants
The participants included a convenience sample of 15 Adult-Geriatric Nurse Practitioner (AGNP) students clinically training in the health and wellness center. Students were asked to volunteer for the research component of the study, which examined their confidence and attitudes toward delivering a BAP intervention to older adults. They completed an informed consent and the research component was explained.
Every older adult presenting to the health and wellness center was asked to participate in the study. The 104 participants were 60 years and older, English-speaking and mentally alert.
Intervention
In 2016-2017, after approval by the IRB, 15 NP students and 104 patients were recruited into the study over 28 weeks. The main identified modifiable health behaviors from the screening included exercise, dietary change, smoking and primary care provider and dental follow-up.
A comprehensive education program, preparing nurse practitioner students to deliver the new BAP protocol, was conducted. The baseline survey, A Survey of Confidence and Attitudes, a seven-item evaluative tool developed for this study, was administered to all NP students before the education program (Timepoint 1), immediately after the education program (Timepoint 2) and at the end of the students’ seven-week clinical rotation/practice (Timepoint 3). Role play and practice was done during the educational program and mid-semester to encourage and help ensure appropriate delivery of BAP.
Patients scheduled for their initial visit to the health and wellness center were screened, their health risks determined, and they were given a list of behaviors identified as contributing to overall health. As part of the routine visit social determinants of health and comorbidities, including hypertension, dyslipidemia, arthritis and diabetes, were assessed and identified. For this study, patients selected risk factors and developed a behavioral plan to help them initiate change as directed in the BAP protocol which was administered by the AGNP students. For the BAP intervention, all patients were asked “Is there anything you would like to do for your health in the next week or two?” The nurses then encouraged the patient to come up with a very specific plan of their own to change a health behavior. Patients were asked to measure their confidence that they will be able to carry out their plan, on a scale of 0 to 10. Then the patient might create a SMART plan to change a behavior. A SMART plan is specific, measurable, achievable, relevant and time-based. All patients received a two-week follow-up phone call to assess the degree of completion of their selected behavioral plan. Visit http://www.comprehensivemi.com/about/brief-action-planning for a comprehensive explanation of the BAP protocol.
Outcome measures
Data were collected on NP confidence and attitudes that may influence a patient’s propensity to make a plan to change a behavior. Confidence in ability was measured using two items, “How confident are you in your ability to help patients change a health behavior?” and “How confident are you in your ability to implement BAP with patients at the health and wellness center?” This item had a 10-point Likert-type response, from not at all confident, to extremely confident. Attitudes were measured using two items, “How easy do you think it is to learn BAP?” and “How easy do you think it will be to incorporate BAP into patient visits at the health and wellness center?” This also had a 10-point Likert response, from not at all easy to extremely easy. NPs’ health beliefs were assessed using three measures, “How valuable is helping patients change a health behavior to their overall health?” “How valuable do you think BAP will be to the plan of care for patients at the health and wellness center?” and “How effective have you been in your ability to help patients change a health behavior?” This 10-point Likert response ranged from not at all valuable/effective to extremely valuable/effective.
Data analysis
Outcomes were analyzed to evaluate if NP confidence and attitudes changed after Timepoints 1, 2 and 3. Due to limited sample sizes, Friedman’s ANOVA and Wilcoxon Signed Rank Test explored the trend in changes.
Results
AGNP confidence and attitudes with BAP
Table 1 lists the means and SD of the survey questions. Friedman’s Rank ANOVA tested the overall difference among the three-time points and indicated that changes were significant at p<0.05 regarding NP effectiveness in helping patients change a behavior, NP confidence in helping patients change a health behavior and implementing BAP, NP belief in the ease of learning and incorporating BAP and NP belief in the value of adding BAP to the plan of care.
| Survey Questions (n=15) | Timepoint 1 | Timepoint 2 | Timepoint 3 | p-value | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | - | |
| Valuable helping pts change | 9.53 | 0.743 | 9.87 | 0.352 | 10 | 0 | - |
| Effective helping pts change | 6.4 | 1.502 | 7.2 | 1.935 | 8.45 | 0.82 | 0.014 |
| Confident helping pts change | 7.07 | 1.751 | 8.2 | 1.474 | 8.55 | 0.934 | 0.009 |
| Confident implementing BAP | 5.67 | 2.582 | 8.47 | 0.99 | 8.45 | 1.214 | 0.002 |
| Easy to learn BAP | 6.4 | 2.354 | 8.53 | 1.685 | 8.91 | 1.3 | 0.002 |
| Easy to incorporate BAP | 6.13 | 2.264 | 8.4 | 1.549 | 7.91 | 2.166 | 0.002 |
| Valuable adding BAP | 8.67 | 1.543 | 9.67 | 0.724 | 7.82 | 2.136 | 0.009 |
| Confident implementing after graduation | - | - | - | - | 8.73 | 1.104 | - |
| Likely to use in practice | - | - | - | - | 8.64 | 0.924 | - |
| Items and ratings of participants on a 10-point Likert scale. Category 1=not at all to Category 10=extremely Significant at p<0.05 level based on Friedman’s ANOVA |
|||||||
Table 1: A survey of NP confidence and attitudes.
Completion of BAP
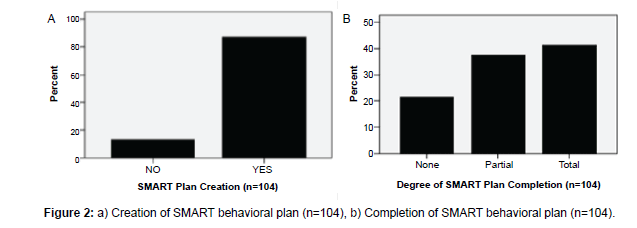
The two-week follow-up period indicated the degree of completion of a newly developed behavioral plan. Figure 2 shows 82% of patients created a SMART behavioral plan during their visit, 42% totally completed their plan (i.e., 50% complete or more), 35% partially completed their plan (up to 50% complete) and 23% did not complete or did very little of their plan.
Discussion
This small study concludes that, when patients are approached with a brief motivational intervention in the spirit of MI (collaboration, evocation, acceptance and compassion), they create a plan to change a health behavior. The literature supports that motivational techniques are emerging as effective strategies to promote behavior change, resulting in positive health outcomes [3,12,27,29]. By encouraging self-efficacy, patients become empowered to self-manage risk factors of chronic illnesses [15,52,53].
Previous studies indicate providers cite that barriers including inadequate and/or ineffective training and education, lack of a sense of effectiveness, lack of confidence and frustration affected their implementation of behavioral strategies [11,35-41]. The literature also indicates that training and education can empower providers, alleviate anxiety and can lead to use of motivational techniques [35,38,42,44-46].
We found that, after the NP education, participation in role playing and practice, there were significant changes in their confidence and belief in the value of the technique. Therefore, training and education are important.
The feasibility, practicability and value of Brief Action Planning was assessed via NP questionnaires. There were changes in NP’s sense of effectiveness and confidence. In clinical practice, provider confidence and power are related to participation and involvement in patients’ health outcomes [46].
Motivating and assisting patients to change their unfavorable health behavior is a major challenge for health professionals [29]. Strategies to increase providers’ involvement in change includes education and training, which can contribute to their perception of confidence, empowerment and efficacy. Results of this study show that BAP was a successful method for delivering evidence-based behavioral strategies to help patients change a health behavior in a general medical setting.
Limitations
There were several limitations to this study, including the small number of NPs, which may have led to sampling bias. The sample of older adults was a cross-section of those presenting to a health and wellness center in a socially homogenous area. There may have been overrepresentation of higher-functioning older adults because the study examined only those who are independent and presenting to a community health setting. Therefore, the results have limited generalizability. Selection bias might result in a low external validity of the study.
Although the NP sample size was small, limited to 15, the Friedman test and Wilcoxon signed ranks tests were utilized in analyses to strengthen the interpretation of the findings.
Completion of plan outcomes was based on self-reports rather than clinical outcomes. This may be subject to social desirability bias. A randomized controlled trial to measure clinical effects of the intervention would give more accurate results.
Conclusion
Although the sample was small, the results allude to the practicality of a theoretical, evidence-based client-centered behavioral intervention. In addition, the study showed the effectiveness of the comprehensive training of the practitioners delivering the intervention.
Anecdotal responses from the nurse practitioner participants support that they found this intervention useful, they will incorporate it into their practice and it offered them a way to assist patients toward behavior change.
BAP is cost-effective [15] and we also found it to be highly feasible in a busy health and wellness center. Delivery takes several min and patients can come up with a plan to change in 3 to 5 min. Adding it to a 20-minute office visit by utilizing other healthcare members to assist, is practical and can be easily incorporated into busy clinical offices [15]. BAP may have potential as an application across different disciplines and may be delivered in different medical settings.
This study may have contributed to initial steps in behavior change. Compliance with the intervention was high and we were encouraged by the patients’ high degree of self-reporting. BAP appeared to be wellaccepted by the patients and NP students.
The emerging body of evidence supports the effectiveness of brief motivational techniques for behavioral change. Beneficial outcomes include prevention and control of the serious negative consequences that problematic behaviors have on the health and functioning of older adults.
A high research priority should be given to BAP interventions because these evidence-based behavioral strategies can help patients change health behaviors and affect outcomes. BAP is a practical, effective technique requiring minimal time. The knowledge gained from this pilot study should lead to the development of a randomized controlled design, a larger sample and a longer follow-up period to establish objective, clinically relevant outcomes.
BAP embedded in a health and wellness center provides evidence that it can help advocate for improved, quality care. Community based brief motivational interventions offer a new strategy for improving quality and containing costs while addressing social determinants of health. The effectiveness of community healthcare is related to the collaboration between providers and the community they serve. Improving health behaviors of communities and in particular, vulnerable populations, at a public health level will help mitigate the widespread challenge of the burden of chronic disease.
References
- Martins RK, McNeil DW (2009) Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev 29: 283-293.
- Campbell MK, Carr C, Devellis B, Switzer B, Biddle A, et al. (2009) A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann Behav Med 38: 71-85.
- Berg CJ, Thomas JL, An LC, Guo H, Collins T, et al. (2012) Change in smoking, diet and walking for exercise in blacks. Health Educ Behav 39: 191-197.
- Doyle VC (2007) Nutrition and colorectal cancer risk: A literature review. Gastroenterol Nurs 30: 178-182.
- Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W (2011) Short and long term effects of a lifestyle intervention for construction workers at risk for cardiovascular disease: A randomized controlled trial. BMC Public Health 11: 836.
- Osterman R, Lewis D, Winhusen T (2017) Efficacy of motivational enhancement therapy to decrease alcohol and illicit-drug use in pregnant substance users reporting baseline alcohol use. J Subst Abuse Treat 77: 150-215.
- Hardcastle S, Blake N, Hagger MS (2012) The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J Behav Med 35: 318-333.
- Pel-Littel RE, Schuurmans MJ, Emmelot-Vonk MH, Verhaar HJ (2009) Frailty: defining and measuring of a concept. J Nutr Health Aging 13: 390-394.
- Tse MMY, Vong SKS, Tang SK (2013) Motivational interviewing and exercise programme for community-dwelling older persons with chronic pain: A randomised controlled study. J Clin Nurs 22: 1843-1856.
- Joseph J, Basu D (2016) Efficacy of brief interventions in reducing hazardous or harmful alcohol use in middle-income countries: Systematic review of randomized controlled trials. Alcohol 52: 56-64.
- McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, et al. (2006) How primary care providers talk to patients ab out alcohol: A qualitative study. J Gen Intern Med 21: 966-972.
- Dermen KH, Ciancio SG, Fabiano JA (2014) A pilot test of motivational oral health promotion with alcohol-dependent inpatients. Health Psychol 33: 392-395.
- Perez-Tortosa S, Roig L, Manresa JM, Martin-Cantera C, Puigdomenech E, et al. (2015) Continued smoking abstinence in diabetic patients in primary care: A cluster randomized controlled multicenter study. Diabetes Res Clin Pract 107: 94-103.
- Gutnick D, Reims K, Davis C, Gainforth H, Jay M, et al. (2014) Brief action planning to facilitate behavior change and support patient self-management. J Clin Outcomes Manag 21: 17-29.
- CDC (2016) Chronic diseases: The leading causes of death and disability in the United States, USA.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B (2005) Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract 55: 305-312.
- Ski CF, Thompson DR (2013) Motivational interviewing as a brief intervention to improve cardiovascular health. Eur J Cardiovasc Nurs 12: 226-229.
- Ren Y, Browning C, Yang H, Thomas S (2013) Motivational interviewing and its application in the management of coronary heart disease. Fam Med Community Health 1: 48-54.
- Heckman CJ, Egleston BL, Hofmann MT (2010) Efficacy of motivational interviewing for smoking cessation: A systematic review and meta-analysis. Tob Control 19: 410-416.
- Knight KM, McGowan L, Dickens C, Bundy C (2006) A systematic review of motivational interviewing in physical health care settings. Br J Health Psychol 11: 319-332.
- Rollnick S, Miller WR, Butler C (2008) Motivational interviewing in health care: Helping patients change behavior. New York: Guilford Press, USA.
- Miller W, Rollnick S (2013) Motivational interviewing: Helping people change. New York, NY: Guilford Press, USA.
- Lannon SL (1997) Using a health promotion model to enhance medication compliance. J Neurosci Nurs. 29: 170-178.
- https://deepblue.lib.umich.edu/bitstream/handle/2027.42/85350/HEALTH_PROMOTION_MANUAL_Rev_5-2011.pdf
- Peterson SJ, Bredow TS (2013) Middle Range Theories. Philadelphia, PA: Wolters Kluwer Health/ Lippincott Williams & Wilkins, USA.
- Langer S, Chew-Graham CA, Drinkwater J, Afzal C, Keane K, et al. (2014) A motivational intervention for patients with COPD in primary care: Qualitative evaluation of a new practitioner role. BMC Fam Pract 15: 164.
- Perry CK, Bennett JA (2006) Heart disease prevention in women: Promoting exercise. J Am Acad Nurse Pract 18: 568-573.
- Neuner-Jehle S, Schmid M, Gruninger U (2013) The "Health Coaching" programme: A new patient-centred and visually supported approach for health behaviour change in primary care. BMC Fam Pract 14: 100.
- Purath J, Keck A, Fitzgerald CE (2014) Motivational interviewing for older adults in primary care: a systematic review. Geriatric Nursing 35: 219-224.
- Hayes E, Kalmakis KA (2007) From the sidelines: Coaching as a nurse practitioner strategy for improving health outcomes. J Am Acad Nurse Pract 19: 555-562.
- Letourneau K, Goodman JH (2014) A patient centered approach to addressing physical activity in older adults: Motivational interviewing. J Gerontol Nurs 40: 26-33.
- Cook PF, Emiliozzi S, McCabe MM (2007) Telephone counseling to improve osteoporosis treatment adherence: An effectiveness study in community practice settings. Am J Med Qual 22: 445-456.
- Cummings SM, Cooper RL, Cassie KM (2009) Motivational interviewing to affect behavioral change in older adults. Social Work Practice 19: 195-204.
- Cook P (2006) Psychological interventions to improve medication complicance: A meta-analysis.
- Fontaine G, Cossette S, Heppell S, Boyer L, Mailhot T, et al. (2016) Evaluation of a web-based e-learning platform for brief motivational interviewing by nurses in cardiovascular care: A pilot study. J Med Internet Res 18: e224.
- Butler CC, Simpson SA, Hood K, Cohen D, Pickles T, et al. (2013) Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: A cluster randomized trial. BMJ 346: f1191.
- Katz DA, Stewart K, Paez M, Holman J, Adams SL, et al. (2016) "Let me get you a nicotine patch": Nurses' perceptions of implementing smoking cessation guidelines for hospitalized veterans. Military Medicine 181: 373-382.
- Pullon S, Webster M, McLeod D, Benn C, Morgan S (2004) Smoking cessation and nicotine replacement therapy in current primary maternity care. Aust Fam Physician 33: 94-96.
- Everett-Murphy K, Paijmans J, Steyn K, Matthews C, Emmelin M, et al. (2011) Scolders, carers or friends: South African midwives' contrasting styles of communication when discussing smoking cessation with pregnant women. Midwifery 27: 517-524.
- Whyte RE, Watson HE, McIntosh J (2006) Nurses' opportunistic interventions with patients in relation to smoking. J Adv Nurs 55: 568-577.
- Gance-Cleveland B, Sidora-Arcoleo K, Keesing H, Gottesman MM, Brady M (2009) Changes in nurse practitioners' knowledge and behaviors following brief training on the healthy eating and activity together (HEAT) guidelines. J Pediatr Health Care 23: 222-230.
- Edwards EJ, Stapleton P, Williams K, Ball L (2015) Building skills, knowledge and confidence in eating and exercise behavior change: Brief motivational interviewing training for healthcare providers. Patient Educ Couns 98: 674-676.
- Welch J (2014) Building a foundation for brief motivational interviewing: Communication to promote health literacy and behavior change. J Continuing Edu Nurs 45: 566-572.
- de Almeida Lopes Monteiro da Cruz D, de Mattos Pimenta CA, Pedrosa MF, da Costa Lima AF, Gaidzinski RR (2009) Nurses' perception of power regarding their clinical role. Revista latino-americana de enfermagem 17: 234-239.
- Krishnamurthi R, Witt E, Barker-Collo S, McPherson K, Davis-Martin K, et al. (2014) Reducing recurrent stroke: Methodology of the motivational interviewing in stroke (MIST) randomized clinical trial. Int J Stroke 9: 133-139.
- Miller W (1983) Motivational interviewing with problem drinkers. Behav Psychotherapy 11: 147-172.
- Rejeski WJ, Brawley LR (2006) Functional health: Innovations in research on physical activity with older adults. Med Sci Sports Exerc 38: 93-99.
- Kemp EC, Floyd MR, McCord-Duncan E, Lang F (2008) Patients prefer the method of "tell back-collaborative inquiry" to assess understanding of medical information. J Am Board Fam Med 21: 24-30.
- Dunn C, Deroo L, Rivara FP (2001) The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction 96: 1725-1742.
- Gainforth HL, Latimer-Cheung AE, Davis C, Casemore S, Martin Ginis KA (2015) Testing the feasibility of training peers with a spinal cord injury to learn and implement brief action planning to promote physical activity to people with spinal cord injury. J Spinal Cord Med 38: 515-525.
- Cole S, Davis C, Cole M, Gutnick D (2010) Motivational interviewing and the patient centered medical Home: A strategic approach to self-management support in primary care.
- Benzo R, Vickers K, Ernst D, Tucker S, McEvoy C, et al. (2013) Development and feasibility of a self-management intervention for chronic obstructive pulmonary disease delivered with motivational interviewing strategies. J Cardiopulm Rehabil Prev 33: 113-123.
Citation: Brathwaite BM, Marino MA, Bruckenthal P (2018) Nurse Practitioner Confidence and Attitudes towards Brief Motivational Interventions to Improve Compliance with Health and Wellness Recommendations. J Comm Pub Health Nursing 4: 212. DOI: 10.4172/2471-9846.1000212
Copyright: ©2018 Brathwaite BM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6955
- [From(publication date): 0-2018 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 5918
- PDF downloads: 1037